Podcast
Questions and Answers
What is the primary mechanism by which loop diuretics inhibit sodium and chloride reabsorption?
What is the primary mechanism by which loop diuretics inhibit sodium and chloride reabsorption?
- Inhibition of Na+/Ca2+ exchange
- Activation of Na+/H+ exchange
- Direct inhibition of aldosterone
- Inhibition of Na+/K+/2Cl— co-transport system (correct)
Which of the following diuretics is known to cause an increase in the excretion of calcium and magnesium?
Which of the following diuretics is known to cause an increase in the excretion of calcium and magnesium?
- Thiazide diuretics
- Potassium-sparing diuretics
- Carbonic anhydrase inhibitors
- Loop diuretics (correct)
What is a potential complication of using carbonic anhydrase inhibitors like acetazolamide?
What is a potential complication of using carbonic anhydrase inhibitors like acetazolamide?
- Respiratory alkalosis
- Hypophosphatemia
- Hyperkalemia
- Metabolic acidosis (correct)
Which pharmacological effect is NOT associated with loop diuretics?
Which pharmacological effect is NOT associated with loop diuretics?
What therapeutic application is NOT indicated for loop diuretics?
What therapeutic application is NOT indicated for loop diuretics?
Which of the following statements about the pharmacokinetics of loop diuretics is incorrect?
Which of the following statements about the pharmacokinetics of loop diuretics is incorrect?
What is the role of prostaglandins in the action of loop diuretics?
What is the role of prostaglandins in the action of loop diuretics?
How do non-steroidal anti-inflammatory drugs (NSAIDs) affect the efficacy of loop diuretics?
How do non-steroidal anti-inflammatory drugs (NSAIDs) affect the efficacy of loop diuretics?
What is a common adverse effect associated with loop diuretics?
What is a common adverse effect associated with loop diuretics?
Which of the following conditions is most likely prevented by using lower doses of loop diuretics?
Which of the following conditions is most likely prevented by using lower doses of loop diuretics?
What is the primary mechanism through which loop diuretics lower plasma volume?
What is the primary mechanism through which loop diuretics lower plasma volume?
Which thiazide is classified as a true thiazide?
Which thiazide is classified as a true thiazide?
Which of the following is a potential outcome of using loop diuretics at very high doses?
Which of the following is a potential outcome of using loop diuretics at very high doses?
What distinguishes thiazide diuretics from loop diuretics in terms of absorption?
What distinguishes thiazide diuretics from loop diuretics in terms of absorption?
What is a significant risk associated with the concurrent use of loop diuretics and other ototoxic drugs?
What is a significant risk associated with the concurrent use of loop diuretics and other ototoxic drugs?
Why might hyponatremia affect the vascular smooth muscles' sensitivity to catecholamines?
Why might hyponatremia affect the vascular smooth muscles' sensitivity to catecholamines?
Which factor primarily causes edema in congestive heart failure (CHF)?
Which factor primarily causes edema in congestive heart failure (CHF)?
What is a direct consequence of liver cirrhosis in relation to edema?
What is a direct consequence of liver cirrhosis in relation to edema?
In nephrotic syndrome, what primarily leads to edema formation?
In nephrotic syndrome, what primarily leads to edema formation?
Which type of diuretic directly acts on the distal convoluted tubule (DCT)?
Which type of diuretic directly acts on the distal convoluted tubule (DCT)?
What is the mechanism by which osmotic diuretics promote diuresis?
What is the mechanism by which osmotic diuretics promote diuresis?
Which agent is classified as a loop diuretic?
Which agent is classified as a loop diuretic?
How does digitalis lead to increased renal blood flow (RBF) in congestive heart failure?
How does digitalis lead to increased renal blood flow (RBF) in congestive heart failure?
What is the primary function of natriuretic diuretics?
What is the primary function of natriuretic diuretics?
What is the primary mechanism of action of thiazides in the renal system?
What is the primary mechanism of action of thiazides in the renal system?
In what condition are thiazides generally ineffective?
In what condition are thiazides generally ineffective?
Which electrolyte disturbance is commonly associated with thiazide use?
Which electrolyte disturbance is commonly associated with thiazide use?
What paradoxical effect can thiazides have in patients with nephrogenic diabetes insipidus?
What paradoxical effect can thiazides have in patients with nephrogenic diabetes insipidus?
Which of the following is NOT an adverse effect of thiazide diuretics?
Which of the following is NOT an adverse effect of thiazide diuretics?
What is the therapeutic use of thiazides in relation to hypercalcuria?
What is the therapeutic use of thiazides in relation to hypercalcuria?
Thiazides can cause which metabolic disturbance in relation to potassium levels?
Thiazides can cause which metabolic disturbance in relation to potassium levels?
Which statement best describes the efficacy of thiazides?
Which statement best describes the efficacy of thiazides?
Loop diuretics can lead to a loss of potassium due to their effect on Na+/K+/2Cl― co-transport system.
Loop diuretics can lead to a loss of potassium due to their effect on Na+/K+/2Cl― co-transport system.
Carbonic anhydrase inhibitors like acetazolamide cause a significant increase in bicarbonate reabsorption.
Carbonic anhydrase inhibitors like acetazolamide cause a significant increase in bicarbonate reabsorption.
Bumetanide is absorbed more erratically compared to furosemide.
Bumetanide is absorbed more erratically compared to furosemide.
Loop diuretics enhance renal blood flow (RBF) through increased production of prostaglandins.
Loop diuretics enhance renal blood flow (RBF) through increased production of prostaglandins.
Transudative edema is primarily caused by decreased oncotic pressure resulting from hypoalbuminemia.
Transudative edema is primarily caused by decreased oncotic pressure resulting from hypoalbuminemia.
Diuretics can effectively treat edema caused by lymphatic obstruction.
Diuretics can effectively treat edema caused by lymphatic obstruction.
Acetazolamide is primarily used to decrease intraocular pressure in patients with glaucoma.
Acetazolamide is primarily used to decrease intraocular pressure in patients with glaucoma.
Loop diuretics, such as furosemide, act on the distal convoluted tubule (DCT) to promote diuresis.
Loop diuretics, such as furosemide, act on the distal convoluted tubule (DCT) to promote diuresis.
