Podcast
Questions and Answers
In what 3 ways can caspases be activated?
In what 3 ways can caspases be activated?
- Intrinsic mitochondrial pathway (cytochrome c), 2. Extrinsic receptor-ligand pathway (FAS ligand), 3. Cytotoxic CD8 T cell-mediated pathway (granzyme)
What is Bcl2?
What is Bcl2?
It stabilizes the mitochondrial membrane by binding to bax/bak, in order to inhibit leakage of cytochrome c into the cytosol.
What events lead to the inactivation of Bcl2? What's the consequence?
What events lead to the inactivation of Bcl2? What's the consequence?
Cellular injury, DNA damage, and loss of hormonal stimulation. Inactivation of Bcl2 allows cytochrome c to leak from the inner mitochondrial matrix into the cytoplasm and activate caspases.
What is the extrinsic receptor-ligand pathway? How does CD95 play a role?
What is the extrinsic receptor-ligand pathway? How does CD95 play a role?
What is the cytotoxic CD8 T cell-mediated pathway?
What is the cytotoxic CD8 T cell-mediated pathway?
When does apoptosis occur in aberrant T cell maturation?
When does apoptosis occur in aberrant T cell maturation?
What are the 2 ways a cytotoxic T cell kills cells expressing foreign Ag?
What are the 2 ways a cytotoxic T cell kills cells expressing foreign Ag?
What process is involved in physiologic free radical generation?
What process is involved in physiologic free radical generation?
What enzyme transfers electrons to O2, the final electron acceptor?
What enzyme transfers electrons to O2, the final electron acceptor?
What are the free radicals produced in oxidative phosphorylation? How many accepted electrons does each radical state represent?
What are the free radicals produced in oxidative phosphorylation? How many accepted electrons does each radical state represent?
When does pathologic generation of free radicals arise?
When does pathologic generation of free radicals arise?
How does ionizing radiation generate free radicals?
How does ionizing radiation generate free radicals?
An increase in stress on an organ leads to?
An increase in stress on an organ leads to?
By what three general processes does cellular hypertrophy occur?
By what three general processes does cellular hypertrophy occur?
By what general mechanism does hyperplasia occur?
By what general mechanism does hyperplasia occur?
Is the pregnant uterus an example of hypertrophy or hyperplasia?
Is the pregnant uterus an example of hypertrophy or hyperplasia?
A permanent tissue is one that cannot make new cells (no lingering stem cells/progenitors). Permanent tissues can only grow by ______.
A permanent tissue is one that cannot make new cells (no lingering stem cells/progenitors). Permanent tissues can only grow by ______.
How does the heart respond to persistent hypertension?
How does the heart respond to persistent hypertension?
What concern exists with endometrial hyperplasia?
What concern exists with endometrial hyperplasia?
What are three examples of 'decreases in stress' that lead to atrophy?
What are three examples of 'decreases in stress' that lead to atrophy?
What cellular changes does atrophy represent?
What cellular changes does atrophy represent?
How is cell number decreased in an atrophic process?
How is cell number decreased in an atrophic process?
In what two ways is cell size reduced in atrophy?
In what two ways is cell size reduced in atrophy?
What is ubiquitin-proteosome degradation?
What is ubiquitin-proteosome degradation?
How does autophagy occur in atrophy?
How does autophagy occur in atrophy?
What does a change in stress on an organ lead to?
What does a change in stress on an organ lead to?
What is metaplasia?
What is metaplasia?
Describe the metaplastic process observed in Barrett esophagus.
Describe the metaplastic process observed in Barrett esophagus.
Is metaplasia reversible?
Is metaplasia reversible?
How do you treat Barrett esophagus?
How do you treat Barrett esophagus?
Are we concerned about metaplastic processes?
Are we concerned about metaplastic processes?
Does all metaplasia lead to cancer?
Does all metaplasia lead to cancer?
What processes is vitamin A essential for?
What processes is vitamin A essential for?
Describe the pathological effects of vitamin A deficiency.
Describe the pathological effects of vitamin A deficiency.
What is myositis ossificans?
What is myositis ossificans?
What is dysplasia?
What is dysplasia?
What pathologic proliferation is a precursor to cervical cancer?
What pathologic proliferation is a precursor to cervical cancer?
