Podcast
Questions and Answers
What is the purpose of the scene size up in patient assessment?
What is the purpose of the scene size up in patient assessment?
- To evaluate the environment for safety and identify potential hazards (correct)
- To take vital signs immediately
- To administer first aid to the patient
- To determine the patient's medical history
Which assessment follows the primary assessment in patient evaluation?
Which assessment follows the primary assessment in patient evaluation?
- Scene size up
- Detailed physical exam
- Focused history and physical exam (correct)
- Ongoing assessment
What does the acronym ABC stand for in patient assessment?
What does the acronym ABC stand for in patient assessment?
- Airway, Body, Care
- Airway, Breathing, Circulation (correct)
- Assessment, Breathing, Control
- Alertness, Breathing, Circulation
What does the OPQRST acronym help assess in a patient?
What does the OPQRST acronym help assess in a patient?
What should be done if a patient's airway is not patent?
What should be done if a patient's airway is not patent?
What is considered a normal adult pulse rate range?
What is considered a normal adult pulse rate range?
Which of the following indicates a life-threatening condition that requires immediate action?
Which of the following indicates a life-threatening condition that requires immediate action?
In the SAMPLE acronym, what does the 'L' stand for?
In the SAMPLE acronym, what does the 'L' stand for?
Flashcards
Scene Size Up
Scene Size Up
Initial assessment of the scene to ensure safety and identify patient needs. This includes assessing overall scene safety, the number and location of patients, and the mechanism of injury/nature of incident.
Primary Assessment
Primary Assessment
Fast initial assessment of the patient focusing on life-threatening conditions. This involves checking responsiveness, breathing, circulation, and any immediate concerns, like severe bleeding.
AVPU
AVPU
A method to assess a patient's responsiveness. (Alert, Verbal, Pain, Unresponsive)
ABCs (Airway, Breathing, Circulation)
ABCs (Airway, Breathing, Circulation)
Signup and view all the flashcards
MOI/NOI
MOI/NOI
Signup and view all the flashcards
Pain Assessment (OPQRST)
Pain Assessment (OPQRST)
Signup and view all the flashcards
C-Spine Precautions
C-Spine Precautions
Signup and view all the flashcards
Patient Priority & Transport
Patient Priority & Transport
Signup and view all the flashcards
Study Notes
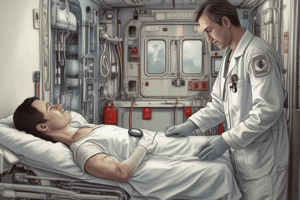
Patient Assessment
-
Scene Size Up: Assess the scene for safety, number of patients, mechanism of injury (MOI) / nature of illness (NOI), and potential spinal injuries (C-spine). Secure the scene and ensure personnel safety.
-
Primary Assessment: A rapid initial evaluation of the patient's condition, prioritizing life-threatening issues;
- General Impression: Observe the patient's appearance and behavior.
- AVPU: Alert, Verbal, Pain, Unresponsive (used to quickly assess responsiveness)
- Chief Complaint (C/C): Determine the patient's primary concern.
- Life Threats: Identify and address any immediate concerns (e.g., airway obstruction, severe bleeding).
- Consent: Obtain appropriate consent for treatment.
- Expose (necessary): Remove clothing for a comprehensive assessment, if safe and possible.
- Transport Priority: Determine the appropriate transport category and speed based on needs:
- Rapid Transport (life-threatening)
- Prompt Transport (generally needed, as needed)
- Regular Transport (no immediate life-threatening issues, obeying traffic laws).
-
Focused History and Physical Exam: Collect detailed information about the patient's past health, taking into account the MOI/NOI, followed by a thorough examination.
-
Detailed Physical Exam: Follow up on the focused exam with a further detailed examination of the patient.
ABCs
-
Airway: Evaluate airway patency (open and clear). If open, maintain with head tilt-chin lift. If obstructed, clear with suction and use an OPA/NPA.
-
Breathing: Assess respirations—rate (12-20), rhythm (regular/irregular), and quality (labored, constricted, wheezing). Monitor SpO2 (target 95-100%). Administer supplemental oxygen as needed (nasal cannula, non-rebreather, BVM-most to least).
-
Circulation: Check pulse rate (adult 60-100, child 70-150, infant 100-160), rhythm (regular/irregular/irregularly irregular), quality (strong, weak, thready, bounding). Assess capillary refill (2-3 seconds). Monitor blood glucose (70-130), skin condition (pink, warm, dry), and blood pressure (100-120/60-80).
Assessment Tools
-
OPQRST: Used for pain assessment: Onset, Provocation, Quality, Region/Radiation, Severity, and Timing.
-
DCAP-BTLS: Useful for identifying injuries: Deformities, Contusions, Abrasions, Punctures, Burns, Tenderness, Lacerations, Swelling.
-
SAMPLE: A useful method of gathering history: Signs and Symptoms, Allergies, Medications, Past pertinent medical history, Last oral intake, Events leading up to the injury.
Additional Notes
- BSI: Standard precautions for infection control/prevention.
- MOI/NOI: Mechanism of injury/nature of illness - crucial for understanding the patient's condition and directing treatment.
- C-spine precautions: If any possibility of spinal injury, immobilize the patient's head until spinal board is in place.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers essential patient assessment techniques including scene size up and primary assessment. It emphasizes the importance of quickly identifying life-threatening issues and effectively communicating with the patient. Test your knowledge on prioritizing transport and obtaining consent during emergencies.