Podcast
Questions and Answers
Which of the following statements about DAMPs and PAMPs is true?
Which of the following statements about DAMPs and PAMPs is true?
- PAMPs originate from damaged tissues.
- Neither DAMPs nor PAMPs interact with pattern recognition receptors.
- DAMPs are released only from pathogens.
- Both DAMPs and PAMPs act as danger signals to the immune system. (correct)
M1 macrophages are associated with anti-inflammatory responses.
M1 macrophages are associated with anti-inflammatory responses.
False (B)
What are the two main phenotypes of macrophages?
What are the two main phenotypes of macrophages?
M1 and M2
DAMPs and PAMPs interact with _____ in the innate immune system to signal an immune response.
DAMPs and PAMPs interact with _____ in the innate immune system to signal an immune response.
Match the macrophage phenotype with its corresponding function:
Match the macrophage phenotype with its corresponding function:
What is a consequence of ischemia leading to ATP depletion?
What is a consequence of ischemia leading to ATP depletion?
Apoptosis is a chaotic process characterized by the rupture of the plasma cell membrane.
Apoptosis is a chaotic process characterized by the rupture of the plasma cell membrane.
What type of macrophages are involved in the inflammation during the early phase of acute kidney injury (AKI)?
What type of macrophages are involved in the inflammation during the early phase of acute kidney injury (AKI)?
Reperfusion leads to the production of ________ species which can cause lipid peroxidation.
Reperfusion leads to the production of ________ species which can cause lipid peroxidation.
Match the cellular responses to their descriptions in epithelial injury:
Match the cellular responses to their descriptions in epithelial injury:
Which of the following is NOT a consequence of intracellular lipase activation?
Which of the following is NOT a consequence of intracellular lipase activation?
Systemic inflammation can lead to acute kidney injury (AKI).
Systemic inflammation can lead to acute kidney injury (AKI).
What is the role of M2 macrophages in the context of ischemic injury?
What is the role of M2 macrophages in the context of ischemic injury?
What does DAMPs stand for?
What does DAMPs stand for?
Macrophage infiltration is associated with scarring and fibrosis in kidney injuries.
Macrophage infiltration is associated with scarring and fibrosis in kidney injuries.
What is the role of TGFβ in kidney injury?
What is the role of TGFβ in kidney injury?
The innate immune response is activated during _____ injury.
The innate immune response is activated during _____ injury.
Match the type of macrophage with its function during kidney injury:
Match the type of macrophage with its function during kidney injury:
What cellular response can lead to stress-induced senescence in tubular epithelial cells?
What cellular response can lead to stress-induced senescence in tubular epithelial cells?
Macrophages only have a pro-inflammatory role in kidney injury.
Macrophages only have a pro-inflammatory role in kidney injury.
What type of receptors are TLRs and NLRs?
What type of receptors are TLRs and NLRs?
The _____ response helps clear cellular debris and promotes tissue repair.
The _____ response helps clear cellular debris and promotes tissue repair.
What is the primary consequence of maladaptive repair following kidney injury?
What is the primary consequence of maladaptive repair following kidney injury?
What is the primary mortality rate for dogs with acute kidney injury (AKI)?
What is the primary mortality rate for dogs with acute kidney injury (AKI)?
Community-acquired AKI presents with early detection due to frequent monitoring.
Community-acquired AKI presents with early detection due to frequent monitoring.
Name one of the syndromes included in the definition of acute kidney injury (AKI) in human medicine.
Name one of the syndromes included in the definition of acute kidney injury (AKI) in human medicine.
In veterinary medicine, AKI is defined as sudden renal parenchymal injury leading to generalized kidney failure to meet __________ demands.
In veterinary medicine, AKI is defined as sudden renal parenchymal injury leading to generalized kidney failure to meet __________ demands.
Match the type of AKI with its description:
Match the type of AKI with its description:
Which of the following options is NOT associated with an increase in mortality in AKI?
Which of the following options is NOT associated with an increase in mortality in AKI?
Ischemia-reperfusion injury is one of the common mechanisms of kidney injury.
