Podcast
Questions and Answers
What is a key consequence of liver disease on fluid balance in the body?
What is a key consequence of liver disease on fluid balance in the body?
- Decreased hydrostatic pressure
- Decreased osmotic pressure (correct)
- Increased synthesis of albumin
- Increased osmotic pressure
Which condition can lead to lymphatic obstruction?
Which condition can lead to lymphatic obstruction?
- Increased sodium intake
- Cirrhosis
- Renal failure
- Cancer (correct)
How does sodium and water retention affect fluid dynamics in the body?
How does sodium and water retention affect fluid dynamics in the body?
- Decreases appetite for water
- Increases plasma oncotic pressure
- Decreases hydrostatic pressure
- Increases hydrostatic pressure (correct)
What is a primary effect of increased vascular permeability during inflammation?
What is a primary effect of increased vascular permeability during inflammation?
Which situation is likely to cause edema through direct damage to glomeruli?
Which situation is likely to cause edema through direct damage to glomeruli?
In which type of inflammation is edema likely to be observed?
In which type of inflammation is edema likely to be observed?
What role does hydrostatic pressure play in edema formation?
What role does hydrostatic pressure play in edema formation?
Which of the following does NOT contribute to edema in the body?
Which of the following does NOT contribute to edema in the body?
What is the rate of fluid reabsorption at the venous end of the capillary system?
What is the rate of fluid reabsorption at the venous end of the capillary system?
What happens if hydrostatic pressure at the venous end is elevated?
What happens if hydrostatic pressure at the venous end is elevated?
Which condition is a cause of oncotic edema?
Which condition is a cause of oncotic edema?
What is the rate at which fluid is drained through lymphatic capillaries?
What is the rate at which fluid is drained through lymphatic capillaries?
What results if the lymphatics cannot drain the surplus fluid?
What results if the lymphatics cannot drain the surplus fluid?
What type of edema results from injuries that make the vascular bed leaky?
What type of edema results from injuries that make the vascular bed leaky?
Which statement about hydrostatic edema is true?
Which statement about hydrostatic edema is true?
What primarily causes lymphedema?
What primarily causes lymphedema?
What components primarily make up a thrombus?
What components primarily make up a thrombus?
Which of the following is NOT considered one of the components of Virchow's triad for thrombosis?
Which of the following is NOT considered one of the components of Virchow's triad for thrombosis?
What is the potential outcome if thrombus fragments break off?
What is the potential outcome if thrombus fragments break off?
What condition is characterized by a restriction of blood flow to a tissue?
What condition is characterized by a restriction of blood flow to a tissue?
Which type of emboli are the most common?
Which type of emboli are the most common?
What happens during severe ischemia if there is no alternate blood supply?
What happens during severe ischemia if there is no alternate blood supply?
Which condition is characterized by an irreversible process that typically leads to tissue necrosis?
Which condition is characterized by an irreversible process that typically leads to tissue necrosis?
What is a consequence of chronic thrombi?
What is a consequence of chronic thrombi?
What primarily causes localized edema?
What primarily causes localized edema?
Which condition is NOT a common cause of hemorrhage?
Which condition is NOT a common cause of hemorrhage?
What distinguishes exudate from transudate?
What distinguishes exudate from transudate?
What is the term for blood accumulation within a tissue?
What is the term for blood accumulation within a tissue?
Which of the following conditions is likely to result in generalized edema?
Which of the following conditions is likely to result in generalized edema?
What condition contributes to the increased hydrostatic pressure in generalized edema?
What condition contributes to the increased hydrostatic pressure in generalized edema?
Which of the following is a common cause of hemorrhage exacerbated by blood clotting defects?
Which of the following is a common cause of hemorrhage exacerbated by blood clotting defects?
Which type of edema results from sodium retention due to kidney disease?
Which type of edema results from sodium retention due to kidney disease?
What characterizes a red (hemorrhagic) infarct?
What characterizes a red (hemorrhagic) infarct?
What is a defining factor of septic shock?
What is a defining factor of septic shock?
Which factor does NOT influence infarct development?
Which factor does NOT influence infarct development?
What is true about a white (anemic) infarct?
What is true about a white (anemic) infarct?
Which type of shock is characterized by the inability of the heart to pump blood?
Which type of shock is characterized by the inability of the heart to pump blood?
What common feature do cardiogenic and hypovolemic shock share?
What common feature do cardiogenic and hypovolemic shock share?
What results from arterial vasodilation during septic shock?
What results from arterial vasodilation during septic shock?
