Podcast
Questions and Answers
What is the underlying mechanism of pancreatitis?
What is the underlying mechanism of pancreatitis?
- Blockage of the common bile duct, preventing enzyme release.
- Autoimmune response targeting pancreatic islet cells.
- Premature activation of pancreatic digestive enzymes causing autodigestion. (correct)
- Increased insulin production leading to cellular damage.
A client presents with severe, constant, knifelike pain in the left upper quadrant radiating to the back. Which condition is most likely indicated by these symptoms?
A client presents with severe, constant, knifelike pain in the left upper quadrant radiating to the back. Which condition is most likely indicated by these symptoms?
- Diverticulitis
- Appendicitis
- Acute pancreatitis (correct)
- Cholecystitis
What is the primary cause associated with chronic calcifying pancreatitis?
What is the primary cause associated with chronic calcifying pancreatitis?
- Hereditary factors
- Alcohol use disorder (correct)
- Autoimmune disorders
- Excessive fat intake
Which of the following strategies is most effective in preventing pancreatitis?
Which of the following strategies is most effective in preventing pancreatitis?
Gallstones causing a blockage where the common bile duct and pancreatic duct meet is a risk factor for which condition?
Gallstones causing a blockage where the common bile duct and pancreatic duct meet is a risk factor for which condition?
An individual with pancreatitis induced by alcohol use disorder should receive which of the following instructions?
An individual with pancreatitis induced by alcohol use disorder should receive which of the following instructions?
What dietary recommendation is most appropriate for a client to prevent acute pancreatitis?
What dietary recommendation is most appropriate for a client to prevent acute pancreatitis?
A nurse is planning care for an older adult with pancreatitis. Which intervention is most important to include?
A nurse is planning care for an older adult with pancreatitis. Which intervention is most important to include?
Which client statement indicates a proper understanding of the dietary changes needed to manage pancreatitis?
Which client statement indicates a proper understanding of the dietary changes needed to manage pancreatitis?
A client with pancreatitis develops hypovolemia. What is the primary cause of this complication?
A client with pancreatitis develops hypovolemia. What is the primary cause of this complication?
A client with a pancreatic pseudocyst has a sump tube for drainage. What nursing action is most important?
A client with a pancreatic pseudocyst has a sump tube for drainage. What nursing action is most important?
What laboratory finding would indicate that a client with pancreatitis has developed type 1 diabetes mellitus?
What laboratory finding would indicate that a client with pancreatitis has developed type 1 diabetes mellitus?
A client with pancreatitis develops left lung effusion and atelectasis. What nursing intervention is most important?
A client with pancreatitis develops left lung effusion and atelectasis. What nursing intervention is most important?
A client with necrotizing hemorrhagic pancreatitis develops disseminated intravascular coagulopathy (DIC). What nursing action is most important?
A client with necrotizing hemorrhagic pancreatitis develops disseminated intravascular coagulopathy (DIC). What nursing action is most important?
A client with necrotizing hemorrhagic pancreatitis is at risk for multi-system organ failure. What assessment finding would indicate the development of this complication?
A client with necrotizing hemorrhagic pancreatitis is at risk for multi-system organ failure. What assessment finding would indicate the development of this complication?
A client with pancreatitis reports severe abdominal pain. Which position should the nurse recommend to best alleviate the client's discomfort?
A client with pancreatitis reports severe abdominal pain. Which position should the nurse recommend to best alleviate the client's discomfort?
A nurse assesses a client with acute pancreatitis. Which finding indicates potential peritonitis?
A nurse assesses a client with acute pancreatitis. Which finding indicates potential peritonitis?
A client with pancreatitis is NPO. Which diet is most appropriate after the client's pain subsides and the diet is advanced?
A client with pancreatitis is NPO. Which diet is most appropriate after the client's pain subsides and the diet is advanced?
A nurse is caring for a client with pancreatitis. Which laboratory value requires immediate intervention?
A nurse is caring for a client with pancreatitis. Which laboratory value requires immediate intervention?
A client with chronic pancreatitis is prescribed pancrelipase. What should the nurse include in client teaching regarding this medication?
A client with chronic pancreatitis is prescribed pancrelipase. What should the nurse include in client teaching regarding this medication?
A nurse is monitoring a client with pancreatitis for signs of hypocalcemia. Which assessment finding indicates a positive Trousseau's sign?
A nurse is monitoring a client with pancreatitis for signs of hypocalcemia. Which assessment finding indicates a positive Trousseau's sign?
Which medication is typically avoided in clients with pancreatitis due to the risk of seizures?