What processes can precede a dysplastic process?
What processes can precede a dysplastic process?
Is dysplasia reversible?
Is dysplasia reversible?
What is aplasia? Example?
What is aplasia? Example?
What is hypoplasia? Example?
What is hypoplasia? Example?
When does cellular injury occur?
When does cellular injury occur?
Which is more susceptible to ischemic injury: neurons or skeletal myocytes?
Which is more susceptible to ischemic injury: neurons or skeletal myocytes?
How does the rapidity of a stressor affect the response of the cells?
How does the rapidity of a stressor affect the response of the cells?
What are 5 common causes of cellular injury?
What are 5 common causes of cellular injury?
How does hypoxia cause cellular injury?
How does hypoxia cause cellular injury?
What is ischemia?
What is ischemia?
What 3 pathologies/pathologic states can cause ischemia?
What 3 pathologies/pathologic states can cause ischemia?
What is hypoxemia?
What is hypoxemia?
List 4 causes of hypoxemia.
List 4 causes of hypoxemia.
What are 3 general causes of hypoxia in a tissue?
What are 3 general causes of hypoxia in a tissue?
When does decreased O2 carrying capacity arise? Examples?
When does decreased O2 carrying capacity arise? Examples?
How does CO poisoning reduce O2 carrying capacity?
How does CO poisoning reduce O2 carrying capacity?
What are the PaO2 and SaO2 in anemia? CO poisoning?
What are the PaO2 and SaO2 in anemia? CO poisoning?
Common exposures to CO?
Common exposures to CO?
What’s the classic physical finding in CO poisoning?
What’s the classic physical finding in CO poisoning?
What is methemoglobinemia?
What is methemoglobinemia?
PaO2 and SaO2 in methemoglobinemia?
PaO2 and SaO2 in methemoglobinemia?
When does methemoglobinemia occur?
When does methemoglobinemia occur?
What’s the classic finding in methemoglobinemia?
What’s the classic finding in methemoglobinemia?
Tx for methemoglobinemia?
Tx for methemoglobinemia?
What cellular functions does low ATP affect? Consequences?
What cellular functions does low ATP affect? Consequences?
Is cellular injury reversible? What's the hallmark of reversible injury?
Is cellular injury reversible? What's the hallmark of reversible injury?
What histologic findings indicate reversible injury?
What histologic findings indicate reversible injury?
What is the hallmark of irreversible cellular injury?
What is the hallmark of irreversible cellular injury?
What are the consequences of specific membranes in the cell being damaged?
What are the consequences of specific membranes in the cell being damaged?
What is the morphologic hallmark of cell death? How does it occur?
What is the morphologic hallmark of cell death? How does it occur?
What are the 2 mechanisms of cell death?
What are the 2 mechanisms of cell death?
Describe the main differences between necrosis and apoptosis.
Describe the main differences between necrosis and apoptosis.
Describe coagulative necrosis.
Describe coagulative necrosis.
When and where does coagulative necrosis occur?
When and where does coagulative necrosis occur?
How do you recognize an organ that has undergone coagulative necrosis?
How do you recognize an organ that has undergone coagulative necrosis?
When does red infarction arise? Examples?
When does red infarction arise? Examples?
What is liquefactive necrosis?
What is liquefactive necrosis?
When and where does liquefactive necrosis occur?
When and where does liquefactive necrosis occur?
When does acute inflammation arise?
When does acute inflammation arise?
What type(s) of necrosis are associated with the pancreas?
What type(s) of necrosis are associated with the pancreas?
What are the types of necrosis?
What are the types of necrosis?
What is gangrenous necrosis?
What is gangrenous necrosis?
Where does gangrenous necrosis most often occur?
Where does gangrenous necrosis most often occur?
Describe caseous necrotic tissue.
Describe caseous necrotic tissue.
When and where does caseous necrosis occur?
When and where does caseous necrosis occur?
What is fat necrosis?
What is fat necrosis?
When and where does fat necrosis occur?
When and where does fat necrosis occur?
What is dystrophic calcification?
What is dystrophic calcification?
What does fat necrosis have to do with dystrophic calcification?
What does fat necrosis have to do with dystrophic calcification?
What are the serum Ca and P levels in dystrophic calcification? Metastatic calcification?
