Podcast
Questions and Answers
Which of the following statements describes the pathophysiology of asthma?
Which of the following statements describes the pathophysiology of asthma?
- Asthma is characterized by irreversible airflow limitation.
- Asthma does not involve mucus secretion.
- Asthma involves chronic inflammation and bronchoconstriction. (correct)
- Asthma is primarily caused by aging.
Cigarette smoking can trigger asthma attacks.
Cigarette smoking can trigger asthma attacks.
True (A)
What are the expected patient outcomes for asthma in terms of airway management?
What are the expected patient outcomes for asthma in terms of airway management?
Maintain open airway, normal breath sounds and respiratory rate, normal or personal best objective lung function measurements, and participation in activities of daily living (ADLs).
The primary characteristic of Chronic Obstructive Pulmonary Disease (COPD) is persistent _______ limitation.
The primary characteristic of Chronic Obstructive Pulmonary Disease (COPD) is persistent _______ limitation.
Match the following conditions with their characteristics:
Match the following conditions with their characteristics:
What is a key characteristic of asthma?
What is a key characteristic of asthma?
Airway inflammation in asthma is caused only by allergens.
Airway inflammation in asthma is caused only by allergens.
Name one mechanism that leads to airway obstruction in obstructive pulmonary diseases.
Name one mechanism that leads to airway obstruction in obstructive pulmonary diseases.
In asthma, bronchoconstriction is primarily caused by __________ of smooth muscle.
In asthma, bronchoconstriction is primarily caused by __________ of smooth muscle.
Match the following triggers for asthma attacks with their descriptions:
Match the following triggers for asthma attacks with their descriptions:
Which of the following is a common clinical manifestation of COPD?
Which of the following is a common clinical manifestation of COPD?
Barrel chest is a characteristic feature of COPD.
Barrel chest is a characteristic feature of COPD.
What is the primary treatment goal in managing COPD symptoms?
What is the primary treatment goal in managing COPD symptoms?
A patient with COPD may experience an increased work of breathing due to __________.
A patient with COPD may experience an increased work of breathing due to __________.
Match the following medications to their types used in COPD management:
Match the following medications to their types used in COPD management:
What best describes cor pulmonale in relation to COPD?
What best describes cor pulmonale in relation to COPD?
Pursed lip breathing can help patients with COPD by prolonging expiration.
Pursed lip breathing can help patients with COPD by prolonging expiration.
What is a significant complication that can arise due to worsening COPD?
What is a significant complication that can arise due to worsening COPD?
The use of _________ muscles signifies advanced respiratory distress in COPD patients.
The use of _________ muscles signifies advanced respiratory distress in COPD patients.
Which of the following interventions is NOT used in the management of COPD?
Which of the following interventions is NOT used in the management of COPD?
What is a major characteristic of asthma's early phase response?
What is a major characteristic of asthma's early phase response?
The late phase response of asthma peaks 15-30 minutes after exposure to a trigger.
The late phase response of asthma peaks 15-30 minutes after exposure to a trigger.
Name two inflammatory cells involved in asthma.
Name two inflammatory cells involved in asthma.
Increased vascular permeability in asthma leads to __________ formation.
Increased vascular permeability in asthma leads to __________ formation.
Match the following asthma characteristics with their descriptions:
Match the following asthma characteristics with their descriptions:
What is one of the expected patient outcomes for asthma management?
What is one of the expected patient outcomes for asthma management?
Chronic obstructive pulmonary disease (COPD) can be fully reversed with treatment.
Chronic obstructive pulmonary disease (COPD) can be fully reversed with treatment.
Name one trigger for COPD as mentioned in the content.
Name one trigger for COPD as mentioned in the content.
The presence of mucosal edema leads to bronchial __________ in COPD patients.
The presence of mucosal edema leads to bronchial __________ in COPD patients.
Match the following COPD characteristics with their descriptions:
Match the following COPD characteristics with their descriptions:
What is the primary characteristic of asthma?
What is the primary characteristic of asthma?
Airway obstruction in asthma can only occur due to allergens.
Airway obstruction in asthma can only occur due to allergens.
