Podcast
Questions and Answers
Which of the following best describes the primary function of the cardiopulmonary system?
Which of the following best describes the primary function of the cardiopulmonary system?
- To circulate nutrients throughout the body
- To eliminate waste products from the body
- To supply the oxygen demands of the body (correct)
- To regulate body temperature
What is the relationship between ventilation and perfusion in the context of respiratory function?
What is the relationship between ventilation and perfusion in the context of respiratory function?
- Ventilation is the movement of air, while perfusion is the flow of blood. (correct)
- Ventilation is the movement of air, while perfusion is the elimination of carbon dioxide.
- Ventilation and perfusion are unrelated processes.
- Ventilation is the exchange of gases, while perfusion is the movement of air.
How does the cardiovascular system support oxygenation?
How does the cardiovascular system support oxygenation?
- By providing the transport mechanisms to distribute oxygen to cells and tissues. (correct)
- By directly absorbing oxygen from the air.
- By exchanging gases directly with the environment.
- By regulating the rate and depth of respiration.
Which of the following statements accurately describes gas exchange in the lungs?
Which of the following statements accurately describes gas exchange in the lungs?
What role do neural and chemical regulators play in respiration?
What role do neural and chemical regulators play in respiration?
During respiration, what is the primary exchange that occurs at the cellular level?
During respiration, what is the primary exchange that occurs at the cellular level?
How does intrapleural pressure change to facilitate airflow into the lungs?
How does intrapleural pressure change to facilitate airflow into the lungs?
Which muscles are primarily responsible for creating the negative pleural pressure that increases the size of the thorax during inspiration?
Which muscles are primarily responsible for creating the negative pleural pressure that increases the size of the thorax during inspiration?
What physiological process occurs when the diaphragm relaxes and the internal intercostal muscles contract?
What physiological process occurs when the diaphragm relaxes and the internal intercostal muscles contract?
How does the thickness of the alveolar capillary membrane affect respiratory gas exchange?
How does the thickness of the alveolar capillary membrane affect respiratory gas exchange?
Which of the following conditions can result in a thickened alveolar capillary membrane, thereby affecting gas exchange?
Which of the following conditions can result in a thickened alveolar capillary membrane, thereby affecting gas exchange?
What is the primary function of the oxygen-transport system in the body?
What is the primary function of the oxygen-transport system in the body?
What is a key factor that influences the amount of oxygen delivered to the lungs?
What is a key factor that influences the amount of oxygen delivered to the lungs?
How is carbon dioxide transported from the tissues back to the lungs for exhalation?
How is carbon dioxide transported from the tissues back to the lungs for exhalation?
What role does the central nervous system play in the regulation of respiration?
What role does the central nervous system play in the regulation of respiration?
How does the cerebral cortex influence respiration?
How does the cerebral cortex influence respiration?
What changes in blood composition stimulate chemoreceptors to adjust respiratory regulation?
What changes in blood composition stimulate chemoreceptors to adjust respiratory regulation?
Which process is directly facilitated by the right ventricle of the heart?
Which process is directly facilitated by the right ventricle of the heart?
What is the function of the left ventricle in the context of oxygenation?
What is the function of the left ventricle in the context of oxygenation?
What is the primary function of the coronary arteries?
What is the primary function of the coronary arteries?
What is the primary determinant of cardiac output?
What is the primary determinant of cardiac output?
How is cardiac output calculated?
How is cardiac output calculated?
Which of the following best describes the role of the sinoatrial (SA) node in the cardiac conduction system?
Which of the following best describes the role of the sinoatrial (SA) node in the cardiac conduction system?
What is the correct sequence of the cardiac impulse pathway?
What is the correct sequence of the cardiac impulse pathway?
An electrocardiogram (ECG) is used to assess which aspect of cardiac function?
An electrocardiogram (ECG) is used to assess which aspect of cardiac function?
Which of the following conditions directly decreases the oxygen-carrying capacity of the blood?
Which of the following conditions directly decreases the oxygen-carrying capacity of the blood?
How does pregnancy affect oxygenation?
How does pregnancy affect oxygenation?
Which of the following is a common adaptation in patients with chronic lung disease that affects the chest wall?
Which of the following is a common adaptation in patients with chronic lung disease that affects the chest wall?
Which condition is characterized by ventilation in excess of what is required to eliminate carbon dioxide produced by cellular metabolism?