The diuresis effect of loop diuretics occurs after 60 minutes of oral administration.
The diuresis effect of loop diuretics occurs after 60 minutes of oral administration.
In nephrotic syndrome, excessive loss of plasma proteins leads to increased plasma oncotic pressure and subsequent edema.
In nephrotic syndrome, excessive loss of plasma proteins leads to increased plasma oncotic pressure and subsequent edema.
Loop diuretics can cause increased excretion of calcium and magnesium along with sodium and potassium.
Loop diuretics can cause increased excretion of calcium and magnesium along with sodium and potassium.
Renal diuretics directly affect the kidneys, while extra-renal diuretics indirectly induce diuresis through mechanisms such as increased water intake.
Renal diuretics directly affect the kidneys, while extra-renal diuretics indirectly induce diuresis through mechanisms such as increased water intake.
Spironolactone is classified as a loop diuretic due to its action in the ascending limb of the loop of Henle.
Spironolactone is classified as a loop diuretic due to its action in the ascending limb of the loop of Henle.
Congestive heart failure (CHF) causes renal ischemia, which stimulates the renin-angiotensin-aldosterone system (RAAS) leading to fluid retention.
Congestive heart failure (CHF) causes renal ischemia, which stimulates the renin-angiotensin-aldosterone system (RAAS) leading to fluid retention.
Osmotic diuretics increase the osmotic pressure of tubular fluid, preventing water reabsorption and leading to increased urine output.
Osmotic diuretics increase the osmotic pressure of tubular fluid, preventing water reabsorption and leading to increased urine output.
In patients with liver cirrhosis, increased plasma oncotic pressure due to the synthesis of excessive albumin can cause fluid accumulation in the peritoneal cavity.
In patients with liver cirrhosis, increased plasma oncotic pressure due to the synthesis of excessive albumin can cause fluid accumulation in the peritoneal cavity.
Acute renal failure necessitates the maintenance of adequate GFR and enhances K+ excretion.
Acute renal failure necessitates the maintenance of adequate GFR and enhances K+ excretion.
Thiazide diuretics produce their effect within 4–5 hours after administration.
Thiazide diuretics produce their effect within 4–5 hours after administration.
Hyperuricemia due to loop diuretics is primarily caused by decreased uric acid reabsorption in the PCT.
Hyperuricemia due to loop diuretics is primarily caused by decreased uric acid reabsorption in the PCT.
Ototoxicity from loop diuretics is less frequent in patients without impaired renal function.
Ototoxicity from loop diuretics is less frequent in patients without impaired renal function.
Hypokalemic metabolic alkalosis can occur due to decreased tubular secretion of K+ and H+.
Hypokalemic metabolic alkalosis can occur due to decreased tubular secretion of K+ and H+.
Ethacrynic acid is a thiazide diuretic that falls under the category of true thiazides.
Ethacrynic acid is a thiazide diuretic that falls under the category of true thiazides.
Electrolyte disturbances from diuretics can include hypokalemia and hypomagnesemia.
Electrolyte disturbances from diuretics can include hypokalemia and hypomagnesemia.
All loop diuretics, except ethacrynic acid, are derivatives of sulfonamides and can cause allergic reactions.
All loop diuretics, except ethacrynic acid, are derivatives of sulfonamides and can cause allergic reactions.
Thiazides can exacerbate conditions of renal failure due to their ineffectiveness when GFR is below 30-40 ml/min.
Thiazides can exacerbate conditions of renal failure due to their ineffectiveness when GFR is below 30-40 ml/min.
Thiazides inhibit the Na+/Cl― co-transport system in the distal convoluted tubule (DCT) leading to increased reabsorption of Na+ and Cl―.
Thiazides inhibit the Na+/Cl― co-transport system in the distal convoluted tubule (DCT) leading to increased reabsorption of Na+ and Cl―.
Thiazides have a significant antidiuretic action in managing nephrogenic diabetes insipidus by improving ADH receptor sensitivity.
Thiazides have a significant antidiuretic action in managing nephrogenic diabetes insipidus by improving ADH receptor sensitivity.
The maximum excretion load for thiazides is always more than 8% of the filtered Na+.
The maximum excretion load for thiazides is always more than 8% of the filtered Na+.
Thiazides are less effective in treating essential hypertension compared to loop diuretics.
Thiazides are less effective in treating essential hypertension compared to loop diuretics.
Thiazide use can lead to hypokalemic metabolic alkalosis due to increased secretion of potassium and hydrogen ions.
Thiazide use can lead to hypokalemic metabolic alkalosis due to increased secretion of potassium and hydrogen ions.
Thiazides enhance excretion of calcium (Ca2+) in the kidneys.
Thiazides enhance excretion of calcium (Ca2+) in the kidneys.
Hypovolemia and hypotension are not common adverse effects associated with thiazide diuretics.
Hypovolemia and hypotension are not common adverse effects associated with thiazide diuretics.
What is the role of carbonic anhydrase inhibitors in the prevention of metabolic acidosis?
What is the role of carbonic anhydrase inhibitors in the prevention of metabolic acidosis?
How do loop diuretics lead to rapid diuresis after intravenous administration?
How do loop diuretics lead to rapid diuresis after intravenous administration?
What impact do NSAIDs have on the effectiveness of loop diuretics?
What impact do NSAIDs have on the effectiveness of loop diuretics?
In what way do loop diuretics enhance renal blood flow (RBF)?
In what way do loop diuretics enhance renal blood flow (RBF)?
What kind of edema are diuretics like loop diuretics not effective in treating?
What kind of edema are diuretics like loop diuretics not effective in treating?
What physiological changes occur with the use of loop diuretics and contribute to the treatment of acute pulmonary edema?
What physiological changes occur with the use of loop diuretics and contribute to the treatment of acute pulmonary edema?
How do carbonic anhydrase inhibitors like acetazolamide affect intraocular pressure?
How do carbonic anhydrase inhibitors like acetazolamide affect intraocular pressure?
What is the primary site of action for loop diuretics in the nephron?
What is the primary site of action for loop diuretics in the nephron?
Explain how renal Na+ retention leads to transudative edema in congestive heart failure.
Explain how renal Na+ retention leads to transudative edema in congestive heart failure.
What compensatory measure should be taken in acute hyperkalemia to enhance K+ excretion?