Ischemia-reperfusion injury is one of the common mechanisms of kidney injury.
What is the odds ratio for survival when AKI is present?
What is the odds ratio for survival when AKI is present?
Which of the following is a mechanism involved in sepsis-induced acute kidney injury (AKI)?
Which of the following is a mechanism involved in sepsis-induced acute kidney injury (AKI)?
Ischemia-reperfusion injury leads to the production of reactive oxygen species (ROS).
Ischemia-reperfusion injury leads to the production of reactive oxygen species (ROS).
What type of injury is characterized by altered renal hemodynamics and direct tubular epithelial toxicity?
What type of injury is characterized by altered renal hemodynamics and direct tubular epithelial toxicity?
Inflammatory cytokines such as _____ and TNF-a are involved in the ischemia-reperfusion injury cascade.
Inflammatory cytokines such as _____ and TNF-a are involved in the ischemia-reperfusion injury cascade.
Match the type of acute kidney injury with its associated characteristic:
Match the type of acute kidney injury with its associated characteristic:
Which factor is not typically associated with nephrotoxic acute kidney injury?
Which factor is not typically associated with nephrotoxic acute kidney injury?
Maladaptive repair after acute kidney injury can lead to chronic kidney disease (CKD).
Maladaptive repair after acute kidney injury can lead to chronic kidney disease (CKD).
Name one potential consequence of the inflammatory cascade triggered by ischemia-reperfusion injury.
Name one potential consequence of the inflammatory cascade triggered by ischemia-reperfusion injury.
What is the primary cause of pre-renal AKI?
What is the primary cause of pre-renal AKI?
Intrinsic renal AKI is caused by a response to renal hypoperfusion.
Intrinsic renal AKI is caused by a response to renal hypoperfusion.
Name the phase of AKI where uremic effects dominate.
Name the phase of AKI where uremic effects dominate.
The imbalance in __________ delivery to renal tissue can lead to ischemic injury.
The imbalance in __________ delivery to renal tissue can lead to ischemic injury.
Match the type of AKI with its characteristics:
Match the type of AKI with its characteristics:
Which of the following best describes the term 'adaptive repair' in AKI?
Which of the following best describes the term 'adaptive repair' in AKI?
DAMPs primarily recruit leukocytes during the late phase of AKI.
DAMPs primarily recruit leukocytes during the late phase of AKI.
What cellular event occurs due to ATP depletion during ischemia?
What cellular event occurs due to ATP depletion during ischemia?
Ischemia can lead to the production of reactive oxygen species (ROS), resulting in __________ damage.
Ischemia can lead to the production of reactive oxygen species (ROS), resulting in __________ damage.
Which of the following mediators is released during the early phase of inflammation in AKI?
Which of the following mediators is released during the early phase of inflammation in AKI?
The recovery phase of AKI guarantees complete renal function restoration.
The recovery phase of AKI guarantees complete renal function restoration.
Identify one key characteristic of tubular dysfunction in AKI.
Identify one key characteristic of tubular dysfunction in AKI.
Reperfusion injury is primarily associated with the production of __________ species.
Reperfusion injury is primarily associated with the production of __________ species.
Match the phenomenon with its description:
Match the phenomenon with its description:
What is the primary function of M1 macrophages during the first 24-48 hours after injury?
What is the primary function of M1 macrophages during the first 24-48 hours after injury?
M2 macrophages are primarily responsible for the initial inflammatory response in acute kidney injury.
M2 macrophages are primarily responsible for the initial inflammatory response in acute kidney injury.
What do DAMPs and PAMPs signal to in the immune system?
What do DAMPs and PAMPs signal to in the immune system?
The _______ feedback mechanism involves solute delivery to the macula densa.
The _______ feedback mechanism involves solute delivery to the macula densa.
Match the macrophage type with its role during kidney injury:
Match the macrophage type with its role during kidney injury:
Which factors are involved in the tubulo-glomerular feedback mechanism?
Which factors are involved in the tubulo-glomerular feedback mechanism?
Maladaptive repair leads to inflammation, fibrosis, and chronic kidney disease (CKD).
