Podcast
Questions and Answers
What is the primary function of the endopelvic fascia in the pelvis?
What is the primary function of the endopelvic fascia in the pelvis?
- It forms a rigid structure to prevent movement of organs.
- It acts as a connective tissue that supports pelvic organs. (correct)
- It serves as a primary source of blood supply to the pelvic organs.
- It provides an elastic layer around the pelvic cavity.
Which of the following structures is associated with supporting the anterior vaginal wall?
Which of the following structures is associated with supporting the anterior vaginal wall?
- Rectovaginal fascia/septum
- Cardinal ligament
- Thickened fascia of the pubocervical ligament
- Urethrovaginal fascia/septum (correct)
How do thickened areas of the endopelvic fascia contribute to pelvic support?
How do thickened areas of the endopelvic fascia contribute to pelvic support?
- They are responsible for the transmission of nerve signals.
- They provide additional strength and support in specific areas. (correct)
- They restrict movement of pelvic organs during activities.
- They allow for more flexibility in the pelvic structure.
What role do the discrete ligaments play in the pelvic structure?
What role do the discrete ligaments play in the pelvic structure?
The pubocervical ligament is associated with which of the following structures?
The pubocervical ligament is associated with which of the following structures?
What is the significance of the axial section of the pelvis mentioned in the context?
What is the significance of the axial section of the pelvis mentioned in the context?
Which layer is considered the main packing material in the pelvis?
Which layer is considered the main packing material in the pelvis?
In relation to pelvic support, what is the primary role of ligaments such as the cardinal ligaments?
In relation to pelvic support, what is the primary role of ligaments such as the cardinal ligaments?
What is the anatomical relationship described as 'water under the bridge' in relation to the uterine artery and ureter?
What is the anatomical relationship described as 'water under the bridge' in relation to the uterine artery and ureter?
Which structures primarily provide support to the uterus?
Which structures primarily provide support to the uterus?
At which level is the broad ligament positioned relative to the uterus?
At which level is the broad ligament positioned relative to the uterus?
Which ligaments are primarily responsible for pulling the uterine cervix and upper vagina posteriorly?
Which ligaments are primarily responsible for pulling the uterine cervix and upper vagina posteriorly?
What is a significant consideration when ligating the uterine artery during a surgical procedure?
What is a significant consideration when ligating the uterine artery during a surgical procedure?
What is the primary function of the pubocervical ligament?
What is the primary function of the pubocervical ligament?
Which ligament is primarily responsible for maintaining the anteverted and anteflexed position of the uterus?
Which ligament is primarily responsible for maintaining the anteverted and anteflexed position of the uterus?
What classification system describes the support structures of the pelvic floor?
What classification system describes the support structures of the pelvic floor?
What type of prolapse occurs due to weakness in the urethrovaginal septum?
What type of prolapse occurs due to weakness in the urethrovaginal septum?
What anatomical structure is involved in the anterior vaginal wall prolapse?
What anatomical structure is involved in the anterior vaginal wall prolapse?
Which ligaments provide support to the upper part of the vagina?
Which ligaments provide support to the upper part of the vagina?
In pelvic support levels, what does Level 3 primarily support?
In pelvic support levels, what does Level 3 primarily support?
What type of uterine position is defined by the anterior tilting of the uterine body in relation to the cervix?
What type of uterine position is defined by the anterior tilting of the uterine body in relation to the cervix?
How does the rectovaginal septum contribute to pelvic support?
How does the rectovaginal septum contribute to pelvic support?
What condition results from weakness in the rectovaginal septum?
What condition results from weakness in the rectovaginal septum?
The broad ligament reflects from the posterior pelvic wall to which structure?
The broad ligament reflects from the posterior pelvic wall to which structure?
Which condition involves a combination of anterior and posterior vaginal wall prolapses?
Which condition involves a combination of anterior and posterior vaginal wall prolapses?
Which of the following describes the condition where the rectum protrudes through the vaginal wall?
Which of the following describes the condition where the rectum protrudes through the vaginal wall?
What is the anatomical significance of the perineal body in pelvic support?
What is the anatomical significance of the perineal body in pelvic support?
Flashcards are hidden until you start studying
Study Notes
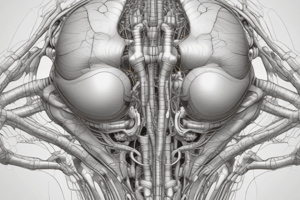
Overview of Pelvic Support Structures
- Pelvic diaphragm functions as a supportive structure, compared to a ship in the berth.
- Ligaments and fascia serve as key support systems, analogous to ropes maintaining tension and stability.
Connective Tissue and Endopelvic Fascia
- The endopelvic fascia, composed of collagen and elastic fibers, connects pelvic organs to the pelvic walls and floor.
- Acts as a packing material in the pelvis, adapting during development to provide support.
- Distinct membranes and discrete ligaments cover the pelvic walls, enhancing structural integrity.
Ligamentous and Membranous Support
- Key ligaments include Pubovesical and Pubocervical ligaments, providing structure to the bladder and urethra.
- Urethrovaginal fascia supports the anterior vaginal wall, while the Rectovaginal fascia supports the rectum.
- Uterosacral ligaments aid in maintaining the anteverted position of the uterus.
Uterine Positioning
- Anteversion: Anterior tilt of the uterine cervix relative to the vagina.
- Anteflexion: Anterior tilt of the uterine body in relation to the cervix.
- Variations of retroversion and retroflexion also exist.
Delancey’s Classification of Connective Tissue Support
- Level 1: Supports cervix and upper vagina; includes Cardinal and Uterosacral ligaments.
- Weakness results in utero-vaginal prolapse.
- Level 2: Provides support to the middle vagina; includes Endopelvic fascia and Rectovaginal septum.
- Weakness leads to anterior (Cystocele) and posterior (Rectocele) vaginal prolapses.
- Level 3: Supports the lowest part of the vagina; involves the Perineal body and membranes.
- Weakness can cause anterior and posterior vaginal wall prolapses.
Types of Vaginal Prolapses
- Urethrocoele: Prolapse of the urethra in the anterior wall.
- Cystocoele: Prolapse of the bladder in the anterior wall.
- Rectocoele: Prolapse of the rectum in the posterior wall.
- Enterocoele: Prolapse involving the intestine.
- Uterovaginal prolapse: Involves all aspects of urogenital prolapse.
Broad Ligament and Peritoneal Folds
- The broad ligament encompasses the peritoneum reflecting off pelvic structures, creating a pathway from the posterior pelvic wall to the bladder.
Summary
- Structural integrity of the pelvis is maintained through a combination of ligaments, fascia, and connective tissues.
- Understanding these supports and their classifications is crucial for recognizing potential pelvic disorders and prolapse issues.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.