Podcast
Questions and Answers
Which of the following is most commonly associated with chronic pain?
Which of the following is most commonly associated with chronic pain?
- Short-lived pain responses
- Sudden onset and immediate resolution
- Irregular sleep patterns and fatigue (correct)
- Protection against future injuries
What type of pain is typically caused by direct stimulation of nerve endings due to tissue injury?
What type of pain is typically caused by direct stimulation of nerve endings due to tissue injury?
- Mixed pain
- Nociceptive pain (correct)
- Dysfunctional pain
- Neuropathic pain
Which statement about neuropathic pain is true?
Which statement about neuropathic pain is true?
- It is solely caused by inflammation.
- It may occur without any identifiable noxious stimulus. (correct)
- It implies normal functioning of the nervous system.
- It usually correlates well with the level of injury.
Which pain management strategy would be least effective for someone experiencing chronic pain?
Which pain management strategy would be least effective for someone experiencing chronic pain?
What typically characterizes visceral pain mechanisms?
What typically characterizes visceral pain mechanisms?
What type of pain is typically associated with mechanical, thermal, and chemical nociceptors?
What type of pain is typically associated with mechanical, thermal, and chemical nociceptors?
What is a common characteristic of visceral pain?
What is a common characteristic of visceral pain?
Which of the following best describes referred pain?
Which of the following best describes referred pain?
Which pain management strategy utilizes the gate control mechanism?
Which pain management strategy utilizes the gate control mechanism?
Which condition is classified under neuropathic pain?
Which condition is classified under neuropathic pain?
What type of pain is often described as a deep dull ache associated with joints?
What type of pain is often described as a deep dull ache associated with joints?
In which scenario might nociceptor sensitization occur?
In which scenario might nociceptor sensitization occur?
How do enkephalinergic interneurons function in pain modulation?
How do enkephalinergic interneurons function in pain modulation?
What role do PAG neurons play in pain modulation?
What role do PAG neurons play in pain modulation?
What is a characteristic feature of visceral pain?
What is a characteristic feature of visceral pain?
Which of the following explains referred pain?
Which of the following explains referred pain?
What is a primary mechanism behind neuropathic pain?
What is a primary mechanism behind neuropathic pain?
How do opioids inhibit pain transmission at the spinal cord level?
How do opioids inhibit pain transmission at the spinal cord level?
What might cause the emotional reactions associated with visceral pain?
What might cause the emotional reactions associated with visceral pain?
Which condition is most commonly associated with central neuropathic pain?
Which condition is most commonly associated with central neuropathic pain?
Which statement describes a characteristic of neuropathic pain?
Which statement describes a characteristic of neuropathic pain?
What is the effect of the decrease in inhibitory interneurons on pain?
What is the effect of the decrease in inhibitory interneurons on pain?
How does central sensitization affect pain pathways?
How does central sensitization affect pain pathways?
Flashcards are hidden until you start studying
Study Notes
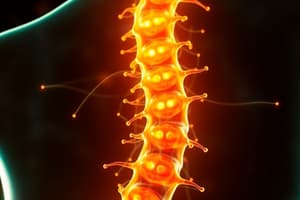
PAG Neurons and Pain Modulation
- PAG neurons release opioids upon stimulation, which travel to the RVM and activate serotonergic neurons in the nucleus raphe magnus.
- These activated neurons in the RVM can directly inhibit pain sensation by acting on ascending pathway neurons in the dorsal horn of the spinal cord.
- Alternatively, they can indirectly inhibit pain by activating local inhibitory interneurons in the dorsal horn, which release enkephalin.
- Enkephalin binds to opioid receptors on first-order neurons, inhibiting the release of Substance P, CGRP, and glutamate, thus reducing pain signal transmission to second-order neurons.
- Enkephalin can also bind to second-order neurons, indirectly activating potassium channels, leading to hyperpolarization and reduced impulse transmission, further lowering pain perception.
Visceral Pain
- Distension-sensitive nociceptors are primarily involved in visceral pain, while other types of pain receptors are less prevalent.
- Visceral pain presents as complex, diffuse and poorly localized, often referred to somatic regions.
- The severity of visceral pain may not accurately reflect the severity of the underlying disease.
- Visceral pain arises from internal organ dysfunction due to factors such as stretching, obstruction, spasm, traction, tumor invasion, ischemia, or inflammation.
- Strong emotional responses are associated with visceral pain, involving vagal and spinal activation of the anterior cingulate cortex.
- Exaggerated autonomic responses, such as abdominal wall spasm, nausea, vomiting, sweating, and blood pressure changes, may accompany visceral pain.
Referred Pain
- Referred pain is pain perceived in a location different from its actual origin.
- This phenomenon occurs when afferents from the painful organ and the referred pain site converge onto the same sensory projection neurons in the dorsal root ganglia.
- The brain misinterprets the source due to this convergence and projects the pain signal to the somatic site.
Neuropathic Pain
- Neuropathic pain arises from lesions or diseases affecting the somatosensory system.
- It results from imbalances in excitatory and inhibitory somatosensory signaling, leading to hyperexcitability.
- This hyperexcitability is due to altered ion channels and changes in second-order nociceptive neurons, which become activated by Aβ, δ and C afferents, transmitting heightened sensory information to the central nervous system.
- Central sensitization, characterized by increased NMDA/AMPA receptor activity and a loss of GABA-releasing interneurons, contributes to pain amplification in neuropathic pain.
- Impaired inhibitory modulation of pain signals in the CNS is another characteristic of neuropathic pain.
- Reduced inhibitory interneuron activity in the brain contributes to co-morbidities like anxiety, depression, and sleep problems.
Types of Pain
- Acute Pain: Sudden onset, resolves after healing or intervention, associated with autonomic hyperactivity.
- Chronic Pain: Pain lasting longer than 3-6 months; irritability, fatigue, concentration difficulties, anxiety, insomnia, and depression are common.
- Nociceptive Pain: Pain triggered by tissue injury, either somatic or visceral.
- Neuropathic Pain: Pain arising from neurological damage, either central or peripheral.
- Inflammatory Pain: Nociceptor sensitization due to inflammation, leading to primary or secondary hyperalgesia.
- Dysfunctional Pain: Pain without a discernible noxious stimulus or identifiable inflammation or damage.
- Mixed Pain: Pain involving multiple pain mechanisms.
Somatic Nociceptive Pain
- Involves mechano-, thermo-, chemo-, and polymodal nociceptors.
- Superficial pain arises from the skin and subcutaneous tissues, characterized by tingling, sharpness, cutting, or burning sensations.
- Deep pain originates from muscles, tendons, ligaments, bones, joints, and arteries, presenting as a more diffuse pain radiating to nearby areas.
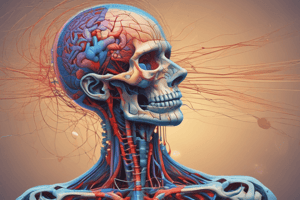
Pain Processing Pathways
- Pain is relayed to the brain through ascending pathways, primarily the spinothalamic tract.
Gate Control Mechanism
- This mechanism describes how various factors can influence the experience of pain.
- Stimulation of non-noxious, large sensory afferents from the skin can activate lamina II inhibitory opiateergic interneurons, which block pain signals by inhibiting the projection neuron.
- This explains why rubbing a painful area can alleviate pain.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.