Maladaptive repair leads to inflammation, fibrosis, and chronic kidney disease (CKD).
What is the role of KIM-1 in tubular epithelial cells?
What is the role of KIM-1 in tubular epithelial cells?
M-CSF is produced by _______ after kidney injury.
M-CSF is produced by _______ after kidney injury.
Which cytokines are released by M1 macrophages?
Which cytokines are released by M1 macrophages?
Chronic kidney disease (CKD) primarily develops due to immediate cell death following acute injury.
Chronic kidney disease (CKD) primarily develops due to immediate cell death following acute injury.
Name one consequence of tubule cell stress-induced senescence.
Name one consequence of tubule cell stress-induced senescence.
The initial response to injury is characterized by the activation of ______ macrophages.
The initial response to injury is characterized by the activation of ______ macrophages.
Match the macrophage phase with its function:
Match the macrophage phase with its function:
Flashcards
DAMPs
DAMPs
Damage-associated molecular patterns released from injured tissues.
M1 Macrophages
M1 Macrophages
Activated immune cells that are pro-inflammatory, removing damaged tissue and pathogens in the first 24-48 hours of injury.
M2 Macrophages
M2 Macrophages
Anti-inflammatory immune cells promoting tissue repair and regeneration.
PAMPs
PAMPs
Signup and view all the flashcards
Tubular Leakage
Tubular Leakage
Signup and view all the flashcards
Kidney Injury
Kidney Injury
Signup and view all the flashcards
AKI
AKI
Signup and view all the flashcards
Macrophages (M1)
Macrophages (M1)
Signup and view all the flashcards
Macrophages (M2)
Macrophages (M2)
Signup and view all the flashcards
Tubular Epithelial Cells
Tubular Epithelial Cells
Signup and view all the flashcards
KIM-1
KIM-1
Signup and view all the flashcards
Fibrosis
Fibrosis
Signup and view all the flashcards
Maladaptive repair
Maladaptive repair
Signup and view all the flashcards
Ischemia-induced cell injury
Ischemia-induced cell injury
Signup and view all the flashcards
Reperfusion injury
Reperfusion injury
Signup and view all the flashcards
Sublethal injury to renal tubular cells
Sublethal injury to renal tubular cells
Signup and view all the flashcards
Apoptosis
Apoptosis
Signup and view all the flashcards
Inflammation and AKI
Inflammation and AKI
Signup and view all the flashcards
AKI in Veterinary Practice
AKI in Veterinary Practice
Signup and view all the flashcards
AKI Mortality Rate
AKI Mortality Rate
Signup and view all the flashcards
Why is AKI a Continuum?
Why is AKI a Continuum?
Signup and view all the flashcards
Community-Acquired AKI
Community-Acquired AKI
Signup and view all the flashcards
Hospital-Acquired AKI
Hospital-Acquired AKI
Signup and view all the flashcards
Why 'Acute Kidney Injury' Instead of 'Acute Renal Failure'?
Why 'Acute Kidney Injury' Instead of 'Acute Renal Failure'?
Signup and view all the flashcards
Causes of AKI
Causes of AKI
Signup and view all the flashcards
AKI: Functional Definition
AKI: Functional Definition
Signup and view all the flashcards
Ischemia-Reperfusion Injury (IRI)
Ischemia-Reperfusion Injury (IRI)
Signup and view all the flashcards
Pre-renal AKI
Pre-renal AKI
Signup and view all the flashcards
Intrinsic Renal AKI
Intrinsic Renal AKI
Signup and view all the flashcards
What triggers IRI's inflammatory cascade?
What triggers IRI's inflammatory cascade?