Which condition is characterized by ventilation in excess of what is required to eliminate carbon dioxide produced by cellular metabolism?
What is a potential cause of hypoventilation?
What is a potential cause of hypoventilation?
Inadequate tissue oxygenation at the cellular level is defined as which condition?
Inadequate tissue oxygenation at the cellular level is defined as which condition?
What is a late sign of hypoxia?
What is a late sign of hypoxia?
Which condition involves electrical impulses in the heart that do not originate from the SA node?
Which condition involves electrical impulses in the heart that do not originate from the SA node?
What is the primary feature of altered cardiac output related to oxygenation?
What is the primary feature of altered cardiac output related to oxygenation?
What is the purpose of pursed-lip breathing exercises?
What is the purpose of pursed-lip breathing exercises?
What is a key focus of health promotion related to oxygenation?
What is a key focus of health promotion related to oxygenation?
What is recognized as a key goal of oxygen therapy?
What is recognized as a key goal of oxygen therapy?
What physiological principle explains how air moves into and out of the lungs during breathing?
What physiological principle explains how air moves into and out of the lungs during breathing?
Which of the following accurately describes the role of the diaphragm and intercostal muscles in respiration?
Which of the following accurately describes the role of the diaphragm and intercostal muscles in respiration?
How does an increased thickness of the alveolar capillary membrane affect the process of respiratory gas exchange?
How does an increased thickness of the alveolar capillary membrane affect the process of respiratory gas exchange?
What is the primary mechanism by which oxygen-carrying capacity is determined in the blood?
What is the primary mechanism by which oxygen-carrying capacity is determined in the blood?
How do chemoreceptors in the body contribute to the regulation of respiration?
How do chemoreceptors in the body contribute to the regulation of respiration?
What would be the immediate physiological consequence of the right ventricle's failure to pump efficiently?
What would be the immediate physiological consequence of the right ventricle's failure to pump efficiently?
How do the coronary arteries support the heart's ability to function as an effective pump?
How do the coronary arteries support the heart's ability to function as an effective pump?
How does an increase in a patient's metabolic rate affect their oxygen demand and CO2 production?
How does an increase in a patient's metabolic rate affect their oxygen demand and CO2 production?
Which assessment finding would indicate that a patient is experiencing hypoventilation
Which assessment finding would indicate that a patient is experiencing hypoventilation
Why is it critical to recognize cyanosis as a clinical sign?
Why is it critical to recognize cyanosis as a clinical sign?
Flashcards
Cardio and respiratory systems
Cardio and respiratory systems
Supplies the oxygen demands of the body.
Cardiovascular system
Cardiovascular system
Provides the transport mechanisms to distribute oxygen to cells and tissues.
Respiration
Respiration
The exchange of oxygen and carbon dioxide during cellular metabolism.
Intrapleural pressure
Intrapleural pressure
Signup and view all the flashcards
Ventilation
Ventilation
Signup and view all the flashcards
Diffusion
Diffusion
Signup and view all the flashcards
Perfusion
Perfusion
Signup and view all the flashcards
Atelectasis
Atelectasis
Signup and view all the flashcards
Alveolar capillary membrane
Alveolar capillary membrane
Signup and view all the flashcards
Cardiac Output
Cardiac Output
Signup and view all the flashcards
Heart Rate
Heart Rate
Signup and view all the flashcards
Stroke Volume
Stroke Volume
Signup and view all the flashcards
electrical impulses
electrical impulses
Signup and view all the flashcards
Altered cardiac output
Altered cardiac output
Signup and view all the flashcards
Myocardial ischemia
Myocardial ischemia
Signup and view all the flashcards
Infants & Toddlers
Infants & Toddlers
Signup and view all the flashcards
School-aged children & adolescents
School-aged children & adolescents
Signup and view all the flashcards
Young & middle aged adults
Young & middle aged adults
Signup and view all the flashcards
Older adults
Older adults
Signup and view all the flashcards
Dyspnea
Dyspnea
Signup and view all the flashcards
Cough
Cough
Signup and view all the flashcards
Wheezing
Wheezing
Signup and view all the flashcards
Fatigue
Fatigue
Signup and view all the flashcards
Chest pain
Chest pain
Signup and view all the flashcards
Goal in oxygen theory?
Goal in oxygen theory?
Signup and view all the flashcards
Venturi mask
Venturi mask
Signup and view all the flashcards
Defibrillation
Defibrillation
Signup and view all the flashcards
what is the gas we breathe in and breathe out?
what is the gas we breathe in and breathe out?
