Podcast
Questions and Answers
A client exhibits labored breathing, increased anxiety, and confusion. An arterial blood gas (ABG) reveals a PaO2 of 55 mm Hg. Which condition is most consistent with these findings?
A client exhibits labored breathing, increased anxiety, and confusion. An arterial blood gas (ABG) reveals a PaO2 of 55 mm Hg. Which condition is most consistent with these findings?
- Hypercarbia
- Hyperventilation
- Hypoxemia (correct)
- Respiratory alkalosis
An older adult is admitted with community-acquired pneumonia. Which assessment finding would prompt the nurse to consider the presence of inadequate oxygenation, rather than delirium or dementia?
An older adult is admitted with community-acquired pneumonia. Which assessment finding would prompt the nurse to consider the presence of inadequate oxygenation, rather than delirium or dementia?
- Rapid, shallow breathing (correct)
- Confusion
- Restlessness
- Decreased energy
A client with chronic obstructive pulmonary disease (COPD) is being discharged home on oxygen. What is the most important teaching point regarding oxygen administration?
A client with chronic obstructive pulmonary disease (COPD) is being discharged home on oxygen. What is the most important teaching point regarding oxygen administration?
- Administer oxygen at the prescribed flow rate, even if breathing improves. (correct)
- Increase oxygen flow during periods of shortness of breath.
- Maintain the oxygen saturation above 95% at all times.
- Adjust the oxygen flow rate based on comfort level.
A client is receiving oxygen via a nonrebreather mask. Which assessment requires immediate intervention?
A client is receiving oxygen via a nonrebreather mask. Which assessment requires immediate intervention?
During the change of shift report, the nurse learns that a client has a PaCO2 of 60 mm Hg. How should the nurse interpret this information?
During the change of shift report, the nurse learns that a client has a PaCO2 of 60 mm Hg. How should the nurse interpret this information?
A client with a history of asthma is admitted for acute respiratory distress. Which nursing intervention is most important to include in the plan of care to promote effective ventilation?
A client with a history of asthma is admitted for acute respiratory distress. Which nursing intervention is most important to include in the plan of care to promote effective ventilation?
A nurse is caring for a post-operative client who is at risk for developing atelectasis. Which intervention is most effective in preventing this complication?
A nurse is caring for a post-operative client who is at risk for developing atelectasis. Which intervention is most effective in preventing this complication?
A nurse is preparing to administer oxygen to a client with a suspected diagnosis of pneumonia. What is the most important safety measure to implement?
A nurse is preparing to administer oxygen to a client with a suspected diagnosis of pneumonia. What is the most important safety measure to implement?
When caring for a client receiving oxygen via a simple mask, which action should the nurse take to ensure client safety?
When caring for a client receiving oxygen via a simple mask, which action should the nurse take to ensure client safety?
A client with a tracheostomy is receiving oxygen via a tracheostomy collar. What is the priority nursing action?
A client with a tracheostomy is receiving oxygen via a tracheostomy collar. What is the priority nursing action?
A nurse is teaching a client how to use an incentive spirometer. Which instruction is most important to ensure the client performs the technique correctly?
A nurse is teaching a client how to use an incentive spirometer. Which instruction is most important to ensure the client performs the technique correctly?
A client is scheduled for a thoracentesis. What should the nurse emphasize when educating the client about the procedure?
A client is scheduled for a thoracentesis. What should the nurse emphasize when educating the client about the procedure?
A client with a pneumothorax has a chest tube connected to a water-seal drainage system. Which finding requires immediate intervention by the nurse?
A client with a pneumothorax has a chest tube connected to a water-seal drainage system. Which finding requires immediate intervention by the nurse?
A nurse is caring for a client with carbon monoxide poisoning. Which intervention would be most effective in reversing the effects of this condition?
A nurse is caring for a client with carbon monoxide poisoning. Which intervention would be most effective in reversing the effects of this condition?
A client with a history of sleep apnea is prescribed continuous positive airway pressure (CPAP) therapy. What should the nurse emphasize when educating the client about this treatment?
A client with a history of sleep apnea is prescribed continuous positive airway pressure (CPAP) therapy. What should the nurse emphasize when educating the client about this treatment?
The provider orders an arterial blood gas (ABG) to be drawn on a client. Prior to arterial puncture, what assessment should the nurse perform?
The provider orders an arterial blood gas (ABG) to be drawn on a client. Prior to arterial puncture, what assessment should the nurse perform?
