Podcast
Questions and Answers
What is the most common cause of pulpal disease?
What is the most common cause of pulpal disease?
- Bacterial infection from dental caries (correct)
- Occlusal trauma
- Restorative intervention
- Direct blow to the tooth
Periapical pathology refers to disease occurring around the apex of a tooth.
Periapical pathology refers to disease occurring around the apex of a tooth.
True (A)
Inflammation around the apex of the tooth is termed what?
Inflammation around the apex of the tooth is termed what?
apical periodontitis
Adjacent bone and occasionally the root apex may ____, but healing may occur if the cause of inflammation is removed.
Adjacent bone and occasionally the root apex may ____, but healing may occur if the cause of inflammation is removed.
Match the following terms related to periapical pathology with their descriptions:
Match the following terms related to periapical pathology with their descriptions:
All of the following are factors that may affect Periapical Pathology (PAP) EXCEPT:
All of the following are factors that may affect Periapical Pathology (PAP) EXCEPT:
Healing is very limited in pulpitis cases.
Healing is very limited in pulpitis cases.
What is the term for minor damage to the periodontal ligament and localized inflammation which may be caused by biting unexpectedly on a hard object in food?
What is the term for minor damage to the periodontal ligament and localized inflammation which may be caused by biting unexpectedly on a hard object in food?
Indications for treatment of an acute periapical periodontitis includes closed acute ______.
Indications for treatment of an acute periapical periodontitis includes closed acute ______.
Match the histopathological findings with their definitions:
Match the histopathological findings with their definitions:
Which of the following indicates that a tooth feels elevated in its socket?
Which of the following indicates that a tooth feels elevated in its socket?
Antibiotics are always necessary for apical periodontitis treatment.
Antibiotics are always necessary for apical periodontitis treatment.
The accumulation of acute inflammatory cells at the apex of a nonvital tooth is termed what?
The accumulation of acute inflammatory cells at the apex of a nonvital tooth is termed what?
A localized, purulent form of apical periodontitis is an apical ______.
A localized, purulent form of apical periodontitis is an apical ______.
Match the following terms related to periapical abscess with their definitions:
Match the following terms related to periapical abscess with their definitions:
All of the following are sequelae to acute periapical abscess EXCEPT:
All of the following are sequelae to acute periapical abscess EXCEPT:
Antibiotics are necessary unless concurrent cellulitis is NOT present.
Antibiotics are necessary unless concurrent cellulitis is NOT present.
What is the term for a serious, potentially life-threatening infection, where the face is swollen and the eye is swollen shut?
What is the term for a serious, potentially life-threatening infection, where the face is swollen and the eye is swollen shut?
A periapical abscess appears as a zone of ______.
A periapical abscess appears as a zone of ______.
Match the following sequelae of acute periapical abscess with their descriptions:
Match the following sequelae of acute periapical abscess with their descriptions:
Chronic apical periodontitis is often referred to as:
Chronic apical periodontitis is often referred to as:
In early stages of periapical periodontitis lymphocytes predominate.
In early stages of periapical periodontitis lymphocytes predominate.
Cholesterol crystals and foamy macrophages are features of what type of periapical pathology?
Cholesterol crystals and foamy macrophages are features of what type of periapical pathology?
Non restorable teeth may be extracted, followed by curettage of all apical tissues, with nonsteroidal ______ drugs in symptomatic cases.
Non restorable teeth may be extracted, followed by curettage of all apical tissues, with nonsteroidal ______ drugs in symptomatic cases.
Match following sequelae of PAP:
Match following sequelae of PAP:
Which of the following is the most common cystic lesion in the jaws, always associated with the apex of a non-vital tooth?
Which of the following is the most common cystic lesion in the jaws, always associated with the apex of a non-vital tooth?
Pain is a constant feature of radicular cysts.
Pain is a constant feature of radicular cysts.
Cystic cavity enlargement is secondary to which type of pressure?
Cystic cavity enlargement is secondary to which type of pressure?
Breakdown products of degenerating epithelial cell and ______ cell and connective tissue components are considered cyst contents.