Name one factor that can lead to airway obstruction in obstructive pulmonary diseases.
Name one factor that can lead to airway obstruction in obstructive pulmonary diseases.
In asthma, airway hyper-responsiveness is a key feature influenced by exposure to __________.
In asthma, airway hyper-responsiveness is a key feature influenced by exposure to __________.
Match the airway obstruction causes to their descriptions:
Match the airway obstruction causes to their descriptions:
Which symptom is typically the earliest indicator of COPD?
Which symptom is typically the earliest indicator of COPD?
Cor pulmonale is characterized by the enlargement of the left side of the heart due to COPD.
Cor pulmonale is characterized by the enlargement of the left side of the heart due to COPD.
What condition is an acute exacerbation of COPD most commonly caused by?
What condition is an acute exacerbation of COPD most commonly caused by?
The barrel-shaped chest results from impaired _______ function in COPD.
The barrel-shaped chest results from impaired _______ function in COPD.
Match the following types of oxygen therapy with their flow rates:
Match the following types of oxygen therapy with their flow rates:
Which of the following is a common medication used for bronchodilator therapy in COPD?
Which of the following is a common medication used for bronchodilator therapy in COPD?
Pursed lip breathing can help reduce feelings of breathlessness in COPD patients.
Pursed lip breathing can help reduce feelings of breathlessness in COPD patients.
List one lifestyle change that can help prevent disease progression in COPD.
List one lifestyle change that can help prevent disease progression in COPD.
What is one of the primary goals of interprofessional care for COPD patients?
What is one of the primary goals of interprofessional care for COPD patients?
Common clinical manifestations of COPD include cough, _______ production, and dyspnea.
Common clinical manifestations of COPD include cough, _______ production, and dyspnea.
Which of the following medications is a long-acting inhaled beta 2 adrenergic agonist?
Which of the following medications is a long-acting inhaled beta 2 adrenergic agonist?
Anticholinergics are used mainly as long-term control medications for asthma.
Anticholinergics are used mainly as long-term control medications for asthma.
What is the main purpose of using a metered dose inhaler with a spacer?
What is the main purpose of using a metered dose inhaler with a spacer?
The green zone indicates that a person is ________.
The green zone indicates that a person is ________.
Match the following asthma medications with their types:
Match the following asthma medications with their types:
Which zone indicates that immediate medical attention is needed for asthma?
Which zone indicates that immediate medical attention is needed for asthma?
Long-acting oral beta 2 adrenergic agonists are intended for quick relief of asthma symptoms.
Long-acting oral beta 2 adrenergic agonists are intended for quick relief of asthma symptoms.
What frequency range indicates that a patient's asthma is in the yellow zone?
What frequency range indicates that a patient's asthma is in the yellow zone?
Which of the following is a common trigger for asthma attacks?
Which of the following is a common trigger for asthma attacks?
Wheezing can be present in patients with both minor and severe asthma attacks.
Wheezing can be present in patients with both minor and severe asthma attacks.
What is the primary characteristic of status asthmaticus?
What is the primary characteristic of status asthmaticus?
In asthma management, _________ medications are used for immediate relief.
In asthma management, _________ medications are used for immediate relief.
Match the following clinical manifestations with their descriptions:
Match the following clinical manifestations with their descriptions:
What is one of the diagnostic studies used to confirm airflow obstruction in asthma?
What is one of the diagnostic studies used to confirm airflow obstruction in asthma?
Hyperinflation and air trapping of the alveoli is a sign of asthma exacerbation.
Hyperinflation and air trapping of the alveoli is a sign of asthma exacerbation.
Name one factor that can increase work of breathing in asthma.
Name one factor that can increase work of breathing in asthma.
In severe cases of asthma, a _______ chest may indicate greatly diminished breath sounds.
In severe cases of asthma, a _______ chest may indicate greatly diminished breath sounds.
Which medication type helps to reduce inflammation in asthma patients?
Which medication type helps to reduce inflammation in asthma patients?
Patients with asthma may have no symptoms between attacks.
Patients with asthma may have no symptoms between attacks.