A nurse is providing discharge instructions to a client with a new prescription for home oxygen therapy. Which statement by the client indicates a need for further teaching?
A nurse is providing discharge instructions to a client with a new prescription for home oxygen therapy. Which statement by the client indicates a need for further teaching?
A client is diagnosed with oxygen toxicity secondary to prolonged high FIO2. Which intervention by the nurse is a priority?
A client is diagnosed with oxygen toxicity secondary to prolonged high FIO2. Which intervention by the nurse is a priority?
A nurse is caring for a client with a nasal cannula. Which assessment finding requires intervention by the nurse?
A nurse is caring for a client with a nasal cannula. Which assessment finding requires intervention by the nurse?
A client returns to the unit after a surgical procedure. Which is the first action the nurse should take?
A client returns to the unit after a surgical procedure. Which is the first action the nurse should take?
A nurse is caring for a client with a water-seal chest tube drainage system. Which action will the nurse take?
A nurse is caring for a client with a water-seal chest tube drainage system. Which action will the nurse take?
A nurse is caring for a client with a chest tube who is scheduled to ambulate. Prior to ambulating, what intervention is required by the nurse?
A nurse is caring for a client with a chest tube who is scheduled to ambulate. Prior to ambulating, what intervention is required by the nurse?
The provider orders a nurse to administer oxygen at 100% FIO2. Which oxygen delivery device is appropriate to administer this level of oxygen?
The provider orders a nurse to administer oxygen at 100% FIO2. Which oxygen delivery device is appropriate to administer this level of oxygen?
A nurse is caring for a client with COPD who is showing symptoms of hypoxemia. Which action by the nurse is appropriate?
A nurse is caring for a client with COPD who is showing symptoms of hypoxemia. Which action by the nurse is appropriate?
A client is showing signs of poor oxygenation and increased carbon dioxide and the provider orders the the nurse to administer oxygen. The nurse understands the administration of oxygen can be dangerous for this client. What does the client potentially has?
A client is showing signs of poor oxygenation and increased carbon dioxide and the provider orders the the nurse to administer oxygen. The nurse understands the administration of oxygen can be dangerous for this client. What does the client potentially has?
The doctor tells the nurse to start the client on 2L of oxygen by nasal cannula. What action is required by the nurse before administering the oxygen?
The doctor tells the nurse to start the client on 2L of oxygen by nasal cannula. What action is required by the nurse before administering the oxygen?
A nurse draws an arterial blood gas on a restless client. What information must be noted by the nurse?
A nurse draws an arterial blood gas on a restless client. What information must be noted by the nurse?
When administering oxygen, what is the most important step?
When administering oxygen, what is the most important step?
Flashcards
Inspiration
Inspiration
Process of breathing in to fill the lungs with air.
Expiration
Expiration
Process of breathing out, expelling air from the lungs.
Ventilation
Ventilation
Movement of air in and out of the lungs, facilitating respiration.
Respiration
Respiration
Signup and view all the flashcards
External Respiration
External Respiration
Signup and view all the flashcards
Internal Respiration
Internal Respiration
Signup and view all the flashcards
Hypoxemia
Hypoxemia
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Arterial Blood Gas (ABG)
Arterial Blood Gas (ABG)
Signup and view all the flashcards
Pulse Oximetry
Pulse Oximetry
Signup and view all the flashcards
SaO2
SaO2
Signup and view all the flashcards
PaO2
PaO2
Signup and view all the flashcards
High Fowler Position
High Fowler Position
Signup and view all the flashcards
Tripod Position
Tripod Position
Signup and view all the flashcards
Orthopneic Position
Orthopneic Position
Signup and view all the flashcards
Deep Breathing
Deep Breathing
Signup and view all the flashcards
Incentive Spirometry
Incentive Spirometry
Signup and view all the flashcards
Pursed-Lip Breathing
Pursed-Lip Breathing
Signup and view all the flashcards
Diaphragmatic Breathing
Diaphragmatic Breathing
Signup and view all the flashcards
Oxygen Therapy
Oxygen Therapy
Signup and view all the flashcards
Oxygen Analyzer
Oxygen Analyzer
Signup and view all the flashcards
Humidifier
Humidifier
Signup and view all the flashcards
Nasal Cannula
Nasal Cannula
Signup and view all the flashcards
Simple Mask
Simple Mask
Signup and view all the flashcards
Partial Rebreather Mask
Partial Rebreather Mask
Signup and view all the flashcards
Nonrebreather Mask
Nonrebreather Mask
Signup and view all the flashcards
Venturi Mask
Venturi Mask
Signup and view all the flashcards
Oxygen Toxicity
Oxygen Toxicity
Signup and view all the flashcards
Positive Airway Pressure (PAP)
Positive Airway Pressure (PAP)
Signup and view all the flashcards
Water-Seal Chest Tube Drainage
Water-Seal Chest Tube Drainage
Signup and view all the flashcards
Study Notes
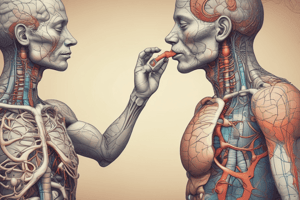
Oxygenation Overview
- Oxygen, constituting about 21% of Earth's atmosphere, is vital for human life.