Which medication is typically avoided in clients with pancreatitis due to the risk of seizures?
A client with pancreatitis has developed hyperglycemia. What is the likely cause of this increased blood glucose level?
A client with pancreatitis has developed hyperglycemia. What is the likely cause of this increased blood glucose level?
A nurse reviews a client's medication list and identifies a drug that could contribute to pancreatitis. Which medication is most likely to be implicated?
A nurse reviews a client's medication list and identifies a drug that could contribute to pancreatitis. Which medication is most likely to be implicated?
What is the primary rationale for keeping a client with acute pancreatitis NPO (nothing by mouth)?
What is the primary rationale for keeping a client with acute pancreatitis NPO (nothing by mouth)?
A nurse is assessing a client with suspected pancreatitis. Which type of pain is most consistent with this condition?
A nurse is assessing a client with suspected pancreatitis. Which type of pain is most consistent with this condition?
A client with a history of alcohol abuse is admitted with pancreatitis. What is the priority nursing intervention?
A client with a history of alcohol abuse is admitted with pancreatitis. What is the priority nursing intervention?
A client with pancreatitis also has associated biliary dysfunction. Which laboratory result is expected?
A client with pancreatitis also has associated biliary dysfunction. Which laboratory result is expected?
Which of the following signs indicates Cullen’s sign in a client?
Which of the following signs indicates Cullen’s sign in a client?
What is the purpose of performing an ERCP (endoscopic retrograde cholangiopancreatography) on a client with pancreatitis caused by gallstones?
What is the purpose of performing an ERCP (endoscopic retrograde cholangiopancreatography) on a client with pancreatitis caused by gallstones?
Flashcards
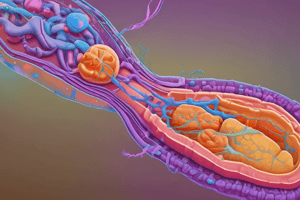
Islets of Langerhans
Islets of Langerhans
Glands in the pancreas that secrete insulin and glucagon, regulating blood sugar.
Pancreatitis
Pancreatitis
Premature activation of pancreatic enzymes causes the pancreas to digest itself.
Pancreatitis Pain
Pancreatitis Pain
Severe, constant, knifelike pain in the upper abdomen, often radiating to the back.
Chronic Pancreatitis
Chronic Pancreatitis
Inflammation and fibrosis of the pancreas, often linked to alcohol use or gallstones.
Signup and view all the flashcards
Pancreatitis Risk Factors
Pancreatitis Risk Factors
Gallstones block the common bile duct and pancreatic duct, or excessive alcohol consumption.
Signup and view all the flashcards
Alcohol Abstinence
Alcohol Abstinence
Abstaining from alcohol is crucial for managing alcohol-induced pancreatitis and preventing further damage.
Signup and view all the flashcards
Pancreatitis Diet
Pancreatitis Diet
Small, frequent meals that are easy to digest and low in fat help minimize pancreatic stimulation.
Signup and view all the flashcards
Hypovolemia in Pancreatitis
Hypovolemia in Pancreatitis
In pancreatitis, fluid can shift into the retroperitoneal space, leading to hypovolemic shock.
Signup and view all the flashcards
Pancreatic Infection
Pancreatic Infection
Infection can occur through leakage of pancreatic fluids, causing fever, pain, and jaundice.
Signup and view all the flashcards
Diabetes Risk
Diabetes Risk
Damage to pancreatic beta cells can result in insulin deficiency and the development of type 1 diabetes.
Signup and view all the flashcards
Lung Complications
Lung Complications
Pancreatic ascites can lead to lung issues like effusion and atelectasis, possibly leading to pneumonia.
Signup and view all the flashcards
Coagulation Defects
Coagulation Defects
Necrotizing hemorrhagic pancreatitis can release thromboplastic endotoxins, causing DIC and coagulation issues.
Signup and view all the flashcards
Organ Failure Risk
Organ Failure Risk
Severe pancreatitis can cause systemic inflammation, leading to multi-system organ failure.
Signup and view all the flashcards
Lab Values
Lab Values
Elevated amylase and lipase levels confirm pancreatic inflammation; WBC, glucose, liver enzymes, and bilirubin may also increase.
Signup and view all the flashcards
Grey Turner's Sign
Grey Turner's Sign
Ecchymoses (bruising) on the flanks, indicating blood seepage from pancreatic enzyme action.
Signup and view all the flashcards
Cullen's Sign
Cullen's Sign
Bluish-gray discoloration around the umbilicus, indicating blood in the abdominal wall.
