Podcast
Questions and Answers
What does a non-blanching rash on the buttocks and legs indicate in a child?
What does a non-blanching rash on the buttocks and legs indicate in a child?
- Viral infection
- Dehydration
- Meningococcal Septicaemia (correct)
- Allergic reaction
What is the normal urine output volume for children per kilogram?
What is the normal urine output volume for children per kilogram?
- 60 ml/kg
- 40 ml/kg
- 100 ml/kg
- 80 ml/kg (correct)
Which examination finding is most concerning for Meningococcal Septicaemia?
Which examination finding is most concerning for Meningococcal Septicaemia?
- Increased urine output
- Normal skin color
- Stable heart rate
- Photophobia (correct)
What initial assessment is crucial when determining the level of consciousness in a child?
What initial assessment is crucial when determining the level of consciousness in a child?
What does an increase in work of breathing indicate?
What does an increase in work of breathing indicate?
What anatomical difference contributes to a higher oxygen consumption in infants?
What anatomical difference contributes to a higher oxygen consumption in infants?
When assessing capillary refill time, which reference is most important?
When assessing capillary refill time, which reference is most important?
Which element is NOT included in the Paediatric Assessment Triangle for evaluating appearance?
Which element is NOT included in the Paediatric Assessment Triangle for evaluating appearance?
Which symptom is NOT typically associated with viral infections in children?
Which symptom is NOT typically associated with viral infections in children?
What is the recommended suction pressure for neonates?
What is the recommended suction pressure for neonates?
What is the critical response for a child with stridor and increased work of breathing?
What is the critical response for a child with stridor and increased work of breathing?
Which of the following factors can cause significant heat loss in infants?
Which of the following factors can cause significant heat loss in infants?
What is a common challenge in assessing pain in sick children?
What is a common challenge in assessing pain in sick children?
What assessment tool helps in the early recognition and management of respiratory failure in children?
What assessment tool helps in the early recognition and management of respiratory failure in children?
What is characterized by nasal flaring during breathing in infants?
What is characterized by nasal flaring during breathing in infants?
Which physiological aspect is commonly associated with infants that affects their circulatory status?
Which physiological aspect is commonly associated with infants that affects their circulatory status?
Flashcards
Infant Respiratory Differences
Infant Respiratory Differences
Infants have fewer alveoli (air sacs) in their lungs, weaker intercostal muscles, and use their diaphragm more than adults. They also have a higher metabolic rate and faster respiratory rate.
Infant Circulation Differences
Infant Circulation Differences
Newborns have a smaller blood volume (80ml/kg). This smaller blood volume and lower blood pressure result in a faster heart rate.
Infant Communication Challenges
Infant Communication Challenges
Infants and young children may have limited communication skills, making it hard to express pain, symptoms, or anxiety.
Paediatric Assessment Triangle (PAT)
Paediatric Assessment Triangle (PAT)
Signup and view all the flashcards
Pediatric PAT: Appearance (T.I.C.L.S)
Pediatric PAT: Appearance (T.I.C.L.S)
Signup and view all the flashcards
Airway Assessment in Infant
Airway Assessment in Infant
Signup and view all the flashcards
Heat Loss in Infants
Heat Loss in Infants
Signup and view all the flashcards
Respiratory Rate Assessment in Infants
Respiratory Rate Assessment in Infants
Signup and view all the flashcards
Meningococcal Septicaemia
Meningococcal Septicaemia
Signup and view all the flashcards
Meningitis
Meningitis
Signup and view all the flashcards
Central Nervous System (CNS)
Central Nervous System (CNS)
Signup and view all the flashcards
Assessment for Meningitis
Assessment for Meningitis
Signup and view all the flashcards
Assessment for Sepsis
Assessment for Sepsis
Signup and view all the flashcards
Work of Breathing
Work of Breathing
Signup and view all the flashcards
Stridor
Stridor
Signup and view all the flashcards
Capillary Refill Time (CRT)
Capillary Refill Time (CRT)
Signup and view all the flashcards
Study Notes
Paramedic Science: Health & Human Development 2 - Paediatrics
- Subject: Paramedic Science, Health & Human Development 2, Paediatrics
- Course institution: University of the West of Scotland (UWS)
Anatomical and Physiological Differences
- Children have proportionately larger heads and a larger occiput (the back of the head) compared to adults.
- Infants are obligate nose breathers.
- The larynx is more superior and anterior in children.
- The epiglottis is more cephalic (toward the head), elongated, and flexible in children.
- Mucous membranes are loosely attached in children.
- Cricoid cartilage is the narrowest part of the airway in children.
- Infants and young children rely more on the diaphragm for breathing.
- Infants have a smaller blood volume (approximately 80ml/kg in a 3kg newborn).
- Infants have lower blood pressure and a faster heart rate.
- Infants' larger body surface area to mass ratio increases heat loss.
- Family members may be anxious.
- History of illness may be difficult to establish.