What compensatory measure should be taken in acute hyperkalemia to enhance K+ excretion?
What is the relationship between liver cirrhosis and the development of ascites?
What is the relationship between liver cirrhosis and the development of ascites?
Identify an adverse effect of loop diuretics related to electrolyte imbalances.
Identify an adverse effect of loop diuretics related to electrolyte imbalances.
In nephrotic syndrome, what is the primary physiological change that results in edema formation?
In nephrotic syndrome, what is the primary physiological change that results in edema formation?
Compare and contrast renal and extra-renal diuretics in terms of their mechanisms.
Compare and contrast renal and extra-renal diuretics in terms of their mechanisms.
Explain the relationship between hyponatremia and vascular smooth muscle response to catecholamines.
Explain the relationship between hyponatremia and vascular smooth muscle response to catecholamines.
What role does hypoalbuminemia play in the mechanism of edema related to liver cirrhosis?
What role does hypoalbuminemia play in the mechanism of edema related to liver cirrhosis?
What is a potential complication of administering loop diuretics that may require monitoring for specific symptoms?
What is a potential complication of administering loop diuretics that may require monitoring for specific symptoms?
What distinguishes thiazide diuretics from other types of diuretics in terms of their chemical structure?
What distinguishes thiazide diuretics from other types of diuretics in terms of their chemical structure?
Describe how thiazide diuretics are classified based on their action within the nephron.
Describe how thiazide diuretics are classified based on their action within the nephron.
How does the absorption of thiazide diuretics occur in the gastrointestinal tract?
How does the absorption of thiazide diuretics occur in the gastrointestinal tract?
What is the effect of osmotic diuretics on renal tubular fluid and urine output?
What is the effect of osmotic diuretics on renal tubular fluid and urine output?
How does the activation of the renin-angiotensin-aldosterone system contribute to the pathophysiology of edema in congestive heart failure?
How does the activation of the renin-angiotensin-aldosterone system contribute to the pathophysiology of edema in congestive heart failure?
What is one potential adverse effect of thiazide-like diuretics that practitioners should be cautious about?
What is one potential adverse effect of thiazide-like diuretics that practitioners should be cautious about?
What effect do loop diuretics have on plasma volume during hypertensive emergencies?
What effect do loop diuretics have on plasma volume during hypertensive emergencies?
What is the effect of thiazide diuretics on calcium excretion and how does this relate to kidney stones?
What is the effect of thiazide diuretics on calcium excretion and how does this relate to kidney stones?
Describe the paradoxical action of thiazides in patients with nephrogenic diabetes insipidus.
Describe the paradoxical action of thiazides in patients with nephrogenic diabetes insipidus.
What is the maximum excretion limit for filtered Na+ load in thiazide action and its implication for renal function?
What is the maximum excretion limit for filtered Na+ load in thiazide action and its implication for renal function?
Explain the relationship between thiazide diuretics and electrolyte disturbances, specifically hypokalemia.
Explain the relationship between thiazide diuretics and electrolyte disturbances, specifically hypokalemia.
What adverse metabolic effects can thiazides induce aside from electrolyte imbalances?
What adverse metabolic effects can thiazides induce aside from electrolyte imbalances?
Discuss the impact of renal prostaglandins on the action of thiazide diuretics compared to loop diuretics.
Discuss the impact of renal prostaglandins on the action of thiazide diuretics compared to loop diuretics.
What is the significance of combining thiazides with other antihypertensive drugs?
What is the significance of combining thiazides with other antihypertensive drugs?
Identify the primary adverse effects of thiazide diuretics that need monitoring in clinical practice.
Identify the primary adverse effects of thiazide diuretics that need monitoring in clinical practice.
Transudative edema is associated with renal ______ retention.
Transudative edema is associated with renal ______ retention.
In congestive heart failure (CHF), the decreased ______ causes renal ischemia.
In congestive heart failure (CHF), the decreased ______ causes renal ischemia.
Liver cirrhosis leads to a decrease in plasma ______ pressure due to insufficient albumin synthesis.
Liver cirrhosis leads to a decrease in plasma ______ pressure due to insufficient albumin synthesis.
In nephrotic syndrome, glomerular dysfunction results in excessive loss of plasma ______ in urine.
In nephrotic syndrome, glomerular dysfunction results in excessive loss of plasma ______ in urine.
Thiazide diuretics act on the proximal part of the ______ convoluted tubule.
Thiazide diuretics act on the proximal part of the ______ convoluted tubule.
Osmotic diuretics, such as ______, increase the osmotic pressure of tubular fluid.
Osmotic diuretics, such as ______, increase the osmotic pressure of tubular fluid.
K+ sparing diuretics act on the distal part of the ______ convoluted tubule.
K+ sparing diuretics act on the distal part of the ______ convoluted tubule.
Digitalis in CHF leads to increased ______, enhancing renal blood flow.
Digitalis in CHF leads to increased ______, enhancing renal blood flow.
Acute renal failure necessitates the maintenance of adequate ______ and enhances K+ excretion.
Acute renal failure necessitates the maintenance of adequate ______ and enhances K+ excretion.
Saline should be given to compensate for Na+ and water loss in cases of acute ______.
Saline should be given to compensate for Na+ and water loss in cases of acute ______.
Loop diuretics can cause electrolyte disturbances such as hyponatremia, hypokalemia, hypomagnesemia, and ______.
Loop diuretics can cause electrolyte disturbances such as hyponatremia, hypokalemia, hypomagnesemia, and ______.
Hypokalemic metabolic alkalosis is due to increased tubular secretion of K+ and ______.
Hypokalemic metabolic alkalosis is due to increased tubular secretion of K+ and ______.
Ototoxicity, which may lead to reversible hearing loss, occurs with very high doses and can impair ion transport in the ______.
Ototoxicity, which may lead to reversible hearing loss, occurs with very high doses and can impair ion transport in the ______.
Thiazide diuretics are absorbed from the GIT and are secreted into the lumen of the PCT by an organic acid ______ system.
Thiazide diuretics are absorbed from the GIT and are secreted into the lumen of the PCT by an organic acid ______ system.
The diuresis effect of thiazide diuretics is typically produced within ______ hours after administration.
The diuresis effect of thiazide diuretics is typically produced within ______ hours after administration.