Breakdown products of degenerating epithelial cell and ______ cell and connective tissue components are considered cyst contents.
What is the treatment for a small residual cyst?
What is the treatment for a small residual cyst?
Osteomyelitis is an example of inflammatory diseases of the bone that involves localized inflammation of bone.
Osteomyelitis is an example of inflammatory diseases of the bone that involves localized inflammation of bone.
Localized inflammation of bone is what type of inflammatory bone disease?
Localized inflammation of bone is what type of inflammatory bone disease?
[Blank] is a rare disease due to availability of antibiotics.
[Blank] is a rare disease due to availability of antibiotics.
Match the predisposing factors with their causes:
Match the predisposing factors with their causes:
What is the treatment for acute osteomyelitis?
What is the treatment for acute osteomyelitis?
Focal sclerosing osteitis is described as normal, caries-free teeth.
Focal sclerosing osteitis is described as normal, caries-free teeth.
Odontogenic infections and jaw fractures are the most common cause of what type of bone disease?
Odontogenic infections and jaw fractures are the most common cause of what type of bone disease?
Synonyms for focal sclerosing osteitis are focal sclerosing ______, bony scar, condensing osteitis, and sclerotic bone.
Synonyms for focal sclerosing osteitis are focal sclerosing ______, bony scar, condensing osteitis, and sclerotic bone.
In diffuse sclerosing osteomyelitis are carious non vital teeth often implicated or less often implicated?
In diffuse sclerosing osteomyelitis are carious non vital teeth often implicated or less often implicated?
What type of cells are often missing in florid osseous dysplasia?
What type of cells are often missing in florid osseous dysplasia?
Flashcards
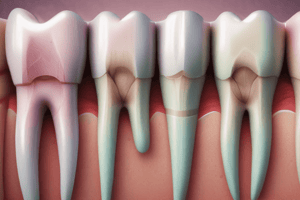
Apical Periodontitis
Apical Periodontitis
Inflammation around the apex of the tooth, bacterial infection caused by dental caries is the most common cause of pulpal disease
Pulpitis
Pulpitis
An infection of the pulp.
Periapical pathology
Periapical pathology
Disease occurring around the apex of a tooth.
PAP are well localized by patient
PAP are well localized by patient
Signup and view all the flashcards
Etiology of periapical periodontitis
Etiology of periapical periodontitis
Signup and view all the flashcards
Acute periapical periodontitis indications
Acute periapical periodontitis indications
Signup and view all the flashcards
Periapical abscess
Periapical abscess
Signup and view all the flashcards
Apical Abscess
Apical Abscess
Signup and view all the flashcards
Histopathology-Microscopically
Histopathology-Microscopically
Signup and view all the flashcards
Acute periapical abscess sequelae
Acute periapical abscess sequelae
Signup and view all the flashcards
Sequelae of PAP
Sequelae of PAP
Signup and view all the flashcards
Chronic apical periodontitis
Chronic apical periodontitis
Signup and view all the flashcards
Periapical granulomas
Periapical granulomas
Signup and view all the flashcards
Prognosis of granuloma
Prognosis of granuloma
Signup and view all the flashcards
Sequelae of PAP
Sequelae of PAP
Signup and view all the flashcards
Radicular cyst
Radicular cyst
Signup and view all the flashcards
Radicular cyst pathogenesis
Radicular cyst pathogenesis
Signup and view all the flashcards
Radicular cyst lining
Radicular cyst lining
Signup and view all the flashcards
Cyst Contents
Cyst Contents
Signup and view all the flashcards
Residual Cysts
Residual Cysts
Signup and view all the flashcards
Radicular cyst treatment
Radicular cyst treatment
Signup and view all the flashcards
Osteitis
Osteitis
Signup and view all the flashcards
Osteomyelitis
Osteomyelitis
Signup and view all the flashcards
Osteomyelitis
Osteomyelitis
Signup and view all the flashcards
Osteomyelitis
Osteomyelitis
Signup and view all the flashcards
Predisposing factors
Predisposing factors
Signup and view all the flashcards
Acute suppurative osteomyelitis
Acute suppurative osteomyelitis
Signup and view all the flashcards
Acute osteomyelitis Symptoms
Acute osteomyelitis Symptoms
Signup and view all the flashcards
Sequestrum
Sequestrum
Signup and view all the flashcards
Involucrum
Involucrum
Signup and view all the flashcards
Acute Osteomyelitis
Acute Osteomyelitis
Signup and view all the flashcards
Chronic osteomyelitis.