- Cells use oxygen to metabolize nutrients and produce energy.
- Without oxygen, cells quickly die.
Learning Objectives
- Explain the difference between ventilation and respiration.
- Differentiate between external and internal respiration.
- Name methods for assessing the oxygenation status of clients at the bedside.
- List signs of inadequate oxygenation.
- Name nursing interventions that can be used to improve ventilation and oxygenation.
- Name sources for supplemental oxygen.
- Identify items that may be needed when providing oxygen therapy.
- List common oxygen delivery devices.
- Discuss hazards related to the administration of oxygen.
- Describe additional therapeutic techniques that relate to oxygenation.
- Discuss facts concerning oxygenation that affect the care of older adults.
Gerontologic Considerations
- Age-related changes can decrease gas exchange and ventilation efficiency.
- Functional respiratory changes in older adults include diminished cough and gag reflexes.
- Older adults may use accessory muscles more for breathing.
- Diminished efficiency of gas exchange in the lungs is possible with age.
- Increased mouth breathing and snoring may be observed.
- Lung volume changes can decrease overall efficiency and raise energy expenditure.
- Confusion or restlessness needs assessment to rule out oxygen deficit before assuming delirium or dementia.
- Encourage older adults needing home oxygen to socialize.
- Educate older adults and caregivers on portable oxygen.
- Check behind older adults' ears for skin breakdown from oxygen tubes/devices.
- Older adults may have facial seal issues with masks from weight loss/denture use.
- Advise annual flu and pneumonia immunization, with possible booster pneumonia dose after 5 years.
Anatomy and Physiology of Breathing
- Lung tissue elasticity allows expansion during inspiration and returning to a resting position with expiration.
- Ventilation is the air movement in/out of lungs, aiding respiration.
- Respiration is the oxygen and carbon dioxide exchange.
- External respiration happens between alveoli and capillaries.
- Internal respiration occurs at the cellular level involving hemoglobin and body cells.
- Increased blood carbon dioxide and hydrogen ions stimulate breathing.
- Ventilation is due to pressure changes in the thoracic cavity.
- During inspiration, the diaphragm goes down and intercostals move chest out.
- Expansion creates more chest space, decreasing lung pressure below atmospheric.
- Air is pulled in through the nose and lungs.
- Accessory muscles (pectoralis minor and sternocleidomastoid) help with greater chest expansion.
- During inspiration, chest cavity increases, but chest pressure decreases, allowing air to move into the lungs.
- Respiratory muscles relax and the thoracic cavity decreases during expiration.
- Intrathoracic pressure increases and air exits the respiratory tract.
- Contraction of abdominal muscles can forcibly exhale additional air.
Assessing Oxygenation
- Assess the quality of a client's oxygenation through physical assessment, arterial blood gases (ABGs), and pulse oximetry.
- These measures help identify hypoxemia and hypoxia.
- Hypoxemia is insufficient oxygen in arterial blood.
- Hypoxia is inadequate oxygen at the cellular level.
Physical Assessment
- Monitor respiratory rate.
- Observe breathing pattern and effort.
- Check chest symmetry.
- Auscultate lung sounds.
- Record heart rate and blood pressure.
- Determine consciousness level.
- Observe skin, mucous membranes, lips, and nail bed color.
Arterial Blood Gases (ABG)
- ABG assessment is a lab test to assess oxygenation, ventilation, and acid-base balance.
- ABGs measure PaO2, SaO2, PaCO2, blood pH, and bicarbonate (HCO3) levels.
- Arterial blood is preferred because arteries carry oxygen to all cells.
- ABGs are ordered to assess clients in respiratory distress or monitor medical treatment progress.
- A laboratory technician and nurse collaboratively collect arterial blood.