True thiazides are derivatives of ______.
True thiazides are derivatives of ______.
Carbonic anhydrase inhibitors, such as acetazolamide, are weak ______ that decrease NaHCO3 reabsorption.
Carbonic anhydrase inhibitors, such as acetazolamide, are weak ______ that decrease NaHCO3 reabsorption.
Loop diuretics inhibit the ______ co-transport system in the thick ascending limb of the loop of Henle.
Loop diuretics inhibit the ______ co-transport system in the thick ascending limb of the loop of Henle.
The therapeutic uses of loop diuretics include treating edematous conditions such as congestive heart ______.
The therapeutic uses of loop diuretics include treating edematous conditions such as congestive heart ______.
Diuresis from loop diuretics occurs within ______ minutes after intravenous administration.
Diuresis from loop diuretics occurs within ______ minutes after intravenous administration.
Prostaglandins, produced by loop diuretics, lead to increased renal ______ flow.
Prostaglandins, produced by loop diuretics, lead to increased renal ______ flow.
Acetazolamide can be used in the treatment of ______, a condition characterized by increased intraocular pressure.
Acetazolamide can be used in the treatment of ______, a condition characterized by increased intraocular pressure.
Loop diuretics increase the excretion of ______, magnesium, halides, and hydrogen ions.
Loop diuretics increase the excretion of ______, magnesium, halides, and hydrogen ions.
Diuretics are not effective in treating edema due to ______ obstruction.
Diuretics are not effective in treating edema due to ______ obstruction.
Thiazides inhibit the Na+/Cl― co-transport system in the proximal part of the ______.
Thiazides inhibit the Na+/Cl― co-transport system in the proximal part of the ______.
Thiazides can reduce urine volume in some cases of nephrogenic diabetes ______.
Thiazides can reduce urine volume in some cases of nephrogenic diabetes ______.
Thiazides have moderate efficacy, with a maximum excretion of filtered Na+ load of only ______%
Thiazides have moderate efficacy, with a maximum excretion of filtered Na+ load of only ______%
Thiazides can lead to electrolyte disturbances such as ______ and hypokalemia.
Thiazides can lead to electrolyte disturbances such as ______ and hypokalemia.
The action of thiazides depends on renal ______ like loop diuretics.
The action of thiazides depends on renal ______ like loop diuretics.
Thiazides are often combined with other antihypertensive drugs to enhance their ______ effects.
Thiazides are often combined with other antihypertensive drugs to enhance their ______ effects.
One potential adverse effect of thiazides is ______, due to increased tubular secretion of K+ and H+.
One potential adverse effect of thiazides is ______, due to increased tubular secretion of K+ and H+.
Thiazides can cause ______, which is related to both decreased pancreatic release of insulin and decreased tissue utilization of glucose.
Thiazides can cause ______, which is related to both decreased pancreatic release of insulin and decreased tissue utilization of glucose.
Transudative edema is usually generalized and is associated with renal ______ retention.
Transudative edema is usually generalized and is associated with renal ______ retention.
In congestive heart failure (CHF), the decreased ______ causes renal ischemia.
In congestive heart failure (CHF), the decreased ______ causes renal ischemia.
The cirrhotic liver cannot synthesize sufficient ______ and other plasma proteins.
The cirrhotic liver cannot synthesize sufficient ______ and other plasma proteins.
Diuretics are drugs that increase urine volume and ______ excretion.
Diuretics are drugs that increase urine volume and ______ excretion.
Thiazide diuretics act on the proximal part of the ______.
Thiazide diuretics act on the proximal part of the ______.
Osmotic diuretics prevent water reabsorption by increasing the osmotic pressure of ______ fluid.
Osmotic diuretics prevent water reabsorption by increasing the osmotic pressure of ______ fluid.
Nephrotic syndrome results in excessive loss of plasma ______ in urine.
Nephrotic syndrome results in excessive loss of plasma ______ in urine.
Loop diuretics, such as furosemide, act on the ascending limb of the loop of ______.
Loop diuretics, such as furosemide, act on the ascending limb of the loop of ______.
Carbonic anhydrase inhibitors, such as acetazolamide, may cause metabolic ______
Carbonic anhydrase inhibitors, such as acetazolamide, may cause metabolic ______
Loop diuretics are known to inhibit the Na+/K+/2Cl― ______ system in the thick ascending limb of LOH.
Loop diuretics are known to inhibit the Na+/K+/2Cl― ______ system in the thick ascending limb of LOH.
Diuresis from loop diuretics occurs within ______ minutes after intravenous administration.
Diuresis from loop diuretics occurs within ______ minutes after intravenous administration.
They cause venodilatation leading to a decrease in ______ return.
They cause venodilatation leading to a decrease in ______ return.
Loop diuretics are classified as ______ diuretics due to their potent effect on Na+ loss.
Loop diuretics are classified as ______ diuretics due to their potent effect on Na+ loss.
Prostaglandins are increased by loop diuretics and lead to enhanced renal ______ flow.
Prostaglandins are increased by loop diuretics and lead to enhanced renal ______ flow.
Loop diuretics increase the excretion of ______, Mg2+, halides, and H+.
Loop diuretics increase the excretion of ______, Mg2+, halides, and H+.
Patients with edema due to lymphatic obstruction or inflammatory edema should not be treated with ______.
Patients with edema due to lymphatic obstruction or inflammatory edema should not be treated with ______.
Acute hypercalcemia and acute hyperkalemia require saline to compensate for Na+ and water loss to maintain adequate ______.
Acute hypercalcemia and acute hyperkalemia require saline to compensate for Na+ and water loss to maintain adequate ______.
Loop diuretics cause peripheral VD due to increased production of ______ in many vascular beds.
Loop diuretics cause peripheral VD due to increased production of ______ in many vascular beds.
Thiazide diuretics are absorbed from the GIT and secreted into the lumen of the PCT by an organic acid excretory ______.
Thiazide diuretics are absorbed from the GIT and secreted into the lumen of the PCT by an organic acid excretory ______.
Adverse effects of loop diuretics include hypovolemia, hypotension, and electrolyte disturbances such as hypokalemia and ______.
Adverse effects of loop diuretics include hypovolemia, hypotension, and electrolyte disturbances such as hypokalemia and ______.