What is the purpose of an asthma action plan?
What is the purpose of an asthma action plan?
ABG changes in an asthma patient may indicate ________ and hypercapnia.
ABG changes in an asthma patient may indicate ________ and hypercapnia.
Match the patterns of asthma medication with their effects:
Match the patterns of asthma medication with their effects:
What is one primary characteristic of asthma as an obstructive pulmonary disease?
What is one primary characteristic of asthma as an obstructive pulmonary disease?
What is the primary characteristic of the late-phase response in asthma?
What is the primary characteristic of the late-phase response in asthma?
Which of the following mechanisms can lead to airway obstruction in obstructive pulmonary diseases?
Which of the following mechanisms can lead to airway obstruction in obstructive pulmonary diseases?
Which inflammatory cells play a significant role in asthma pathophysiology during the late-phase response?
Which inflammatory cells play a significant role in asthma pathophysiology during the late-phase response?
Which of the following factors contributes to airway hyper-responsiveness in asthma?
Which of the following factors contributes to airway hyper-responsiveness in asthma?
What is predominantly released by mast cells when an allergen attaches to IgE receptors in asthma?
What is predominantly released by mast cells when an allergen attaches to IgE receptors in asthma?
What is the timeline for the peak of the late-phase response after exposure to a trigger?
What is the timeline for the peak of the late-phase response after exposure to a trigger?
What role does airway inflammation play in the pathophysiology of asthma?
What role does airway inflammation play in the pathophysiology of asthma?
Which symptom is NOT commonly associated with the early-phase response of asthma?
Which symptom is NOT commonly associated with the early-phase response of asthma?
In asthma pathophysiology, what is the primary consequence of mast cell degranulation?
In asthma pathophysiology, what is the primary consequence of mast cell degranulation?
What is the primary benefit of medication given by inhalation compared to systemic administration?
What is the primary benefit of medication given by inhalation compared to systemic administration?
At what percentage of personal best peak flow is a patient in the 'Red Zone'?
At what percentage of personal best peak flow is a patient in the 'Red Zone'?
Which medication class is specifically classified as a short-acting muscarinic antagonist?
Which medication class is specifically classified as a short-acting muscarinic antagonist?
Which of the following indicates that a patient is in the 'Yellow Zone' regarding asthma control?
Which of the following indicates that a patient is in the 'Yellow Zone' regarding asthma control?
What is a common adverse effect of using inhaled medications for asthma?
What is a common adverse effect of using inhaled medications for asthma?
What component of asthma medication is exemplified by omalizumab?
What component of asthma medication is exemplified by omalizumab?
Which statement regarding the use of beta-2 adrenergic agonists is TRUE?
Which statement regarding the use of beta-2 adrenergic agonists is TRUE?
Which method is preferable for ensuring accurate inhaler use by patients?
Which method is preferable for ensuring accurate inhaler use by patients?
Which nursing intervention is essential for a patient with inadequate airway clearance due to asthma?
Which nursing intervention is essential for a patient with inadequate airway clearance due to asthma?
What is a fundamental characteristic of Chronic Obstructive Pulmonary Disease (COPD)?
What is a fundamental characteristic of Chronic Obstructive Pulmonary Disease (COPD)?
Which factor significantly contributes to the pathophysiological changes in COPD?
Which factor significantly contributes to the pathophysiological changes in COPD?
What is one expected objective lung function measurement for a patient effectively managing asthma?
What is one expected objective lung function measurement for a patient effectively managing asthma?
Which of the following statements accurately describes the airway obstruction mechanisms in COPD?
Which of the following statements accurately describes the airway obstruction mechanisms in COPD?
What is a potential complication of Status Asthmaticus?
What is a potential complication of Status Asthmaticus?
Which of the following triggers can precipitate an asthma attack?
Which of the following triggers can precipitate an asthma attack?
What is the primary method used to assess airflow obstruction in asthma?
What is the primary method used to assess airflow obstruction in asthma?
Which medication category includes short-acting inhaled beta-adrenergic agonists?
Which medication category includes short-acting inhaled beta-adrenergic agonists?