- Children have limited communication skills, making it difficult for them to express pain, symptoms, or anxiety.
Airway
- Larynx is higher and anterior in children.
- Epiglottis is more cephalad, elongated and floppy in children.
- Shape of trachea: Cylindrical in adults, funnel shape in children, and narrowest in the cricoid cartilage.
- Infants and young children use the diaphragm more to breathe than adults.
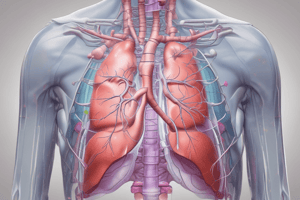
Breathing
- Children have fewer alveoli in their lungs.
- Intercostal muscles are weaker in children.
- Children use the diaphragm more.
- Children have a higher metabolic rate and higher oxygen consumption.
- Children have a faster respiratory rate.
Circulation
- Infant blood volume is approximately 240ml in a 3kg newborn so even small fluid loss is significant.
- Children have lower blood pressure and a faster heart rate.
Disability
- Children have limited communication skills and may have difficulty expressing pain, symptoms, & anxiety.
Exposure/Environment
- Infants have a higher surface area to mass ratio, increasing heat loss.
- Family members may be anxious.
- It may be difficult to obtain a good history of illness in young children.
Assessment Tools
- Paediatric Assessment Triangle (PAT)
- Appearance
- Tone, movement,floppy/listless
- Interactivity, engagement, reactions
- Consolability, comfort by parent/carer
- Gaze, eye contact, 'glassy eyed' behaviour
- Speech/cry, normal, strong, muffled, weak
- Work of Breathing
- Abnormal airway sounds (stridor, grunting, wheezing)
- Abnormal positioning (upright, sniffing position, tripod)
- Recession/head bobbing, nasal flaring
- Circulation
- Skin colour/temperature
- Pulse rate/rhythm/depth
- Heart rate/rhythm
- Capillary refill (centrally & peripherally)
- Disability
- Level of consciousness (AVPU & modified GCS for children < 4), Blood Glucose, Interaction with parent/carer, Pupil response, Posture and tone
- Appearance
- Expose/Examine/Environment
- Temperature
- Rashes?
- Bruising/Injuries?
- Child Protection Concerns?
- NICE 'Traffic Lights' Clinical Assessment Tool.
- Early recognition and management of respiratory and/or circulatory failure to prevent the majority of paediatric cardiac arrests.
Recognizing Respiratory Distress and Failure
- Assess pallor, cyanosis, and mottling in circulation.
Airway (Further Details)
- Is the airway patent?
- Is positional opening required?
- Is suction required? If suction is needed, keep suction pressure less than 200 mmHg in adults and 80-120 mmHg in neonates.
- Are there any abnormal sounds?
- Minimize anxiety in a conscious child.
Breathing (Further Details)
- Respiratory rate? Adequate? Support with BVM required?
- Any chest movement, recession, or tracheal tug?
- Head bobbing or seesaw breathing?
- Auscultate (listen to the lungs)
- Any air entry?
- Any inspiratory/expiratory noises?
- Oxygen administration
- SPO2
Circulation (Further Details)
- Skin color/temperature
- Pulse rate/rhythm/depth
- Heart rate/rhythm
- Capillary refill time, centrally and peripherally
- Blood pressure
- Urine output?
- Fluid loss, haemorrhage? 80ml/kg normal volume. 20% TBL volume considered cat bleed.
Disability (Further Details)
- Level of Consciousness (AVPU & modified GCS for children < 4)
- Blood Glucose
- Interaction with parent/carer
- Pupil response
- Posture and tone
Sick Child Recognition & Management
- Specific scenarios related to sick children, including history and examination findings are described in detail.
- Differentials are presented including viral infection, meningococcal septicaemia, croup, foreign body airway obstruction, epliglottis, and anaphylaxis.
- Treatment pathways for each potential diagnosis are outlined, including the use of the JRCALC guidelines.
Paediatric Trauma
- Children's height, position, and nature of impact result in different injuries that are more severe.
- Children are smaller target areas compared to adults.
- Children have less body fat, more elastic tissue, and a more flexible skeleton and are more susceptible to organ damage.
- Consider the physiological and anatomical differences when managing paediatric trauma.
SUDI
- Unexpected death in infancy, children and adolescents - follow guidelines.
URTI
- Common reasons for paediatric presentation include tonsillitis/pharyngitis/sore throat (1 week), otitis media (4 days), acute rhinosinusitis (2.5 weeks), acute cough/bronchitis (3 weeks).
Epiglottitis
- Rare, severe and rapidly progressing infection of the epiglottis and surrounding tissue.
- Usually bacterial, e.g. Streptococcus group A and C
- Most common in children 1-6 years of age.
- Leads to total airway obstruction.
- High mortality rate (8%).
Statistics
- 700 children die in England and Wales each year. 50% of deaths involve inappropriate restraint and ejection in RTC's. 30% die at home from falls and burns.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.