What are the serum Ca and P levels in dystrophic calcification? Metastatic calcification?
What's the differential for Ca2+ deposits in the breast?
What's the differential for Ca2+ deposits in the breast?
Why might a patient with fat necrosis think they have breast cancer?
Why might a patient with fat necrosis think they have breast cancer?
What is fibrinoid necrosis?
What is fibrinoid necrosis?
How do you identify fibrinoid necrosis?
How do you identify fibrinoid necrosis?
For what two general pathologies can fibrinoid necrosis occur?
For what two general pathologies can fibrinoid necrosis occur?
What is malignant hypertension?
What is malignant hypertension?
What kind of necrosis would pre-eclampsia lead to?
What kind of necrosis would pre-eclampsia lead to?
What is a free radical?
What is a free radical?
What is apoptosis?
What is apoptosis?
Three examples of physiologically appropriate apoptosis?
Three examples of physiologically appropriate apoptosis?
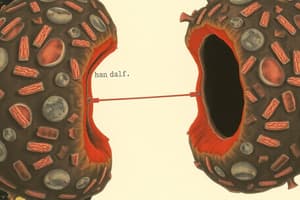
Describe the morphologic changes in the apoptotic process?
Describe the morphologic changes in the apoptotic process?
What are the main enzymatic mediators of apoptosis? How do they work?
What are the main enzymatic mediators of apoptosis? How do they work?
Flashcards
Hypertrophy
Hypertrophy
Increase in cell size due to stress and increased organelle production.
Hyperplasia
Hyperplasia
Increase in cell numbers from stem cells in response to stress.
Cellular Atrophy
Cellular Atrophy
Decrease in cell size and number due to disuse or lack of stimulation.
Metaplasia
Metaplasia
Signup and view all the flashcards
Dysplasia
Dysplasia
Signup and view all the flashcards
Aplasia
Aplasia
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Ischemia
Ischemia
Signup and view all the flashcards
Necrosis
Necrosis
Signup and view all the flashcards
Apoptosis
Apoptosis
Signup and view all the flashcards
Coagulative Necrosis
Coagulative Necrosis
Signup and view all the flashcards
Liquefactive Necrosis
Liquefactive Necrosis
Signup and view all the flashcards
Caseous Necrosis
Caseous Necrosis
Signup and view all the flashcards
Fat Necrosis
Fat Necrosis
Signup and view all the flashcards
Dystrophic Calcification
Dystrophic Calcification
Signup and view all the flashcards
Metastatic Calcification
Metastatic Calcification
Signup and view all the flashcards
Caspases
Caspases
Signup and view all the flashcards
Bcl2
Bcl2
Signup and view all the flashcards
FAS Ligand
FAS Ligand
Signup and view all the flashcards
Oxidative Phosphorylation
Oxidative Phosphorylation
Signup and view all the flashcards
Cytochrome c Oxidase
Cytochrome c Oxidase
Signup and view all the flashcards
Free Radicals
Free Radicals
Signup and view all the flashcards
Ionizing Radiation
Ionizing Radiation
Signup and view all the flashcards
Hydroxyl Radical
Hydroxyl Radical
Signup and view all the flashcards
Study Notes
Cellular Responses to Stress and Injury
- An increase in stress on an organ can lead to hypertrophy or hyperplasia, resulting in increased organ size.
- Cellular hypertrophy occurs through gene activation, increased protein synthesis, and increased organelle production.
- Hyperplasia involves the production of new cells from stem cells.
- The pregnant uterus undergoes both hypertrophy and hyperplasia for growth.
Tissue Types
- Permanent tissues, such as skeletal muscle, cardiac muscle, and nerve, cannot generate new cells and only grow through hypertrophy.
- The heart responds to persistent hypertension with hypertrophy, categorized into concentric (pressure overload) and eccentric (volume overload) growth.
Hyperplasia and Atrophy
- Pathologic hyperplasias, like endometrial hyperplasia caused by excess estrogen, increase cancer risk, unlike benign prostatic hyperplasia (BPH).
- Atrophy occurs due to decreased hormonal stimulation, disuse, or reduced nutrient supply and is characterized by cell size and number reduction through apoptosis.
- Ubiquitin-proteosome degradation and autophagy are cellular processes involved in reducing cell size during atrophy.