What is a typical respiratory rate change during an acute asthma attack?
What is a typical respiratory rate change during an acute asthma attack?
What type of medical assessment helps monitor oxygen levels and need for intervention in asthma management?
What type of medical assessment helps monitor oxygen levels and need for intervention in asthma management?
Which of the following manifestations indicates severe airway obstruction in asthma patients?
Which of the following manifestations indicates severe airway obstruction in asthma patients?
Which of the following symptoms may vary in an asthma attack?
Which of the following symptoms may vary in an asthma attack?
What is the primary goal of interprofessional care for asthma management?
What is the primary goal of interprofessional care for asthma management?
Which diagnostic study is NOT typically used for diagnosing asthma?
Which diagnostic study is NOT typically used for diagnosing asthma?
What changes in breathing mechanics may occur during an asthma episode?
What changes in breathing mechanics may occur during an asthma episode?
What is a common psychological factor exacerbating asthma symptoms?
What is a common psychological factor exacerbating asthma symptoms?
What is a notable characteristic of cough in asthma patients?
What is a notable characteristic of cough in asthma patients?
What is a common physiological change seen in patients with COPD regarding lung shape?
What is a common physiological change seen in patients with COPD regarding lung shape?
Which of the following is a common sign that may suggest cor pulmonale in COPD patients?
Which of the following is a common sign that may suggest cor pulmonale in COPD patients?
What is one of the primary aims of interprofessional care in managing COPD?
What is one of the primary aims of interprofessional care in managing COPD?
Which of the following is NOT commonly used in the treatment of acute exacerbations of COPD?
Which of the following is NOT commonly used in the treatment of acute exacerbations of COPD?
What breathing technique is beneficial for COPD patients during dyspnea?
What breathing technique is beneficial for COPD patients during dyspnea?
Which of the following statements about the clinical manifestations of COPD is FALSE?
Which of the following statements about the clinical manifestations of COPD is FALSE?
What type of oxygen therapy flow rate is typically associated with a Venturi mask?
What type of oxygen therapy flow rate is typically associated with a Venturi mask?
In COPD management, which medication class is typically prescribed to help alleviate shortness of breath due to bronchospasm?
In COPD management, which medication class is typically prescribed to help alleviate shortness of breath due to bronchospasm?
What is a primary complication associated with acute exacerbations of COPD?
What is a primary complication associated with acute exacerbations of COPD?
Which of the following is a characteristic feature of COPD that may significantly impact a patient's posture?
Which of the following is a characteristic feature of COPD that may significantly impact a patient's posture?
Flashcards
Asthma Nursing Care Plan
Asthma Nursing Care Plan
A plan for managing asthma focusing on maintaining a patent airway, normal breathing, and lung function, allowing for daily activities.
COPD (Chronic Obstructive Pulmonary Disease)
COPD (Chronic Obstructive Pulmonary Disease)
A progressive, preventable lung disease marked by persistent airflow limitation. It involves chronic inflammation in airways and lungs.
COPD Pathophysiology
COPD Pathophysiology
COPD's cause: chronic inflammation in airways, lung tissues, and blood vessels, leading to irreversible airflow limitation during exhalation.
COPD Causes
COPD Causes
Signup and view all the flashcards
Airflow Limitation in COPD
Airflow Limitation in COPD
Signup and view all the flashcards
COPD
COPD
Signup and view all the flashcards
Symptoms of COPD
Symptoms of COPD
Signup and view all the flashcards
COPD Complications
COPD Complications
Signup and view all the flashcards
COPD Treatment - Medications
COPD Treatment - Medications
Signup and view all the flashcards
Oxygen Therapy in COPD
Oxygen Therapy in COPD
Signup and view all the flashcards
COPD Pulmonary Rehabilitation
COPD Pulmonary Rehabilitation
Signup and view all the flashcards
Acute Exacerbation of COPD
Acute Exacerbation of COPD
Signup and view all the flashcards
Cor Pulmonale
Cor Pulmonale
Signup and view all the flashcards
Dyspnea
Dyspnea
Signup and view all the flashcards
Barrel Chest
Barrel Chest
Signup and view all the flashcards
What is the most common airway obstruction?