Chronic osteomyelitis.
Signup and view all the flashcards
Osteomyelitis. Diagnosis?
Osteomyelitis. Diagnosis?
Signup and view all the flashcards
Focal sclerosing osteitis
Focal sclerosing osteitis
Signup and view all the flashcards
Diffuse sclerosing osteomyelitis
Diffuse sclerosing osteomyelitis
Signup and view all the flashcards
Garre's Osteomyelitis
Garre's Osteomyelitis
Signup and view all the flashcards
Osteoradionecrosis
Osteoradionecrosis
Signup and view all the flashcards
Alveolar osteitis (dry socket)
Alveolar osteitis (dry socket)
Signup and view all the flashcards
Study Notes
Periapical Pathology
- Bacterial infection from dental caries is the most common cause of pulpal disease
Pulpitis
- An infection of the pulp
Periapical Infection (Apical Periodontitis)
- Inflammation around the apex of the tooth in the periapical tissues
Periapical Pathology Definition
- Disease occurring around the apex of a tooth
- Adjacent bone and the root apex may resorb
- Healing may occur if the cause of inflammation is removed
Pathways for Pulp and Periapical Tissue Infections
- Carious cavity
- Gingival crevice
PAP (Periapical Periodontitis) vs Pulpitis
- Healing is very limited in PAP
- PAP is well localized by the patient due to proprioceptive nerve endings in the periodontal ligament
Factors Affecting PAP
- Presence of open or closed pulpitis
- Virulence of involved microorganisms
- Extent of sclerosis of dentinal tubules
- Competency of the host immune response
Etiology of Periapical Periodontitis
- Untreated pulpitis and pulp necrosis
- Occlusal trauma
- Restorative intervention
- Direct blow to a tooth insufficient to cause pulp necrosis
- Unexpected biting on a hard body in food
- Minor damage to the periodontal ligament and localized inflammation
Acute Periapical Periodontitis Treatment Indications
- Young tooth with open tubules
- Rampant caries
- Closed acute pulpitis
- Presence of highly virulent microorganisms
- Weakened host defense system
Histopathological Findings
- Vascular dilation
- Exudates of neutrophils
- Oedema in the periodontal ligament
- Confined space between the root apex and the alveolar bone
Clinical Presentation
- Intense pain when external pressure is applied to the tooth
- Tooth feels elevated in its socket
- Hot and cold stimulation does not cause pain
Sequela and Prognosis
- Resolution can occur if the inflammation is transient and due to acute trauma
- Can become chronic with adjacent bone resorption
- Acute periapical abscess can occur in complicated severe cases
Apical Periodontitis Characteristics
- Inflammation around the apex of the tooth
- Severely inflamed pulp will eventually necrose
- Pain is severe, spontaneous, and persistent, localizing to the affected tooth
- The tooth is sensitive to percussion with a metal object
- Regional lymphadenopathy may be present
- Management is root canal treatment or extraction
- Antibiotics are not always necessary
Acute Periapical Abscess Definition
- Accumulation of acute inflammatory cells at the apex of a nonvital tooth
- Exudates contain potent exotoxins and lytic enzymes that rapidly break down tissue barriers
- Can be caused by the acute exacerbation of a chronic periapical granuloma
- Pus associated with a lesion will seek the path of least resistance
- Jaw tenderness
- Hypersensitivity to tooth percussion
- Possible systemic features
Apical Abscess Characteristics
- Localized, purulent form of apical periodontitis
- Presents clinically as a fluctuant buccal or palatal swelling, with or without draining pus
- Regional adenopathy is usually present
- If pus is draining, pain usually is not severe
- Antibiotics are not necessary unless concurrent cellulitis is present
- Acute incision and drainage of a fluctuant area is needed
- Definitive therapy is root canal treatment or extraction
Periapical Abscess Appearance
- Face is swollen and the eye may be swollen shut
- Represents a potentially life-threatening infection
Histopathology of a Periapical Abscess
- Appears as a zone of liquefaction, composed of pertinacious exudates, necrotic tissue and viable and dead neutrophils (pus)
- Adjacent tissues containing dilated vessels and a neutrophilic infiltrate surround the area of liquefactive necrosis
Sequelae of Acute Periapical Abscess
- Sinus tract following local penetration of overlying periosteum and mucosa