Hypokalemic metabolic alkalosis occurs due to increased tubular secretion of ______ and H+.
Hypokalemic metabolic alkalosis occurs due to increased tubular secretion of ______ and H+.
Thiazide diuretics are divided into true thiazides and ______-like diuretics.
Thiazide diuretics are divided into true thiazides and ______-like diuretics.
Ototoxicity associated with loop diuretics may be due to impairment of ion transport in the ______ vascularis.
Ototoxicity associated with loop diuretics may be due to impairment of ion transport in the ______ vascularis.
Adverse reactions from loop diuretics can include skin rash, eosinophilia, and interstitial ______.
Adverse reactions from loop diuretics can include skin rash, eosinophilia, and interstitial ______.
Thiazides inhibit Na+/Cl― co-transport system in the proximal part of the ______, leading to inhibition of active reabsorption.
Thiazides inhibit Na+/Cl― co-transport system in the proximal part of the ______, leading to inhibition of active reabsorption.
Thiazides can reduce urine volume in some cases of nephrogenic diabetes ______.
Thiazides can reduce urine volume in some cases of nephrogenic diabetes ______.
Thiazides are often combined with other antihypertensive drugs to enhance their blood pressure- ______ effects.
Thiazides are often combined with other antihypertensive drugs to enhance their blood pressure- ______ effects.
Excess Na+ reaching the DCT is reabsorbed in exchange with ______, leading to K+ loss.
Excess Na+ reaching the DCT is reabsorbed in exchange with ______, leading to K+ loss.
Thiazides have moderate efficacy, with a maximum excretion of filtered Na+ load being only ______%.
Thiazides have moderate efficacy, with a maximum excretion of filtered Na+ load being only ______%.
Adverse effects of thiazides include electrolyte disturbances such as ______ and hypokalemia.
Adverse effects of thiazides include electrolyte disturbances such as ______ and hypokalemia.
Thiazides can lead to ______ metabolic alkalosis due to increased tubular secretion of K+ and H+.
Thiazides can lead to ______ metabolic alkalosis due to increased tubular secretion of K+ and H+.
The action of thiazides also depends on renal ______ like loop diuretics, but to a much lesser extent.
The action of thiazides also depends on renal ______ like loop diuretics, but to a much lesser extent.
Match the following causes of transudative edema with their primary mechanisms:
Match the following causes of transudative edema with their primary mechanisms:
Match the types of diuretics with their specific action sites:
Match the types of diuretics with their specific action sites:
Match the following diuretic classes with their mechanism of action:
Match the following diuretic classes with their mechanism of action:
Match each diuretic class with its primary clinical indication:
Match each diuretic class with its primary clinical indication:
Match the following complications with their associated diuretic class:
Match the following complications with their associated diuretic class:
Match the following conditions with their fluid management approaches:
Match the following conditions with their fluid management approaches:
Match each diuretic with its correct example:
Match each diuretic with its correct example:
Match the following terms regarding mechanisms of edema formation:
Match the following terms regarding mechanisms of edema formation:
Match the following diuretic types with their characteristics:
Match the following diuretic types with their characteristics:
Match the adverse effects with their corresponding diuretic class:
Match the adverse effects with their corresponding diuretic class:
Match the following conditions with their appropriate corrective actions:
Match the following conditions with their appropriate corrective actions:
Match the electrolyte disturbances with their corresponding causes:
Match the electrolyte disturbances with their corresponding causes:
Match the following diuretics with their primary pharmacokinetics:
Match the following diuretics with their primary pharmacokinetics:
Match the diuretic-related complications with their explanations:
Match the diuretic-related complications with their explanations:
Match the following mechanisms of action with their resulting effects:
Match the following mechanisms of action with their resulting effects:
Match the following adverse effects with their usual frequency or occurrence:
Match the following adverse effects with their usual frequency or occurrence:
Match the following diuretics with their therapeutic uses:
Match the following diuretics with their therapeutic uses:
Match the diuretics to their primary mechanism of action:
Match the diuretics to their primary mechanism of action:
Match the pharmacokinetic characteristics of the following diuretics:
Match the pharmacokinetic characteristics of the following diuretics:
Match the following diuretics with their side effects:
Match the following diuretics with their side effects:
Match the following physiological effects of loop diuretics:
Match the following physiological effects of loop diuretics:
Match each diuretic with its unique characteristic:
Match each diuretic with its unique characteristic:
Match the following diuretics with their impact on electrolyte levels:
Match the following diuretics with their impact on electrolyte levels:
Match each diuretic with its associated contraindication:
Match each diuretic with its associated contraindication:
Match the thiazide diuretic effects with their descriptions:
Match the thiazide diuretic effects with their descriptions:
Match the therapeutic uses of thiazides with their conditions:
Match the therapeutic uses of thiazides with their conditions:
Match the adverse effects of thiazides with their descriptions:
Match the adverse effects of thiazides with their descriptions:
Match the mechanisms of thiazides with their actions:
Match the mechanisms of thiazides with their actions:
Match the factors influencing thiazide effectiveness with their definitions:
Match the factors influencing thiazide effectiveness with their definitions:
Match the conditions that thiazides help to control with their specific applications:
Match the conditions that thiazides help to control with their specific applications:
Match the specific adverse effects with their possible causes:
Match the specific adverse effects with their possible causes:
Match the consequences of thiazide usage with their related outcomes:
Match the consequences of thiazide usage with their related outcomes:
Flashcards are hidden until you start studying
Study Notes
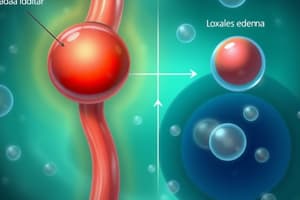
Transudative Edema
- Generally associated with renal sodium retention.
- Common causes include:
- Congestive Heart Failure (CHF): Decreased cardiac output leads to renal ischemia, activating the renin-angiotensin-aldosterone system (RAAS). This results in Na+ and water retention, causing edema.
- Liver Cirrhosis: Impaired liver function prevents adequate synthesis of albumin, decreasing plasma oncotic pressure, leading to hypoalbuminemia. Along with portal hypertension and RAAS stimulation, this contributes to fluid retention and ascites.