- The nurse notifies the laboratory of the need for the blood test.
- The nurse records assessments on the request form.
- The nurse prepares the client and assists the technician.
- Measures prevent complications after arterial puncture.
- A nurse trained in arterial punctures may obtain the specimen in emergencies.
Common Signs of Inadequate Oxygenation
- Decreased energy
- Restlessness
- Rapid, shallow breathing
- Rapid heart rate
- Sitting up to breathe
- Nasal flaring
- Use of accessory muscles
- Hypertension
- Sleepiness, confusion, stupor, coma
Pharmacologic Considerations
- Assess all clients under 5 years of age, over 65 years, or anyone with a compromising chronic health condition for and offer Prevnar 13.
Arterial Blood Gas Procedure
- Perform Allen test before arterial puncture.
- Flex client's elbow and elevate forearm.
- Simultaneously compress radial and ulnar arteries.
- Client opens/closes fist until palm blanches.
- Release ulnar pressure, keeping radial pressure.
- Observe skin for flush/blanch.
- Release radial pressure.
- Allen test verifies adequate ulnar blood supply if radial artery damage occurs.
- Do not puncture radial artery if Allen test shows poor collateral flow.
- Alternative sites: brachial, femoral, or dorsalis pedis arteries.
- Keep client at rest for at least 30 minutes before unless an emergency, as activity can transiently lower oxygen.
- Record client's temperature, respiratory rate, and activity level, as increased metabolism/activity affects results.
- Record oxygen amount at test time and ventilator settings to help determine effectiveness.
- Hyperextend wrist over rolled towel for artery access.
- Comfort the client during puncture since it can be painful without local anesthetic.
- Expel air bubbles from specimen to ensure only contained gas is present.
- Rotate collected specimen to mix with anticoagulant and prevent clotting.
- Place specimen on ice immediately because cell deterioration affects oxygen content.
- Cool sample slows cell metabolism for accurate results.
- Apply direct manual pressure for 5-10 minutes since arterial blood flow is high pressure to control bleeding.
- Cover with pressure dressing of gauze squares and tape.
- Assess puncture site periodically for bleeding/hematoma.
- Report lab findings promptly to the provider to improve treatment.
Pulse Oximetry
- It is a noninvasive technique for monitoring blood oxygen saturation.
- The components include a sensor, red and infrared light emitter, and a microprocessor.
- The sensor is attached to finger, toe, earlobe, or nose bridge.
- The sensor detects the hemoglobin light absorption amount.
- Measurement of obtained oxygen saturation is abbreviated as SpO2.
- Infer PaO2 from pulse oximetry (SpO2) measurement.
- The normal SpO2 is 95% to 100%.
- A sustained less than 90% level is cause for concern.
- If SpO2 remains low, oxygen therapy may be needed.
- Factors affect accuracy of displayed information.
Promoting Oxygenation
- Factors impacting ventilation affect oxygenation.
- Positioning and breathing techniques are key interventions.
- Nasal strips reduce airway resistance for better ventilation.
Positioning
- Place hypoxic clients in high Fowler position.
- This position ease diaphragm movement and lung volume.
- Try tripod position in seated position/arms supported to help lift chest.
- Orthopneic position is leaning forward over bedside table or chair.
- Orthopneic allows maximal chest expansion and comfort.
Breathing Techniques
- Include deep breathing, incentive spirometer use, pursed-lip breathing, and diaphragmatic breathing.
Deep Breathing
- Deep breathing maximizes ventilation, filling alveoli.
- Encourage clients to take in as much air for full alveoli, hold breaths briefly, and exhale slowly.
- Use incentive spirometer.
Incentive Spirometry
- Incentive spirometry uses calibrated device to encourage goal-directed inspired air volume.
Factors Affecting Oxygenation
- Adequate respiration relies on a minimum of 21% environmental oxygen and normal cardiopulmonary function.
- Breathing can be voluntarily controlled.
- Chronic lung disease clients are stimulated by low oxygen.
- Smoking causes inhaled carbon monoxide competes for hemoglobin binding.
- Nicotine constricts blood vessels and increases heart rate.
- Smoking while pregnant increases low-birth-weight risks due to fetal oxygen.
- Pulmonary secretions and interstitial fluid interfere with gas exchange.
- Increased gas exchange requires maximum lung expansion.
- Activity/emotional stress increase oxygen needs.
- Abdominal/flank pain reduce deep breaths and forced coughs.
Oxygen Therapy
- When blood isn't saturated enough by positioning and techniques.