Signup and view all the flashcards
Post-renal AKI
Post-renal AKI
Signup and view all the flashcards
AKI & Sepsis
AKI & Sepsis
Signup and view all the flashcards
AKI & Nephrotoxic Agents
AKI & Nephrotoxic Agents
Signup and view all the flashcards
AKI Phases: Initiation
AKI Phases: Initiation
Signup and view all the flashcards
AKI & Inflammation
AKI & Inflammation
Signup and view all the flashcards
AKI Phases: Extension
AKI Phases: Extension
Signup and view all the flashcards
AKI & Adaptive Repair
AKI & Adaptive Repair
Signup and view all the flashcards
AKI Phases: Maintenance
AKI Phases: Maintenance
Signup and view all the flashcards
AKI & CKD
AKI & CKD
Signup and view all the flashcards
AKI Phases: Recovery
AKI Phases: Recovery
Signup and view all the flashcards
AKI & Maladaptive Repair
AKI & Maladaptive Repair
Signup and view all the flashcards
Microvascular Imbalance in AKI
Microvascular Imbalance in AKI
Signup and view all the flashcards
Tubular Dysfunction in AKI
Tubular Dysfunction in AKI
Signup and view all the flashcards
Cell Death in AKI
Cell Death in AKI
Signup and view all the flashcards
Adaptive Repair in AKI
Adaptive Repair in AKI
Signup and view all the flashcards
Why is the kidney vulnerable to ischemia despite high blood flow?
Why is the kidney vulnerable to ischemia despite high blood flow?
Signup and view all the flashcards
Endothelial Injury in AKI
Endothelial Injury in AKI
Signup and view all the flashcards
ATP Depletion in AKI
ATP Depletion in AKI
Signup and view all the flashcards
DAMPs and PAMPs
DAMPs and PAMPs
Signup and view all the flashcards
Macrophage Phenotypes
Macrophage Phenotypes
Signup and view all the flashcards
Tubulo-Glomerular Feedback (TGF)
Tubulo-Glomerular Feedback (TGF)
Signup and view all the flashcards
TGF & Proximal Tubular Dysfunction
TGF & Proximal Tubular Dysfunction
Signup and view all the flashcards
TGF - Afferent Vasoconstriction
TGF - Afferent Vasoconstriction
Signup and view all the flashcards
Macrophages & Scarring
Macrophages & Scarring
Signup and view all the flashcards
KIM-1 & Macrophages
KIM-1 & Macrophages
Signup and view all the flashcards
Tubular Epithelial Cell Stress
Tubular Epithelial Cell Stress
Signup and view all the flashcards
Senescence & Maladaptive Repair
Senescence & Maladaptive Repair
Signup and view all the flashcards
Tubular Repopulation
Tubular Repopulation
Signup and view all the flashcards
Progenitor Cells & Repair
Progenitor Cells & Repair
Signup and view all the flashcards
Open Question: Tubular Repopulation Source
Open Question: Tubular Repopulation Source
Signup and view all the flashcards
Study Notes
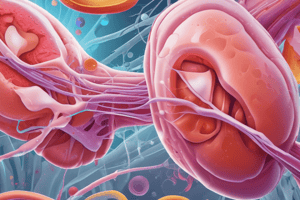
Pathophysiology of Acute Kidney Injury (AKI)
- AKI is defined by a rapid increase in serum creatinine, decrease in urine output, or both.
- AKI is not a single disease, but a collection of syndromes including sepsis, cardiorenal syndrome, and urinary tract obstruction.
- AKI can be community or hospital acquired.
- Community acquired AKI is triggered outside the hospital, with a delay in presentation of a few days.
- Hospital acquired AKI occurs during the period of hospital treatment, and includes frequent monitoring of kidney function markers for early detection.
- In dogs with septic peritonitis, AKI occurs in 40% of cases and is associated with decreased survival odds.
- Mortality rate in dogs with AKI is 39%, versus 9% in dogs without AKI.
Outline: Pathophysiology of AKI
- Definition: Detailed description of AKI
- General pathophysiology of injury: Includes ischemia-reperfusion injury, sepsis, and toxic nephrosis as underlying causes.
- Renal repair: Describes the body's response to repair damage.
- Specific pathophysiology: A breakdown of specifics regarding different causes of AKI.
- Ischemia-reperfusion, sepsis, toxic nephrosis
AKI: Why a new name?