- Nephrotic Syndrome: Glomerular damage results in significant proteinuria, diminishing plasma oncotic pressure and leading to edema.
Diuretic Classes and Agents
- Diuretics promote increased urine volume and sodium excretion.
- Renal Diuretics (act directly on kidneys):
- Thiazide Diuretics: Inhibit Na+/Cl− reabsorption in distal convoluted tubule (DCT), e.g., hydrochlorothiazide.
- Loop Diuretics: Act on the thick ascending limb of the loop of Henle, e.g., furosemide.
- Potassium-Sparing Diuretics: Work on the distal part of the DCT, e.g., spironolactone.
- Osmotic Diuretics: Sustain osmotic pressure in tubular fluid, e.g., mannitol.
- Extra-Renal Diuretics (act indirectly):
- Increased water intake leads to reduced ADH release and diuresis.
- Digitalis in CHF enhances cardiac output, promoting renal blood flow.
- Intravenous albumin can augment osmotic pressure in certain edemas, facilitating fluid mobilization.
Loop Diuretics
- Examples: Furosemide, torsemide, bumetanide, ethacrynic acid.
- Pharmacokinetics:
- Absorbed from the gastrointestinal tract; secreted via organic acid excretory system.
- Furosemide absorption is erratic, while bumetanide is complete.
- Diuretic effect occurs within 5 minutes of intravenous and 30 minutes of oral dosing.
- Mechanism:
- Inhibit Na+/K+/2Cl− co-transport in the thick ascending limb of the loop of Henle, leading to significant losses of Na+, Cl−, and K+.
- Promote renal prostaglandin production, increasing renal blood flow (RBF) and glomerular filtration rate (GFR).
- Therapeutic Uses:
- Treats CHF, nephrotic syndrome, pulmonary edema, acute renal failure, hypercalcemia, and hypertensive emergencies.
- Adverse Effects:
- Potential for hypovolemia, hypotension, and electrolyte imbalances (hyponatremia, hypokalemia, hypomagnesemia).
- Risk of hypokalemic metabolic alkalosis and hyperuricemia, leading to acute gout.
- Ototoxicity occurs with high doses, particularly in renal impairment.
Thiazide Diuretics
- Types include true thiazides (e.g., hydrochlorothiazide) and thiazide-like diuretics (e.g., indapamide).
- Pharmacokinetics:
- Absorption from the GI tract; diuresis observed within 1-2 hours.
- Mechanism:
- Inhibit Na+/Cl− co-transport in proximal DCT, causing Na+, Cl− excretion with water.
- Moderate efficacy with maximum Na+ excretion of 5-7%; ineffective below GFR of 30-40 ml/min.
- Therapeutic Uses:
- Mild edematous states, essential hypertension, and hypercalcuria.
- Can paradoxically reduce urine volume in nephrogenic diabetes insipidus by enhancing ADH sensitivity.
- Adverse Effects:
- Similar to loop diuretics, including fluid balance issues and electrolyte disturbances.
- Associated with hyperglycemia and hyperlipidemia.
Transudative Edema
- Generally associated with renal sodium retention.
- Common causes include:
- Congestive Heart Failure (CHF): Decreased cardiac output leads to renal ischemia, activating the renin-angiotensin-aldosterone system (RAAS). This results in Na+ and water retention, causing edema.
- Liver Cirrhosis: Impaired liver function prevents adequate synthesis of albumin, decreasing plasma oncotic pressure, leading to hypoalbuminemia. Along with portal hypertension and RAAS stimulation, this contributes to fluid retention and ascites.
- Nephrotic Syndrome: Glomerular damage results in significant proteinuria, diminishing plasma oncotic pressure and leading to edema.
Diuretic Classes and Agents
- Diuretics promote increased urine volume and sodium excretion.
- Renal Diuretics (act directly on kidneys):
- Thiazide Diuretics: Inhibit Na+/Cl− reabsorption in distal convoluted tubule (DCT), e.g., hydrochlorothiazide.
- Loop Diuretics: Act on the thick ascending limb of the loop of Henle, e.g., furosemide.
- Potassium-Sparing Diuretics: Work on the distal part of the DCT, e.g., spironolactone.
- Osmotic Diuretics: Sustain osmotic pressure in tubular fluid, e.g., mannitol.
- Extra-Renal Diuretics (act indirectly):
- Increased water intake leads to reduced ADH release and diuresis.
- Digitalis in CHF enhances cardiac output, promoting renal blood flow.
- Intravenous albumin can augment osmotic pressure in certain edemas, facilitating fluid mobilization.
Loop Diuretics
- Examples: Furosemide, torsemide, bumetanide, ethacrynic acid.
- Pharmacokinetics:
- Absorbed from the gastrointestinal tract; secreted via organic acid excretory system.
- Furosemide absorption is erratic, while bumetanide is complete.
- Diuretic effect occurs within 5 minutes of intravenous and 30 minutes of oral dosing.
- Mechanism:
- Inhibit Na+/K+/2Cl− co-transport in the thick ascending limb of the loop of Henle, leading to significant losses of Na+, Cl−, and K+.
- Promote renal prostaglandin production, increasing renal blood flow (RBF) and glomerular filtration rate (GFR).
- Therapeutic Uses:
- Treats CHF, nephrotic syndrome, pulmonary edema, acute renal failure, hypercalcemia, and hypertensive emergencies.
- Adverse Effects:
- Potential for hypovolemia, hypotension, and electrolyte imbalances (hyponatremia, hypokalemia, hypomagnesemia).
- Risk of hypokalemic metabolic alkalosis and hyperuricemia, leading to acute gout.
- Ototoxicity occurs with high doses, particularly in renal impairment.
Thiazide Diuretics
- Types include true thiazides (e.g., hydrochlorothiazide) and thiazide-like diuretics (e.g., indapamide).
- Pharmacokinetics:
- Absorption from the GI tract; diuresis observed within 1-2 hours.
- Mechanism:
- Inhibit Na+/Cl− co-transport in proximal DCT, causing Na+, Cl− excretion with water.
- Moderate efficacy with maximum Na+ excretion of 5-7%; ineffective below GFR of 30-40 ml/min.
- Therapeutic Uses:
- Mild edematous states, essential hypertension, and hypercalcuria.