Metaplasia
- A change in stress can lead to metaplasia, defined as a transformation of one cell type into another more suitable type, often reversible.
- An example is Barrett esophagus, where squamous epithelium becomes columnar due to acid exposure.
- Metaplasia is concerning as it can progress to dysplasia and cancer.
Dysplasia and Cell Development
- Dysplasia refers to disordered cellular growth and can precede cervical cancer (e.g., cervical intraepithelial neoplasia).
- Aplasia is the failure of cell production during embryogenesis, while hypoplasia is a decreased production resulting in a smaller organ.
Cellular Injury Mechanisms
- Cellular injury occurs when stress surpasses the cell's adaptive capabilities.
- Neurons are more susceptible to ischemic injury than skeletal myocytes, demonstrating rapid response differences to stress.
- Common causes of cellular injury include inflammation, nutritional deficiencies, hypoxia, trauma, and genetic mutations.
Hypoxia and Ischemia
- Hypoxia impairs cellular function by reducing ATP production due to the lack of oxygen as the final electron acceptor.
- Ischemia refers to reduced blood flow to an organ, resulting from arterial perfusion issues, venous drainage challenges, or shock states.
- Hypoxemia is defined as a low arterial oxygen pressure, and can arise from various factors including high altitude and V/Q mismatch.
Cell Death Mechanisms
- Cell death occurs via necrosis (a non-programmed, pathologic process) or apoptosis (a regulated, energy-dependent process).
- Necrosis is associated with inflammation and affects large groups of cells, while apoptosis targets individual cells.
- Various types of necrosis include coagulative, liquefactive, gangrenous, caseous, fat, and fibrinoid necrosis—each with distinct causes and appearances.
Necrosis Types
- Coagulative necrosis preserves organ structure and occurs in ischemic situations, excluding the brain.
- Liquefactive necrosis involves enzymatic breakdown and is often found in the brain, abscesses, and pancreatitis.
- Caseous necrosis appears cheese-like and is seen in tuberculous or fungal infections.
- Fat necrosis results from trauma to adipose tissue or pancreatitis, marked by calcium deposition (saponification).
Dystrophic and Metastatic Calcification
- Dystrophic calcification occurs in necrotic tissue regardless of calcium blood levels, while metastatic calcification involves high calcium levels causing deposits in normal tissues.
Apoptosis Mechanism and Regulation
- Apoptosis involves distinct morphological changes: shrinking cells, eosinophilic cytoplasm, and nuclear condensation and fragmentation.
- Caspases are the key enzymes driving apoptosis, activated through intrinsic, extrinsic, or cytotoxic pathways.
- Bcl2 inhibits apoptosis by stabilizing mitochondrial membranes; its inactivation allows for cytochrome c release, triggering caspase activation.
T Cell Maturation and Killing Mechanisms
- Aberrant T cell maturation leads to apoptosis via negative selection in the thymus.
- Cytotoxic T cells eliminate infected cells using FAS-induced apoptosis or perforin-mediated pathways.### FAS Ligand
- FAS ligand is a cytokine belonging to the TNF (Tumor Necrosis Factor) family.
Physiologic Free Radical Generation
- The process involved in physiologic free radical generation is oxidative phosphorylation.
Electron Transfer to O2
- Cytochrome c oxidase (Complex IV) is the enzyme responsible for transferring electrons to O2, which acts as the final electron acceptor.
- This enzyme's activity can be inhibited by cyanide and carbon monoxide (CO).
Free Radicals in Oxidative Phosphorylation
- O2 accepts one electron to form superoxide (O2-).
- Superoxide can accept an additional electron to become hydrogen peroxide (H2O2).
- Hydrogen peroxide can accept another electron to form hydroxyl radical (*OH).
- Finally, four electrons lead to the formation of water (H2O), which is not considered a free radical.
Pathologic Generation of Free Radicals
- Pathologic generation of free radicals can arise in several scenarios:
- Ionizing radiation.
- Inflammation.
- Accumulation of metals.
- Exposure to drugs and chemicals.
- Reperfusion following ischemic injury.
Mechanism of Ionizing Radiation in Free Radical Generation
- Ionizing radiation generates free radicals by hydrolyzing water, resulting in the formation of hydroxyl free radicals (€¢OH).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.