What is the most common airway obstruction?
Signup and view all the flashcards
What is a key characteristic of asthma?
What is a key characteristic of asthma?
Signup and view all the flashcards
What are the hallmarks of asthma?
What are the hallmarks of asthma?
Signup and view all the flashcards
What causes early phase asthma response?
What causes early phase asthma response?
Signup and view all the flashcards
What are examples of inflammatory mediators released in asthma?
What are examples of inflammatory mediators released in asthma?
Signup and view all the flashcards
Early Asthma Response
Early Asthma Response
Signup and view all the flashcards
Late Asthma Response
Late Asthma Response
Signup and view all the flashcards
What triggers late phase asthma response?
What triggers late phase asthma response?
Signup and view all the flashcards
What distinguishes late phase from early phase?
What distinguishes late phase from early phase?
Signup and view all the flashcards
What is airway hyper-responsiveness?
What is airway hyper-responsiveness?
Signup and view all the flashcards
COPD Cause: Smoking
COPD Cause: Smoking
Signup and view all the flashcards
COPD Patho: Airflow Limitation
COPD Patho: Airflow Limitation
Signup and view all the flashcards
COPD Inflammation
COPD Inflammation
Signup and view all the flashcards
COPD Structural Changes
COPD Structural Changes
Signup and view all the flashcards
COPD: Irreversible?
COPD: Irreversible?
Signup and view all the flashcards
COPD: Air Trapping
COPD: Air Trapping
Signup and view all the flashcards
COPD: Barrel Chest
COPD: Barrel Chest
Signup and view all the flashcards
COPD: Prolonged Expiratory Phase
COPD: Prolonged Expiratory Phase
Signup and view all the flashcards
COPD: Weight Loss and Anorexia
COPD: Weight Loss and Anorexia
Signup and view all the flashcards
COPD: Tripod Positioning
COPD: Tripod Positioning
Signup and view all the flashcards
COPD: Cor Pulmonale
COPD: Cor Pulmonale
Signup and view all the flashcards
COPD: Acute Exacerbation
COPD: Acute Exacerbation
Signup and view all the flashcards
COPD: Acute Respiratory Failure
COPD: Acute Respiratory Failure
Signup and view all the flashcards
COPD: Depression and Anxiety
COPD: Depression and Anxiety
Signup and view all the flashcards
COPD: Oxygen Therapy
COPD: Oxygen Therapy
Signup and view all the flashcards
Airway Obstruction in Asthma
Airway Obstruction in Asthma
Signup and view all the flashcards
Asthma Triggers
Asthma Triggers
Signup and view all the flashcards
What are the classic signs of an asthma attack?
What are the classic signs of an asthma attack?
Signup and view all the flashcards
Status Asthmaticus
Status Asthmaticus
Signup and view all the flashcards
What are the key characteristics of status asthmaticus?
What are the key characteristics of status asthmaticus?
Signup and view all the flashcards
Why is status asthmaticus a medical emergency?
Why is status asthmaticus a medical emergency?
Signup and view all the flashcards
Asthma Action Plan
Asthma Action Plan
Signup and view all the flashcards
What are the two main categories of asthma medications?
What are the two main categories of asthma medications?
Signup and view all the flashcards
What are examples of 'reliever' asthma medications?
What are examples of 'reliever' asthma medications?
Signup and view all the flashcards
What are examples of 'controller' asthma medications?
What are examples of 'controller' asthma medications?
Signup and view all the flashcards
Why is it important to identify and avoid asthma triggers?
Why is it important to identify and avoid asthma triggers?
Signup and view all the flashcards
How can regularly monitoring lung function help manage asthma?
How can regularly monitoring lung function help manage asthma?
Signup and view all the flashcards
How can patient education and family involvement improve asthma management?
How can patient education and family involvement improve asthma management?
Signup and view all the flashcards
What is the goal of asthma treatment?
What is the goal of asthma treatment?
Signup and view all the flashcards
What is the hallmark of asthma?
What is the hallmark of asthma?