Signup and view all the flashcards
Serum Amylase in Pancreatitis
Serum Amylase in Pancreatitis
Elevated serum amylase indicates pancreatic cell damage, usually peaking within 24 hours.
Signup and view all the flashcards
Blood Lipase in Pancreatitis
Blood Lipase in Pancreatitis
Blood lipase increases slower than amylase but remains elevated longer, indicating pancreatic damage.
Signup and view all the flashcards
Calcium Levels in Pancreatitis
Calcium Levels in Pancreatitis
Decreased blood calcium levels due to fat necrosis that occurs with pancreatitis.
Signup and view all the flashcards
Blood Glucose in Pancreatitis
Blood Glucose in Pancreatitis
Increased blood glucose levels that happen because of decreased insulin production.
Signup and view all the flashcards
Pancreatitis Initial Treatment
Pancreatitis Initial Treatment
Rest the pancreas by keeping the patient NPO (nothing by mouth) until pain-free.
Signup and view all the flashcards
Comfort Positioning for Pancreatitis
Comfort Positioning for Pancreatitis
Side-lying, fetal, head-of-bed elevated, or leaning forward positions to relieve pain.
Signup and view all the flashcards
Pain Medications for Pancreatitis
Pain Medications for Pancreatitis
Opioid analgesics like morphine or hydromorphone; NSAIDs like ketorolac for pain relief.
Signup and view all the flashcards
H2 Receptor Antagonists (Cimetidine)
H2 Receptor Antagonists (Cimetidine)
Decreases acid secretion. Take 1 hour apart from antacids.
Signup and view all the flashcards
Proton Pump Inhibitors (Omeprazole)
Proton Pump Inhibitors (Omeprazole)
Decreases gastric acid secretion; monitor for hypomagnesemia.
Signup and view all the flashcards
Pancreatic Enzyme Supplements (Pancrelipase)
Pancreatic Enzyme Supplements (Pancrelipase)
Take with meals to aid digestion. Sprinkled on nonprotein foods and drink with water.
Signup and view all the flashcards
ERCP for Pancreatitis
ERCP for Pancreatitis
To open the sphincter of Oddi which can be done if gallstones are the cause.
Signup and view all the flashcardsStudy Notes
- Pancreatitis involves the autodigestion of the pancreas by its own digestive enzymes, which get activated prematurely.
- Each year, approximately 275,000 cases of pancreatitis occur in the United States, with a mortality rate of 1.6 per 100,000.
- Inflammation in the pancreas leads to duct obstruction, increased pressure, and potential rupture, causing enzyme release into pancreatic tissue.
- Pancreatitis can cause inflammation, necrosis, and hemorrhage within the pancreas.
- Acute pancreatitis is an inflammatory process resulting from activated pancreatic enzymes digesting the pancreas, varying from mild to severe necrotizing hemorrhagic pancreatitis.
- Chronic pancreatitis is a progressive disease involving inflammation and fibrosis of the pancreas categorized as chronic calcifying, chronic obstructive, autoimmune, idiopathic, or hereditary.
Health Promotion and Disease Prevention
- Avoid excessive alcohol consumption.
- Maintain a low-fat diet.
Risk Factors
- Gallstones can block the meeting point of the common bile duct and pancreatic duct.
- The primary cause of chronic pancreatitis is alcohol use disorder.
- Increased alcohol consumption during vacations or holidays is linked to acute pancreatitis.
- ERCP can be a postprocedure complication.
- Other risk factors include gastrointestinal surgery, metabolic disturbances like hyperlipidemia and hypercalcemia, kidney failure or transplant, genetic predisposition, trauma, penetrating ulcers, medication toxicity, viral infections like coxsackievirus B and HIV, cigarette smoking.
Expected Findings
- Symptoms include a sudden onset of severe, constant pain described as "boring" that goes through the body.
- Pain is typically epigastric, radiating to the back, left flank, or left shoulder.
- Lying down worsens the pain.
- Eating may worsen discomfort, particularly in acute cases.
- Relief can be found by assuming a fetal position or sitting upright and bending forward.
- Other symptoms include nausea, vomiting, and weight loss.
Physical Findings
- Ecchymoses (bruising) may appear on the flanks due to blood-stained exudates seeping into tissues.
- Cullen’s sign presents as a bluish-gray discoloration around the umbilicus.
- The abdomen may be distended and rigid, indicating peritonitis.
- Generalized jaundice may be observed.
- Bowel sounds may be absent or decreased, suggesting paralytic ileus.
- Warm, moist skin and fruity breath can indicate hyperglycemia.