- May extend through the medullary spaces, resulting in osteomyelitis
- May perforate the cortex and spread diffusely through the overlying soft tissue as cellulitis
- Dental abscesses may discharge through the skin and drain via a cutaneous sinus
- Periapical infection can spread to the bloodstream, resulting in systemic symptoms such as fever, lymphadenopathy, and malaise
- Cellulitis
- Ludwig's angina (submental, submandibular, and sublingual spaces)
Periapical Abscess Late Stage Problems
- Oroantral fistula
- Extension to maxillary cavernous sinus area, thrombophlebitis & brain abscess or acute meningitis
Treatment and Prognosis of Periapical Abscess
- Drainage and elimination of the focus of infection is necessary
- Antibiotics if the patient has systemic features or is immunocompromised
- NSAIDs if not contraindicated
- The tooth should be endodontically treated or extracted
- Sinus and fistula tracts should be surgically removed if not treated spontaneously after extraction
Chronic Apical Periodontitis (Periapical Granuloma)
- A mass of chronically or sub acutely inflamed granulation tissue at the apex of a non-vital tooth
- A secondary reaction to the presence of microbial infection in the root canal, with spread of related toxic products into the apical zone
- In the early stages, neutrophils predominate (acute periapical periodontitis)
Granuloma Progression
- Neutrophils activate osteoclasts leading to bone resorption
- With time, chronic inflammatory cells begin to dominate the host response
Lymphocytes Mediators
- Decrease osteoclast activity
- Increase fibroblast & microvasculature
Histopathological Features
- Periapical granulomas consist of inflamed granulation tissue surrounded by a fibrous connective tissue wall
- The central part of the lesion contains foamy macrophages
- Cholesterol crystals may be present surrounded by multinucleated giant cells
- A diffuse infiltrate of lymphocytes and plasma cells, especially when numerous plasma cells are present
Treatment & Prognosis
- Conservative
- Non-restorable teeth may be extracted, followed by curettage of all apical tissues, with non-steroidal anti-inflammatory drugs
- Antibiotics are not recommended unless systemic signs and symptoms are present
- Follow-up at 1-3-6 months and 1-2 years is needed to rule out possible causes of failure
- All tissues should be submitted for histopathological examination to exclude more serious conditions, like neoplastic process
Sequelae of PAP
- Periapical granuloma enlargement with more bone resorption
- Acute exacerbation to acute periapical periodontitis
- Suppuration to form an acute periapical abscess
- Formation of a radicular cyst
- Low-grade irritation may cause osteosclerosis (bone apposition) or cementum apposition (hypercementosis)
Radicular Cyst Definition
- Apical radicular cysts are the most common cystic lesions in the jaws
- Always associated with the apex of non-vital teeth
- Makes up 75% of all radicular cysts
- Pain is seldom a feature unless there is an acute exacerbation that could lead to abscess formation
- Cysts can rise at any age after tooth eruption, but are rare in deciduous dentition
Radicular Cyst Appearance
- Apical radicular cysts are the most common cystic lesions in the jaws and are always associated with non vital teeth
- Makes up 75% of all radicular cysts
- Small... asymptomatic & discovered accidentally in radiography
- May form a sinus
- Can grow to a large size (uncommon) about 5mm diameter/year
- May perforate the cortex and present as a bluish fluctuant sub mucosal swelling
- Pain is seldom a feature unless there is an acute exacerbation that can lead to abscess formation
- Can be seen at any age (rare in deciduous dentition)
Radicular Cyst Pathogenesis
- Inflammation (usually associated with dental caries extending into the dental pulp or trauma) stimulates cells in the rests of Malassez
- Epithelial cells proliferate to form a cystic cavity
- Cystic cavity can enlarge secondary to:
- Osmotic pressure
- Secondary infection and inflammation related to foreign material or bacteria
- Ongoing inflammation and proinflammatory cytokines (IL-1 & IL-6)
- Osteoclastic resorption of surrounding bone
- The mechanism by which an epithelial lined cyst cavity forms within granulomas is unclear.