Signup and view all the flashcards
What's the early phase response in asthma?
What's the early phase response in asthma?
Signup and view all the flashcards
What characterizes the late phase response in asthma?
What characterizes the late phase response in asthma?
Signup and view all the flashcards
Why is asthma reversible?
Why is asthma reversible?
Signup and view all the flashcards
What are the key features of obstructive pulmonary diseases?
What are the key features of obstructive pulmonary diseases?
Signup and view all the flashcards
Asthma Medications: Quick Relief
Asthma Medications: Quick Relief
Signup and view all the flashcards
Asthma Medications: Long-Term Control
Asthma Medications: Long-Term Control
Signup and view all the flashcards
Peak Flow Meter: Green Zone
Peak Flow Meter: Green Zone
Signup and view all the flashcards
Peak Flow Meter: Yellow Zone
Peak Flow Meter: Yellow Zone
Signup and view all the flashcards
Peak Flow Meter: Red Zone
Peak Flow Meter: Red Zone
Signup and view all the flashcards
Inhaler Spacer
Inhaler Spacer
Signup and view all the flashcards
Inhalation vs. Oral Medications: Asthma
Inhalation vs. Oral Medications: Asthma
Signup and view all the flashcards
What is Obstructive Pulmonary Disease?
What is Obstructive Pulmonary Disease?
Signup and view all the flashcards
Key Feature of Asthma?
Key Feature of Asthma?
Signup and view all the flashcards
Asthma: Early Phase Response
Asthma: Early Phase Response
Signup and view all the flashcards
Asthma: Late Phase Response
Asthma: Late Phase Response
Signup and view all the flashcards
Airway Hyper-responsiveness in Asthma
Airway Hyper-responsiveness in Asthma
Signup and view all the flashcards
Early Phase Asthma Response
Early Phase Asthma Response
Signup and view all the flashcards
Late Phase Asthma Response
Late Phase Asthma Response
Signup and view all the flashcards
What distinguishes late phase asthma from early phase?
What distinguishes late phase asthma from early phase?
Signup and view all the flashcards
Airway Hyper-responsiveness
Airway Hyper-responsiveness
Signup and view all the flashcards
COPD: What is it?
COPD: What is it?
Signup and view all the flashcards
COPD: What are the main causes?
COPD: What are the main causes?
Signup and view all the flashcards
COPD: How does it affect breathing?
COPD: How does it affect breathing?
Signup and view all the flashcards
COPD: What are some common symptoms?
COPD: What are some common symptoms?
Signup and view all the flashcards
Asthma: What is it?
Asthma: What is it?
Signup and view all the flashcards
Inhaled Medications for Asthma
Inhaled Medications for Asthma
Signup and view all the flashcards
Oral Medications for Asthma
Oral Medications for Asthma
Signup and view all the flashcards
COPD: Who gets it?
COPD: Who gets it?
Signup and view all the flashcards
COPD: What does it look like?
COPD: What does it look like?
Signup and view all the flashcards
COPD: Why is exhaling hard?
COPD: Why is exhaling hard?
Signup and view all the flashcards
COPD: How does it affect the heart?
COPD: How does it affect the heart?
Signup and view all the flashcards
COPD: What are exacerbations?
COPD: What are exacerbations?
Signup and view all the flashcards
COPD: What does oxygen therapy do?
COPD: What does oxygen therapy do?
Signup and view all the flashcards
COPD: What is pulmonary rehab?
COPD: What is pulmonary rehab?
Signup and view all the flashcards
COPD: What are some key medications?
COPD: What are some key medications?
Signup and view all the flashcards
COPD: What can I do to prevent it?
COPD: What can I do to prevent it?