Which of the following describes the outcome of rapid vascular occlusion?
Which of the following describes the outcome of rapid vascular occlusion?
Flashcards are hidden until you start studying
Study Notes
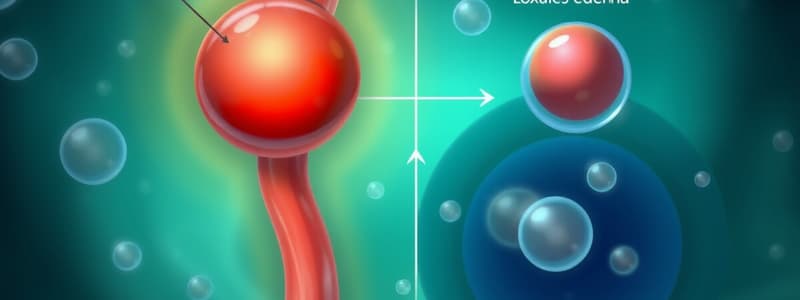
Edema
- Edema is a fluid accumulation in the interstitial spaces
- Edema formation is influenced by hydrostatic and oncotic pressures
- Increased hydrostatic pressure or decreased oncotic pressure leads to edema formation
- Hydrostatic Edema: Increased hydrostatic pressure at the venous end of capillaries hinders reabsorption
- Oncotic Edema: Reduction in plasma osmotic pressure due to albumin loss or deficiency causes fluid retention
- Lymphatic Edema: Lymphatic obstruction prohibits fluid resorption, leading to interstitial fluid accumulation
Localized vs Generalized Edema
- Localized: Specific area, caused by factors like vascular obstruction or lymphatic blockage
- Generalized: Systemic, caused by heart failure, decreased oncotic pressure, or sodium retention
Transudate vs Exudate
- Transudate: Protein-poor fluid due to high hydrostatic pressure or low colloid osmotic pressure
- Exudate: Protein-rich fluid due to increased vascular permeability
Hemorrhage
- Hemorrhage refers to bleeding outside the blood vessels
- It can be caused by damage to blood vessels, weakening of vessels due to conditions like atherosclerosis, infections, invasive tumors, hypertension, or hemorrhagic diatheses
Thrombosis
- Thrombus is a blood clot formed within a blood vessel
- Components of a Thrombus: Red blood cells, white blood cells, platelets, and fibrin
- Virchow's Triad: Factors promoting thrombosis: endothelial injury, abnormal blood flow, and hypercoagulability
Prognosis of Thrombosis
- Propagation: Thrombus enlarges
- Embolization: Thrombus fragment detaches and travels through the bloodstream
- Dissolution: Thrombus dissolves
- Organization and Recanalization: Tissue replaces the thrombus, forming new channels for blood flow
Complications of Thrombi
- Embolization: Fragments of the thrombus break off and travel in the bloodstream
- Ischemic injury: Reduced blood flow leading to tissue damage
- Infarction: Tissue death due to complete lack of blood flow
Embolism
- An embolus is a detached intravascular mass traveling through the bloodstream
- Types: Thromboemboli, Gas, Fat, Tumor, Foreign Body
Ischemia
- Ischemia is restricted or reduced blood flow to an area of tissue
- Causes: Decreased blood supply, obstruction due to thrombus, embolus, pressure, or vessel wall damage
- Prognosis: No effect if alternate blood supply exists, but severe or complete ischemia can lead to infarction
Infarction
- Infarct is an area of necrotic tissue due to occlusion of the vascular supply
- It is irreversible and replaced by scar tissue
- Classification:
- Red (hemorrhagic): Venous or arterial occlusion, tissues with dual blood supply, previously congested tissue, re-established flow after infarction.
- White (anemic): Arterial occlusion in solid organs
- Septic: Microbial infection causing abscess formation
- Bland: No microbial infection
Influencing Factors of Infarct Development
- Anatomy of the vascular supply
- Rate of occlusion
- Tissue vulnerability to hypoxia
Shock
- Shock is a life-threatening condition characterized by diminished cardiac output and reduced effective circulating blood volume
- It leads to impaired tissue perfusion and cellular hypoxia
- Categories:
- Cardiogenic: Heart failure due to myocardial damage, compression, or outflow obstruction
- Hypovolemic: Loss of blood or plasma volume
- Septic: Triggers by infections, associated with severe systemic inflammatory response
- Anaphylactic: Severe allergic reaction, rapid drop in blood pressure, and widespread vasodilation.
- Neurogenic: Damage to the nervous system resulting in vasodilation and decreased blood pressure.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.