Two main mechanisms include:
- Degeneration and death of central cells within a proliferating mass of epithelium that outgrows its blood supply
- Degeneration and liquefactive necrosis of granulation tissue where epithelial proliferation surrounds the area of necrosis
Radicular Cyst Microscopic Presentation
- Lined by nonkeratinizing stratified squamous epithelium of variable thickness which creates an arcading pattern
- Fibrous capsule of varying thickness with acute or chronic inflammatory cells
- May have plasma cells or foamy histiocytes
- May contain cholesterol clefts, bacterial colonies, foreign material related to prior dental treatments, portions of bone/tooth/tooth root, or regional odontogenic rests and neural tissue
Cyst Contents
- Vary from a watery straw color fluid through to semi-solid brownish material
- Cholesterol crystals impart a shimmering appearance
- Complex composition, hypertonic compared with serum
- Contains breakdown products of degenerating epithelial cells and inflammatory cells/connective tissue components
- Serum proteins are present in cyst fluid and are derived as inflammatory exudates
- The fluid contains a higher level of immunoglobulin than serum
- Water and electrolytes
- Cholesterol crystals
Residual Cysts
- Radicular cysts remaining after the tooth has been extracted
- Usually asymptomatic
- Usually small size (less than 1 cm in diameter)
- Unilocular, round or oval, well-defined, usually well-corticated
- Can cause bone expansion and displacement of adjacent teeth
Treatment of Radicular Cysts
- If the tooth is restorable, root canals are filled
- Apicoectomy with complete surgical enucleation
- Tooth can be extracted and the periapical cyst is curated
Inflammatory Bone Diseases
- Categorized based on the extent of involvement of the bone
- Osteitis
- Localized inflammation of bone that does not involve marrow spaces
- Associated with infected sockets following removal of teeth
- Osteomyelitis
- Extensive bone involvement extending through the marrow spaces
- Periostitis
- Inflammation of the periosteal spaces of the bone
- May not be associated with osteomyelitis
Osteomyelitis Today
- Rare due to availability of antibiotics
- Various clinical subtypes depending on the nature/severity of the irritant, host defense, and predisposing factors - Acute - Chronic - Suppurative - Sclerotic
- Most cases are bacterial infections with expanding lytic destruction of involved bone, suppuration, and sequestra formation
- Can be called suppurative osteomyelitis, bacterial osteomyelitis, or secondary osteomyelitis
- Idiopathic inflammatory disorder that demonstrates sclerosis of bone(without suppuration or sequestra formation) that does not respond consistently to antibacterial medications
Osteomyelitis Locations
- Primary Chronic Osteomyelitis (Diffuse Sclerosing Osteomyelitis)
- Focal Sclerosing Osteomyelitis
- Proliferative periostits
- Alveolar osteitis
- Suppurative Osteomyelitis is uncommon in developed nations, but remains a difficulty in developing nations
- The most common cause is odontogenic infections and jaw fractures
- In Africa, an important cause is acute necrotizing gingivitis
Osteomyelitis Predisposing Factors
- Chronic systemic diseases, immunocompromised status, and disorders associated with decreased vascularity of bone
- Tobacco/Alcohol/IV Drug Abuse
- Diabetes Mellitus
- Exanthematous fever and malaria
- Sickle cell anemia
- Malnutrition
- Malignancy
- Collagen vascular disease
- AIDS
- Radiation
- Osteopetrosis, dysosteosclerosis, pagets disease, end-stage cemento-osseous dysplasia may result in hypovascularized bone that is predisposed to necrosis and inflammation
Acute Suppurative Osteomyelitis
- Inflammation spreads through the medullary spaces & insufficient time has passed for the body to react to the presence of the inflammatory infiltrate
Chronic Suppurative Osteomyelitis
- Body response (granulation tissue) forms dense scar tissue that walls off infected area