Signup and view all the flashcards
Study Notes
Week 10: NURS 2055: Adult Illness Concepts I
- Course is NURS 2055: Adult Illness Concepts I
- Specific chapter covered is Chapter 31: Nursing Management of Obstructive Pulmonary Diseases
- Instructor is Ainsley Miller, 2024
- Course is offered at Lakehead University
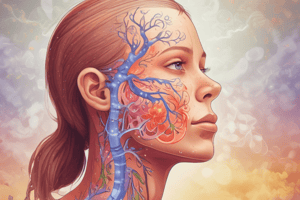
Obstructive Pulmonary Disease
- Most common pulmonary disorder
- Characterized by increased airway resistance
- Obstruction or narrowing of the airway causes resistance
- Airway obstruction results from:
- Accumulated secretions
- Edema
- Inflammation of the airways
- Bronchospasm of smooth muscle
- Destruction of lung tissue
- Combination of the above
Asthma
- Chronic inflammatory disorder of the airway
- Key characteristic is episodic and reversible airway obstruction.
- Hallmarks are airway inflammation and airway hyper-responsiveness.
- Degree of bronchoconstriction is related to airway narrowing, making it harder to breathe.
- Asthma has varying degrees of airway inflammation and hyper-responsiveness.
- Exposure to triggers (infections, allergens) lead to symptoms like wheezing, coughing, and shortness of breath.
Asthma - Early Phase Response
- Allergens or irritants bind to IgE receptors on mast cells
- Mast cells release inflammatory mediators (e.g., histamine)
- Intense inflammation leads to bronchial smooth muscle constriction.
- Increased vasodilation and permeability leads to swelling, and fluid build up
- Epithelial damage occurs from the inflammation and chemicals
- Peaks within 30-90 minutes of exposure to a trigger
- Subsides within another 30-90 minutes.
Asthma - Late Phase Response
- Inflammatory cells (eosinophils and neutrophils) infiltrate the airway and release mediators.
- Inflammation leads to mast cell degranulation and the release of histamine and other mediators.
- This creates a self-sustaining cycle of inflammation.
- Airway hyper-responsiveness increases.
- Peaks 5-12 hours after exposure to trigger
- May last for several hours to days.
- Inflammation is the primary characteristic, not bronchial smooth muscle contraction.
Asthma - Key Take Aways
- Reduction in airway diameter and increased airway resistance.
- Mucosal inflammation.
- Bronchial smooth muscle constriction.
- Excess mucus production.
- Hypertrophy of bronchial smooth muscle and thickening of basement membrane.
- Secretion of tenacious sputum.
- Hyperinflation and air trapping in the alveoli.
- Increased respiratory work.
- Respiratory function problems.
- Distribution of ventilation issues.
- Difficulty breathing.
Asthma Triggers
- Allergens (tobacco, marijuana smoke, nose and sinus conditions, medications, food additives, GERD, genetics)
- Air pollutants.
- Emotional stress.
- Exercise-induced (high-intensity workouts).
Asthma Clinical Manifestations
- Unpredictable, episodic, variable attacks.
- Wheezing.
- Breathlessness (dyspnea).
- Sensation of chest tightness.
- Coughing.
- Gradual or abrupt onset of symptoms.
- No symptoms between attacks.
- Prolonged expiration (1:3 or 1:4 ratio).
- Sitting upright or slightly bent forward using accessory muscles.
- Anxiety.
- Wheezing can be a sign for severe attacks as well as mild attacks.
- Silent chest may indicate severely diminished or absent breaths sounds.
Asthma Status Asthmaticus
- Life-threatening medical emergency
- Extreme form of acute asthma attack.
- Hypoxia, hypercapnia, acute respiratory failure.
- Precipitated by viral illnesses, environmental pollutants/allergens, drug allergies, or changes in medication regimen.
- Forced exhalation increases intrathoracic pressure.
- Hypoxemia and hypocapnia occur as the patient hyperventilates to maintain oxygenation, but they tire and CO2 is retained.
Asthma Diagnostic Studies
- Detailed history and physical examination.
- Family history of asthma, allergies, and eczema.
- Pulmonary function studies (spirometry, peak expiratory flow).
- Allergy assessment.
- Chest x-rays (may show hyperinflation but not diagnostic for asthma).
- Blood tests (eosinophils to assess airway inflammation).
- ABGs.
- Oximetry to assess oxygen levels.
Asthma Interprofessional Care
- Establishing partnerships with patients/families to identify and eliminate triggers.
- Patient and family teaching.