- Can paradoxically reduce urine volume in nephrogenic diabetes insipidus by enhancing ADH sensitivity.
- Adverse Effects:
- Similar to loop diuretics, including fluid balance issues and electrolyte disturbances.
- Associated with hyperglycemia and hyperlipidemia.
Transudative Edema
- Characterized by generalized swelling due to fluid accumulation, commonly linked with renal sodium retention.
- Key clinical causes include:
- Congestive Heart Failure (CHF): Leads to decreased cardiac output and renal ischemia, activating the Renin-Angiotensin-Aldosterone System (RAAS), resulting in sodium and water retention.
- Liver Cirrhosis: Impaired albumin production decreases plasma oncotic pressure, combined with portal hypertension, leads to fluid retention and ascites due to RAAS stimulation.
- Nephrotic Syndrome: Glomerular damage causes excessive protein loss in urine, lowering plasma oncotic pressure and causing edema.
Diuretics: Overview
- Diuretics increase urine volume and enhance sodium excretion.
- Natriuretic drugs specifically promote sodium elimination by the kidneys.
- Classification distinctions:
- Renal Diuretics: Act directly on renal structures.
- Extra-Renal Diuretics: Influence kidney function indirectly (e.g., increased water intake leading to reduced ADH release).
Diuretic Classes
-
Loop Diuretics (e.g., Furosemide):
- Act on the ascending limb of the loop of Henle, leading to potent diuresis.
- Mechanism: Inhibit Na+/K+/2Cl− co-transport, significantly increasing sodium, chloride, potassium, calcium, magnesium, and water excretion.
- Therapeutic uses: Manage conditions like CHF, nephrotic syndrome, acute pulmonary edema, renal failure, hypercalcemia, and hypertensive emergencies.
- Side effects include hypotension, electrolyte imbalances, hypokalemic metabolic alkalosis, and potential ototoxicity.
-
Thiazide Diuretics (e.g., Hydrochlorothiazide):
- Inhibit Na+/Cl− reabsorption in the distal convoluted tubule with milder diuresis (5-7% of filtered sodium).
- Effective for mild edema, essential hypertension, reducing urinary calcium excretion, and paradoxically aiding nephrogenic diabetes insipidus.
- Side effects match loop diuretics, with additional risks of hyperglycemia and hyperlipidemia.
Loop Diuretics Specifics
- Pharmacokinetics: Absorbed via the gastrointestinal tract; effects observed swiftly post-administration.
- Mechanism: Promotes vasodilation and increases renal blood flow, but NSAIDs can negate this effect.
- Not recommended for lymphatic obstruction or localized edema with high protein content.
Thiazide Diuretics Specifics
- Pharmacokinetics: Delayed onset of diuretic effect; effective in the presence of renal function.
- Mechanism: Enhance sodium excretion while decreasing calcium loss, which can enhance calcium retention in deficient situations.
Adverse Effects
- Common to both classes: Hypovolemia, hypotension, electrolyte disturbances, and metabolic alkalosis.
- Unique to loop diuretics: Ototoxicity, skin rashes, and possible kidney impairment with certain formulations.
- Unique to thiazides: Risk of hyperglycemia and lipid profile changes.
Key Takeaways
- Understanding the roles and mechanisms of diuretics is crucial for managing various medical conditions.
- Awareness of potential adverse effects is essential for safe administration and monitoring of treatment.
Transudative Edema
- Characterized by generalized swelling due to fluid accumulation, commonly linked with renal sodium retention.
- Key clinical causes include:
- Congestive Heart Failure (CHF): Leads to decreased cardiac output and renal ischemia, activating the Renin-Angiotensin-Aldosterone System (RAAS), resulting in sodium and water retention.
- Liver Cirrhosis: Impaired albumin production decreases plasma oncotic pressure, combined with portal hypertension, leads to fluid retention and ascites due to RAAS stimulation.
- Nephrotic Syndrome: Glomerular damage causes excessive protein loss in urine, lowering plasma oncotic pressure and causing edema.
Diuretics: Overview
- Diuretics increase urine volume and enhance sodium excretion.
- Natriuretic drugs specifically promote sodium elimination by the kidneys.
- Classification distinctions:
- Renal Diuretics: Act directly on renal structures.
- Extra-Renal Diuretics: Influence kidney function indirectly (e.g., increased water intake leading to reduced ADH release).
Diuretic Classes
-
Loop Diuretics (e.g., Furosemide):
- Act on the ascending limb of the loop of Henle, leading to potent diuresis.
- Mechanism: Inhibit Na+/K+/2Cl− co-transport, significantly increasing sodium, chloride, potassium, calcium, magnesium, and water excretion.
- Therapeutic uses: Manage conditions like CHF, nephrotic syndrome, acute pulmonary edema, renal failure, hypercalcemia, and hypertensive emergencies.
- Side effects include hypotension, electrolyte imbalances, hypokalemic metabolic alkalosis, and potential ototoxicity.
-
Thiazide Diuretics (e.g., Hydrochlorothiazide):
- Inhibit Na+/Cl− reabsorption in the distal convoluted tubule with milder diuresis (5-7% of filtered sodium).
- Effective for mild edema, essential hypertension, reducing urinary calcium excretion, and paradoxically aiding nephrogenic diabetes insipidus.
- Side effects match loop diuretics, with additional risks of hyperglycemia and hyperlipidemia.
Loop Diuretics Specifics
- Pharmacokinetics: Absorbed via the gastrointestinal tract; effects observed swiftly post-administration.
- Mechanism: Promotes vasodilation and increases renal blood flow, but NSAIDs can negate this effect.
- Not recommended for lymphatic obstruction or localized edema with high protein content.
Thiazide Diuretics Specifics
- Pharmacokinetics: Delayed onset of diuretic effect; effective in the presence of renal function.
- Mechanism: Enhance sodium excretion while decreasing calcium loss, which can enhance calcium retention in deficient situations.
Adverse Effects
- Common to both classes: Hypovolemia, hypotension, electrolyte disturbances, and metabolic alkalosis.
- Unique to loop diuretics: Ototoxicity, skin rashes, and possible kidney impairment with certain formulations.
- Unique to thiazides: Risk of hyperglycemia and lipid profile changes.
Key Takeaways
- Understanding the roles and mechanisms of diuretics is crucial for managing various medical conditions.