- It increases Oxygen to prevent/relieve hypoxemia.
- Requires source, flowmeter, and sometimes analyzer/humidifier.
Nursing Implications for Oxygenation Factors
- Cardiac/pulmonary disorders need more than 21% oxygen.
- Hyperventilating clients need slowed rates and pursed-lip breathing.
- COPD clients can have breathing depressed by high oxygen, avoid 2-3L unless mechanically ventilated.
- Smokers have damaged gas exchange.
- Teach to avoid smoking.
- Encourage fluids, coughing, turning, and ambulating to inflate alveoli.
- Assist clients to sit up and encourage weight loss to lower diaphragm compression.
- Provide rest and teach stress reduction for blood oxygen maintenance.
- Support incision with pillow after lung surgery and use pain relief.
Oxygen Sources
- Sources include wall outlets, portable tanks, liquid oxygen, oxygen concentrators.
- Wall outlets connect to a reservoir filled with oxygen.
- Portable tanks provide oxygen for transport.
- Liquid oxygen units convert cooled liquid oxygen to a gas.
- Oxygen concentrators collect oxygen from room air.
Portable Tanks
- Provide oxygen when wall outlets are not available or clients need transport.
- Hold pressurized volumes and need protective caps.
- "Cracking" the tank involves releasing debris from the outlet using wrench.
Liquid Oxygen Unit
- Coverts it to gas, used at home for better mobility.
- Small units contain 4 to 8 hours of oxygen.
- Some problems include expensive liquid oxygen, leaky unit, and frozen moisture.
Oxygen Concentrator
- Collects oxygen from room air
- Portable concentrators now exist and can be powered by car DC outlet or AC current.
- It Eliminates bulky tanks but needs secondary oxygen during power outages.
Oxygen Administration Equipment
- Flowmeter: regulates liters per minute of oxygen.
- Oxygen Analyzer: confirms the oxygen % delivered.
- Humidifier: adds moisture to oxygen to prevent mucosal drying, used above 4L/minute.
Oxygen Delivery Devices
- Nasal Cannula: Delivers low concentrations of oxygen - ideal for non-hypoxic/chronic lung clients.
- High-Flow Nasal Cannula: Delivers up to 100% oxygen
- Masks -Simple Mask: Used when nasal trauma exists. Delivers no less than 5L/minute. -Partial and Non-rebreather Mask: Delivers higher percentages of oxygen. -Venturi Mask: Delivers exact oxygen via color-coded adapters.
Tracheostomy Collar/T-Piece
- Artificial openings need humidification and oxygenation methods.
Oxygen Therapy Nursing Guidelines
- Post oxygen in use signs; oxygen supports combustion.
- No candles.
- Electrical devices must be grounded, inspect for frayed wires.
- Avoid petroleum/aerosol.
- Secure oxygen to stands.
Oxygen Toxicity
- Lung damage from concentrations of >50% over >48-72 hours, reduces surfactant that enhances elasticit.y
- Early symptoms are subtle; prevent with lowest FIO2 for shortest time.
Related Oxygenation Techniques
- Positive Airway Pressure: Relieves apnea/hypopnea with airway ventilation Continuous Positive Airway Pressure (CPAP): keeps alveoli inflated during expiration
- Bilevel Positive Airway Pressure (BiPAP): varies pressure with breath/promotes tolerance
- Water-Seal Chest Tube: Evacuates air or blood from the chest, restoring intrapleural pressure
- Hyperbaric Oxygen Therapy (HBOT): Delivers 100% oxygen, promotes new tissue.
Nursing Diagnoses
- Altered breathing pattern
- Impaired gas exchange
- Activity intolerance
- Chronic/acute anxiety
- Risk for ineffective airway clearance
Nursing Care Plan
- Assess respiratory rate, effort, chest symmetry, air entry
- Check pulse, BP, level of consciousness, and mental status
- Measure SpO2, assess skin color
- Perform auscultation of lung sounds
- Observe cough and sputum production
- Elevate the head and administer to promote optimal ventilation
- Teach pursed lip and diaphragmatic breathing
- Provide 2L of fluid intake.
Key Points
- Oxygen therapy is required to relieve hypoxemia using nasal cannula, mask or mechanical intubation
- Monitor ABGs or pulse oximetry to determine effectiveness.
- Observe for signs of respiratory distress, reduced energy, rapid, shallow breathing is not effective oxygenation.
- Assess breath sounds due to wheezing, stridor is not indicative of adequate oxygen.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.