- Encircled dead space acts as a reservoir for bacteria, so antibiotics are difficult to reach the site
- Starts one month after spread of acute infection, progressive & needs aggressive treatment
Acute Osteomyelitis Signs
- Signs and symptoms of an acute inflammatory process lasting less than 1 month
- Fever, leukocytosis, lymphadenopathy, significant sensitivity and soft tissue swelling of the affected area may be present
Osteomyelitis Radiographic Features
- Early stages may be unremarkable or may demonstrate an ill-defined radiolucency
- Paresthesia of the lower lip may occur with drainage or exfoliation of fragments of necrotic bone
- A fragment of necrotic bone that has separated from the adjacent vital bone is termed a sequestrum
- Fragments of necrotic bone may become surrounded by vital bone, such that the mass of encased nonvital bone is called an involucrum
Acute Osteomyelitis
- Infection of jaw bone may result from untreated pulpal and/or periapical infection
- It is a very serious condition that can cause destruction of large sections of the jaw & be difficult to cure.
Chronic Osteomyelitis Features
- Follows acute osteomyelitis that is not resolved or occurs primarily without a previous acute episode.
- There may be swelling, pain, sinus formation, purulent discharge, sequestrum formation, tooth loss, or pathologic fracture.
- Patients may experience acute exacerbation or periods of decreased pain associated with chronic smoldering progression.
- Sequestra, and Osteogenic periosteal hyperplasia can be found on radiographs
Chronic Osteomyelitis Pathogenesis
- Because of a particular arrangement, large portions of each jawbone receive their blood supply through multiple arterial loops originating from a single vessel. Involvement of this single feeder vessel can lead to necrosis of a large portion of the affected bone.
Osteomyelitis Histopathologic Features - Acute
- Biopsy material is not common because of liquid content and lack of soft-tissue component.
- Material consists predominantly of necrotic bone.
- Bacterial colonization, and Acute inflammatory infiltrate consisting of polymorphonuclear leukocytes may be confused with sequestrum unless a good clinicopathologic correlation.
Osteomyelitis Histopathologic Features - Chronic
- Significant soft tissue component that consists of chronically/sub acutely inflamed fibrous connective tissue filling the intertrabecular areas of the bone.
- Scattered sequestra and pockets of abscess formation are common
Acute Osteomyelitis Treatment and Prognosis
- If an abscess is present, drainage and antibiotics are needed as it is a mixed microbial infection
- Antibiotics of choice are Penicillin, clindamycin, cephalexin, cefotaxime, tobramycin, and gentamicin
- Antibiotic therapy can sterilize the sequestra, non vital bone fragments should be allowed to remain to allow for future bone development
Chronic Osteomyelitis Treatment and Management
- Management is difficult due to pockets of dead bone and organisms being protected from antibiotics by surrounding wall of fibrous connective tissue
- AB: intravenously in high doses
- Surgical intervention is mandatory. Decortications/saucerization is combined with a cancellous bone chips transplant
- Resection of diseased bone (followed by immediate reconstruction with an autologous graft)
- Weakened jawbones must be immobilized
- Adjunctive procedures (hyperbaric oxygen) are rarely used
Focal Sclerosing Osteitis Characteristics
- Common
- Focal bony reaction to low-grade inflammatory stimulus
- Usually seen at apex of tooth with long-standing pulpitis
- Synonyms are focal sclerosing osteomyelitis, bony scar, condensing osteitis, and sclerotic bone
- Focal periapical osteopetrosis describes idiopathic lesions associated with normal, caries-free teeth
- Asymptomatic, mostly discovered on radiographs
- Bone lesions are:
- Uniformly opaque
- Peripheral lucency with opaque center