- Functional definition: Uses functional markers such as GFR (glomerular filtration rate) surrogates (creatinine, cystatin C, SDMA), and USG (urine specific gravity).
- Lesional definition: Focuses on injury markers such as urine sediment, casts, renal glucosuria, uGGT (urinary gamma glutamyl transferase), and uNAG (urinary N-acetyl-glucosaminidase).
Pathophysiology - Historical Classification
- Pre-renal AKI: Physiologic response to renal hypoperfusion, without tubular injury.
- Intrinsic renal AKI: Parenchymal injury (glomerular, tubular, vascular, interstitial).
- Post-renal AKI: Impaired flow of urine (obstruction, rupture).
General Pathophysiology – The Phases of AKI
- I - Initiation: Kidney injury initiation.
- II - Extension: Progression of injury.
- III - Maintenance: Kidney function maintained in the face of extensive damage.
- IV - Recovery: Functional recovery with complete return or chronic kidney disease.
Pathophysiology - Five Characteristics
- Microvascular imbalance: Imbalance in vasodilatory and vasoconstrictive factors.
- Tubular dysfunction: Involves obstruction within the tubules.
- Cell death: Apoptosis and necrosis.
- Inflammation: Causes of inflammation are explored.
- Adaptive and maladaptive repair: Body's repair mechanisms in the context of damage.
Endothelial Injury (Microvascular Events)
- Dysbalance between vasodilatory and vasoconstrictive mediators.
- Energy deprivation of endothelium.
- Increased permeability and edema.
- Release of cytokines, chemokines, adhesion molecules.
(Micro-)Vascular Imbalance in AKI
- Imbalance in vasodilatory/vasoconstrictive factors.
- Mismatch between oxygen and nutrient delivery.
- Often regional, not generalized.
- Kidney not a primary organ.
Definition of AKI (hum)
- Fast increase in serum creatinine.
- Decreased urine output
Definition of AKI (vet)
- Spectrum of diseases with sudden onset renal parenchymal injury.
- Generalized failure of the kidney to meet excretory, metabolic, and endocrine demands of the body.
- Rapid hemodynamic, filtration, tubulointerstitial, or outflow injury.
Interstitial Events (Inflammation, Edema)
- Injury (Ischemia) → ATP depletion.
- HIF gene upregulation.
- Generation of ROS.
- Inflammation and recruitment of leukocytes.
Inflammation - Central Role for Macrophages
- Biphasic phenotypes:
- M1 pro-inflammatory: Active during the first 24-48 hours of injury, triggered by DAMPs/PAMPs to eliminate pathogen particles.
- M2 anti-inflammatory: Starts after the initial pro-inflammatory phase. Involved in tissue repair.
Tubulo-Glomerular Feedback
- Proximal tubular dysfunction → increased solute delivery to the macula densa.
- Afferent vasoconstriction and decreased SN-GFR.
- This contributes to oliguria.
Ischemia-Reperfusion Injury (IRI)
- IRI triggers an inflammatory cascade.
- Pro-inflammatory cytokines are activated.
- Inflammatory molecules are expressed.
- Leukocyte infiltration and activation.
- Generation of reactive oxygen species.
Sepsis-Induced AKI
- Combination of mechanisms including ischemia-reperfusion injury, microcirculatory dysfunction, inflammation and metabolic reprogramming.
Kidney predisposed to toxic injury
- High blood supply.
- Filtration and tubular concentration
- Tubular reabsorption
Take home messages
- AKI involves a complex interplay of multiple mechanisms in systemic diseases.
- Inflammation is central, even without infection.
Kidney Repair
- Adaptive repair: restores normal cell function and homeostasis; lost epithelial cells are replaced via proliferation.
- Maladaptive repair: occurs with prolonged or severe injury and results in scarring, inflammation, fibrosis, and CKD progression.
Epithelial-to-mesenchymal transition
- Transition from epithelial cells to mesenchymal cells.
- Occurs in response to inflammation, ischemia and reperfusion.
- Results in accumulation of fibrotic scar tissue.
Antifibrotic strategies
- Therapies targeting the mechanisms causing fibrogenesis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.