- Awareness of potential adverse effects is essential for safe administration and monitoring of treatment.
Transudative Edema
- Characterized by generalized swelling due to fluid accumulation, commonly linked with renal sodium retention.
- Key clinical causes include:
- Congestive Heart Failure (CHF): Leads to decreased cardiac output and renal ischemia, activating the Renin-Angiotensin-Aldosterone System (RAAS), resulting in sodium and water retention.
- Liver Cirrhosis: Impaired albumin production decreases plasma oncotic pressure, combined with portal hypertension, leads to fluid retention and ascites due to RAAS stimulation.
- Nephrotic Syndrome: Glomerular damage causes excessive protein loss in urine, lowering plasma oncotic pressure and causing edema.
Diuretics: Overview
- Diuretics increase urine volume and enhance sodium excretion.
- Natriuretic drugs specifically promote sodium elimination by the kidneys.
- Classification distinctions:
- Renal Diuretics: Act directly on renal structures.
- Extra-Renal Diuretics: Influence kidney function indirectly (e.g., increased water intake leading to reduced ADH release).
Diuretic Classes
-
Loop Diuretics (e.g., Furosemide):
- Act on the ascending limb of the loop of Henle, leading to potent diuresis.
- Mechanism: Inhibit Na+/K+/2Cl− co-transport, significantly increasing sodium, chloride, potassium, calcium, magnesium, and water excretion.
- Therapeutic uses: Manage conditions like CHF, nephrotic syndrome, acute pulmonary edema, renal failure, hypercalcemia, and hypertensive emergencies.
- Side effects include hypotension, electrolyte imbalances, hypokalemic metabolic alkalosis, and potential ototoxicity.
-
Thiazide Diuretics (e.g., Hydrochlorothiazide):
- Inhibit Na+/Cl− reabsorption in the distal convoluted tubule with milder diuresis (5-7% of filtered sodium).
- Effective for mild edema, essential hypertension, reducing urinary calcium excretion, and paradoxically aiding nephrogenic diabetes insipidus.
- Side effects match loop diuretics, with additional risks of hyperglycemia and hyperlipidemia.
Loop Diuretics Specifics
- Pharmacokinetics: Absorbed via the gastrointestinal tract; effects observed swiftly post-administration.
- Mechanism: Promotes vasodilation and increases renal blood flow, but NSAIDs can negate this effect.
- Not recommended for lymphatic obstruction or localized edema with high protein content.
Thiazide Diuretics Specifics
- Pharmacokinetics: Delayed onset of diuretic effect; effective in the presence of renal function.
- Mechanism: Enhance sodium excretion while decreasing calcium loss, which can enhance calcium retention in deficient situations.
Adverse Effects
- Common to both classes: Hypovolemia, hypotension, electrolyte disturbances, and metabolic alkalosis.
- Unique to loop diuretics: Ototoxicity, skin rashes, and possible kidney impairment with certain formulations.
- Unique to thiazides: Risk of hyperglycemia and lipid profile changes.
Key Takeaways
- Understanding the roles and mechanisms of diuretics is crucial for managing various medical conditions.
- Awareness of potential adverse effects is essential for safe administration and monitoring of treatment.
Transudative Edema
- Characterized by generalized swelling due to fluid accumulation, commonly linked with renal sodium retention.
- Key clinical causes include:
- Congestive Heart Failure (CHF): Leads to decreased cardiac output and renal ischemia, activating the Renin-Angiotensin-Aldosterone System (RAAS), resulting in sodium and water retention.
- Liver Cirrhosis: Impaired albumin production decreases plasma oncotic pressure, combined with portal hypertension, leads to fluid retention and ascites due to RAAS stimulation.
- Nephrotic Syndrome: Glomerular damage causes excessive protein loss in urine, lowering plasma oncotic pressure and causing edema.
Diuretics: Overview
- Diuretics increase urine volume and enhance sodium excretion.
- Natriuretic drugs specifically promote sodium elimination by the kidneys.
- Classification distinctions:
- Renal Diuretics: Act directly on renal structures.
- Extra-Renal Diuretics: Influence kidney function indirectly (e.g., increased water intake leading to reduced ADH release).
Diuretic Classes
-
Loop Diuretics (e.g., Furosemide):
- Act on the ascending limb of the loop of Henle, leading to potent diuresis.
- Mechanism: Inhibit Na+/K+/2Cl− co-transport, significantly increasing sodium, chloride, potassium, calcium, magnesium, and water excretion.
- Therapeutic uses: Manage conditions like CHF, nephrotic syndrome, acute pulmonary edema, renal failure, hypercalcemia, and hypertensive emergencies.
- Side effects include hypotension, electrolyte imbalances, hypokalemic metabolic alkalosis, and potential ototoxicity.
-
Thiazide Diuretics (e.g., Hydrochlorothiazide):
- Inhibit Na+/Cl− reabsorption in the distal convoluted tubule with milder diuresis (5-7% of filtered sodium).
- Effective for mild edema, essential hypertension, reducing urinary calcium excretion, and paradoxically aiding nephrogenic diabetes insipidus.
- Side effects match loop diuretics, with additional risks of hyperglycemia and hyperlipidemia.
Loop Diuretics Specifics
- Pharmacokinetics: Absorbed via the gastrointestinal tract; effects observed swiftly post-administration.
- Mechanism: Promotes vasodilation and increases renal blood flow, but NSAIDs can negate this effect.
- Not recommended for lymphatic obstruction or localized edema with high protein content.
Thiazide Diuretics Specifics
- Pharmacokinetics: Delayed onset of diuretic effect; effective in the presence of renal function.
- Mechanism: Enhance sodium excretion while decreasing calcium loss, which can enhance calcium retention in deficient situations.
Adverse Effects
- Common to both classes: Hypovolemia, hypotension, electrolyte disturbances, and metabolic alkalosis.
- Unique to loop diuretics: Ototoxicity, skin rashes, and possible kidney impairment with certain formulations.
- Unique to thiazides: Risk of hyperglycemia and lipid profile changes.
Key Takeaways
- Understanding the roles and mechanisms of diuretics is crucial for managing various medical conditions.
- Awareness of potential adverse effects is essential for safe administration and monitoring of treatment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.