- Continuous assessment of asthma control and severity.
- Appropriate medication (relievers, rescue medications, controllers, maintenance medications).
- Asthma action plan.
- Regular follow-up.
Categories of Asthma Medications
-
Relievers (fast acting): Bronchodilators, anticholinergics.
- Short-acting beta-adrenergic agonists (e.g., salbutamol/ventolin).
- Anticholinergics/short-acting muscarinic antagonists (e.g., ipratropium/atrovent
-
Controllers (long-term): Anti-inflammatory medications.
- Corticosteroids -Leukotriene modifiers
- Anti-IgE -Long-acting beta adrenergic agonists (LABA) -Methylxanthines
Asthma Patient Education
- Name, dosage, administration method, frequency, indications, adverse effects, improper use consequences and importance of adherence.
- Assess patient's ability to use an inhaler accurately.
- Medications are typically via inhalation route
- Lower dose needed when using inhalers.
- Systemic adverse events/ side effects are reduced when using the inhaler method.
- Faster onset of action.
- Use of inhaler with spacer/meter dose inhaler
COPD
- Preventable disease characterized by persistent and progressive airflow limitation.
- Chronic inflammatory response in the airways and lungs leads to damage.
- Causes include smoking, noxious particles/gases, occupational chemicals and dusts, infection, heredity, and aging.
- Airflow limitations during forced exhalation due to loss of elastic recoil and are not easily reversed.
- Mucus hypersecretion, mucosal edema, and bronchospasm are contributors to the airflow limitations
COPD Clinical Manifestations
- Suspected when patient presents with cough, sputum production, and dyspnea+ history of smoking.
- Intermittent cough is an initial symptom.
- Interrupts daily activities due to breathing issues and difficulty performing daily tasks.
- Dyspnea usually triggers medical assessment.
- Barrel chest.
- Use of intercostal or accessory muscles
- Prolonged Expiratory phase
- Wheezes
- Decreased lung sounds
- Tripod position
- Purse lips when exhaling
- Edema is a sign of right-sided heart failure (HF).
COPD Complications
- Cor pulmonale (right-sided heart hypertrophy, often with or without heart failure) due to pulmonary hypertension.
- Sustained worsening of COPD symptoms during outbreaks can be due to bacterial issues.
- Acute respiratory failure (overall decline in lung function, deterioration in health status, and risk of death).
- Patients wait too long to reach health care providers when symptoms present as significant acute exacerbation of COPD.
- Depression and anxiety are possible experiences.
COPD Interprofessional Care
- Prevent disease progression through smoking cessation
- Reduce frequency and severity of exacerbations.
- Address respiratory symptoms and shortness of breath.
- Improve exercise tolerance.
- Treat exacerbations and complications of the disease
- Improve health status, quality of life, morbidity, and mortality.
COPD Medications
- Bronchodilator therapy (Beta 2 adrenergic agonists, anticholinergic medications).
- Long-acting theophylline preparations.
- Corticosteroids (oral for exacerbations).
- NSAIDs.
- Antibiotics (for exacerbations with purulent sputum).
- Influenza and pneumonia vaccinations.
COPD Pulmonary Rehabilitation
- Optimize functional status and quality of life.
- Implement aerobic conditioning (upper/lower body).
- Teach and utilize breathing exercises (e.g., pursed lip breathing).
- Address energy conservation techniques (e.g., huff coughing)
- Teach and address nutrition, smoking cessation, and environmental factors.
- Provide health promotion, patient education, and self-management strategies.
- Offer support and counselling for emotional well-being.
Comparison of COPD and Asthma
| Feature | COPD | Asthma |
|---|---|---|
| Age at onset | Usually >40 years | Usually <40 years |
| Smoking history | Usually >10 pack-years | Not causal but can be a trigger |
| Clinical symptoms | Persistent | Intermittent and variable |
| Sputum production | Often | Infrequent |
| Allergies | Infrequent | Often |
| Spirometry | Findings may improve but never normalize | Findings often normalize |
| Disease course | Progressive worsening with exacerbations | Stable with exacerbations |
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.