- Opaque periphery with a lucent center
- Confluent/lobulated opaque masses
- Masses of dense sclerotic bone that have very few inflammatory cells and scant connective tissue
- There is believed to be a physiologic bone reaction to a known stimulus, and the lesion itself is not removed
- It is important to rule out more significant lesions, the inflamed pulp that stimulated the focal sclerosing osteomyelitis should be treated
Diffuse Sclerosing Osteomyelitis
- Ill-defined clinical entity that is an inflammatory reaction in the mandible/maxilla believe to be in response to low virulent organism
- Bacteria are generally suspected but are seldom specifically identified
- Chronic periodontal disease can be a portal of entry for bacteria, and is important in the etiology/progression
- Teeth with non-vital caries are less often implicated in this disease
Histology Findings in Diffuse Sclerosing Osteomyelitis
- Bone sclerosis/remodeling
- Scanty marrow spaces
- Necrotic bone separates from vital bone to be surrounded by tissue
- Secondary bacterial colonization
Differential Diagnosis of Diffuse Sclerosing Osteomyelitis
- Florid osseous dysplasia exhibits anterior periapical lesions/traumatic/simple bone cysts
- Florid osseous dysplasia is asymptomatic and appears as a fibroosseous lesion lacking inflammatory cell infiltrate
- Treatment
- Problematic due to large size of lesions, Remove cause, and Antibiotics/Low-dose corticosteroids, (Antibiotics are less effective)
- Surgeries are inappropriate to due extent
- Hyperbaric oxygen therapy/Pamidronate
Chronic Osteomyelitis with Proliferative Periostitis (Garré's Osteomyelitis)
- Uncommon infection - a chronic osteomyelitis with subperiosteal bone and collagen deposition/prominent periosteal inflammatory reaction
- Results from a periapical abscess of a mandibular molar tooth
- Can be caused by infection associated with tooth extraction or partially erupted molars
- Most common in children
- Radiographs and a biopsy provides a definitive diagnosis
- Described in the tibia & the head and neck area- Radiographs and a biopsy provides a definitive diagnosis
- Body of mandible
- Reactive new bone typified by parallel orientation of new trabeculae under low magnification
- Osteoblasts and osteoclasts are seen centrally along the trabeculae
- Scattered lymphocytes and plasma cells
- There is no inflammatory cells, so difficult to differentiate from fibrodysplasia
Histopathology
- Reactive new bone typified by parallel rows of highly cellular and reactive woven bone
- Between trabecular, uninflamed fibrous tissue Identification of and treatment of the tooth/extraction of the involved tooth
Osteoradionecrosis
- One of the most serious complications of radiation
- Bone irradiation results in damage to the osteocytes and microvasculature system
- The affected bone becomes hypoxic, hypovascular, and hypocellular
- Bone is nonhealing dead bone, though infection is not necessarily present
- Bisphosphonates are used for patients with multiple myeloma, metastatic cancers, Paget's disease, and osteoporosis
- Inhibitory effect on osteoclastic bone resorption, and can occur through tooth extraction
Alveolar Osteitis (Dry Socket; Fibrinolytic Alveolitis)
- Alveolar process of maxilla or mandible
- Occurs after tooth extraction, as a postoperative complication -1% - 3% of all extractions. Average is 20-40 years old
- After tooth extraction, a blood clot occurs, made of granulation tissue, coarse fibrillar bone, and organized mature bone eventually.
Alveolar Osteitis (Dry Socket; Fibrinolytic Alveolitis) Predisposing Factors
- Experience
- Traumatic extractions
- Oral contraceptive
- Presurgical infections
- Inadequate irrigation at surgery
- Smoking
Alveolar Osteitis (Dry Socket; Fibrinolytic Alveolitis) Signs and Symptoms
- Severe pain and foul odour that develops 3-4 days after extraction
- Swelling and lymphadenopathy
- Symptoms last 10-40 days
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.