- Hypocalcemia may lead to tetany.
- Trousseau’s sign manifests as a hand spasm when a blood pressure cuff is inflated.
- Chvostek’s sign is facial twitching when the facial nerve is tapped.
Laboratory Tests
- Serum amylase levels increase within 24 hours and remain elevated for 2 to 3 days; persistent elevation may indicate a pancreatic abscess or pseudocyst.
- Blood lipase increases slowly and remains elevated longer than amylase.
- Urine amylase can remain elevated for up to 1 week.
- Elevated enzyme levels indicate pancreatic cell injury.
- White blood cell count is increased due to infection and inflammation.
- Platelet count is decreased.
- Blood calcium and magnesium levels are decreased due to fat necrosis.
- Blood liver enzymes and bilirubin are increased with biliary dysfunction.
- Blood glucose is increased due to decreased insulin production.
- Erythrocyte sedimentation rate is elevated.
Diagnostic Procedures
- A CT scan with contrast is a reliable diagnostic tool for acute pancreatitis.
Nursing Care
- Rest the Pancreas
- Keep the patient NPO until pain-free.
- For severe cases, consider enteral or parenteral nutrition.
- When resuming diet, offer bland, high-protein, low-fat foods without stimulants like caffeine, served in small, frequent meals.
- Administer antiemetics as needed.
- Use a nasogastric tube for gastric decompression in cases of severe vomiting or paralytic ileus.
- No alcohol consumption or smoking.
- Limit stress
Pain Management
- Position the patient for comfort, such as in a fetal position, side-lying, with the head of the bed elevated, or sitting up and leaning forward.
- Administer prescribed analgesics and other medications.
- Monitor respiratory status and vital signs.
- Monitor blood glucose levels and administer insulin as needed.
- Monitor hydration status.
- Monitor IV fluids and electrolyte replacements.
Medications
- Opioid analgesics
- Morphine or hydromorphone manage acute pain.
- Meperidine is discouraged due to the risk of seizures, especially in older adults.
- Histamine Receptor Antagonists:
- Cimetidine decreases gastric acid secretion.
- Take 1 hour before or after antacids.
- Proton Pump Inhibitors:
- Omeprazole decreases gastric acid secretion.
- Monitor for hypomagnesemia.
- Pancreatic Enzymes:
- Pancrelipase aids in digestion of fats and proteins when taken with meals and snacks.
Pancrelipase
- Monitor and report any persistent side effects like headache, cough, dizziness, or sore throat.
- Contents of capsules can be sprinkled on nonprotein foods.
- Drink a full glass of water after taking pancrelipase.
- Wipe lips and rinse mouth after taking medication.
- Take pancrelipase after antacid or histamine receptor antagonists.
- Take pancrelipase with every meal and snack.
Therapeutic Procedures
- ERCP creates an opening in the sphincter of Oddi if gallstones cause pancreatitis.
Interprofessional Care
- Dietary referral for postpancreatitis diet and nutritional supplements when oral intake is resumed.
- Home health services for nutritional needs, wound care, and assistance with ADLs.
- Substance-related support groups for clients or family members with alcohol use disorder.
Client Education
- Abstain from alcohol if pancreatitis is induced by alcohol use disorder.
- Avoid high-fat foods or heavy meals to prevent acute pancreatitis.
Complications
- Hypovolemia
- Up to 6 L of fluid can be third-spaced due to retroperitoneal loss.
- Monitor electrolytes, hypotension, and tachycardia.
- Assist with IV fluid and electrolyte replacement.
Pancreatic infection
- Pseudocyst (outside pancreas); abscess (inside pancreas)
- Leakage of fluid out of damaged pancreatic duct
- Manifestations: Fever, epigastric mass, nausea, vomiting, jaundice
- Monitor for rupture and hemorrhage.
- Maintain sump tube if placed for drainage of cyst.
- Monitor skin around tube for breakdown.
Type 1 Diabetes Mellitus
- Lack or absence of insulin (due to destruction of pancreatic beta cells)
- Monitor blood glucose and administer insulin.
Left Lung Effusion and Atelectasis
- Can precipitate pneumonia
- Causes: Pancreatic ascites
- Monitor for hypoxia and assist with ventilatory support.
Coagulation Defects
- Disseminated intravascular coagulopathy
- Causes: Release of thromboplastic endotoxins
- Monitor coagulation studies and for bleeding.
Multi-System Organ Failure
- Inflammation of pancreas is believed to trigger systemic inflammation
- Cause: Necrotizing hemorrhagic pancreatitis
- Administer treatments and monitor for organ failure.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.