Signup and view all the flashcards
Signup and view all the flashcards
Study Notes
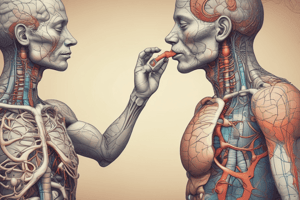
- Oxygen is essential for sustaining life
- The cardiac and respiratory systems work together to meet the body's oxygen needs
- The cardiovascular system transports oxygen to cells and tissues
- Respiratory gases are exchanged between the environment and the blood
- Neural and chemical regulators control respiratory rate and depth based on tissue oxygen demands
Respiration
- Respiration involves exchanging oxygen and carbon dioxide during cellular metabolism
Respiratory Physiology
- Gas exchange occurs in the lungs due to pressure changes
- Intrapleural pressure is negative compared to atmospheric pressure
- Intrapleural pressure becoming more negative creates a pressure gradient for air flow into the lungs
- The diaphragm and external intercostal muscles contract, which increases the size of the thorax
Steps in Oxygenation
- Ventilation is the process of moving gases into and out of the lungs.
- Diffusion involves exchanging respiratory gases across the alveoli capillary membrane
- Perfusion is when the cardiovascular system pumps blood to and from the lungs and body
Respiratory Terminology
- Involves concepts like airway resistance, compliance, work of breathing, inspiration, expiration, atelectasis, and surfactant
- Decreased lung compliance leads to increased airway resistance
- Increased airway resistance causes increased use of accessory muscles
- Increased use of accessory muscles leads to increased breathing work
- Increased breathing work results in increased energy expenditure
Respiratory Physiology
- Normal lung values are determined by age, gender, and height
- Involves tidal volume, residual volume, and forced vital capacity
- Spirometry is used to measure lung volumes
Respiratory Gas Exchange
- Diffusion of respiratory gases occurs at the alveolar capillary membrane
- The thickness of the membrane affects diffusion rate
- Increased membrane thickness slows diffusion, reduces gas exchange, and decreases oxygen delivery to tissues
- Pulmonary edema, pulmonary infiltrates, or pulmonary effusion thickens the membrane
- Chronic diseases, acute diseases, and surgical processes can alter the alveolar capillary membrane surface area
Oxygen Transport
- The oxygen-transport system consists of the lungs and cardiovascular system
- Delivery depends on ventilation, perfusion, rate of diffusion, and oxygen-carrying capacity
- Carbon dioxide is transported back to the lungs for exhalation.
Regulation of Respiration
- The central nervous system controls respiratory rate, depth, and rhythm
- The cerebral cortex regulates voluntary control of respiration
- It maintains the rate and depth of respiratory based on changes CO2 and hydrogen ion concentration
- Chemoreceptors sense changes in chemical content and adjust neural regulators
Cardiovascular Physiology
- The right ventricle pumps deoxygenated blood through the lungs
- The left ventricle pumps oxygenated blood through the systemic circulation
- Consists of two atria and two ventricles
Blood Flow Regulation
- Cardiac output is the amount of blood ejected from the left ventricle each minute
- Stroke volume is the amount of blood ejected from the ventricle with each contraction
- Afterload is the resistance to left ventricle ejection
- Preload is the amount of blood in the left ventricle at the end of diastole
Conduction System
- Includes the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, and Purkinje fibers
- Generates and transmits electrical impulses
- Sinoatrial (SA) node acts as the pacemaker
- Atrioventricular (AV) node acts as the mediator
Electrocardiogram
- Reflects the electrical conduction system of the heart
Factors Affecting Oxygenation
- Decreased oxygen-carrying capacity can be attributed to anemia or Carbon Monoxide
- Hypovolemia can be attributed to shock or severe dehydration
- Decreased inspired oxygen concentration includes airway obstruction and decreased environmental oxygen
- Increase in metabolic rate is due to pregnancy, exercise, wound healing or a fever
- Conditions such as pregnancy, obesity, or neuromuscular diseases affect chest wall movement
- Chronic lung disease and changes in the anteroposterior diameter of the chest wall occur because of overuse of accessory muscles & air trapping
Alterations in Respiratory Functioning
- Hyperventilation occurs when ventilation exceeds the requirement to eliminate carbon dioxide produced by the cells
- Can be caused by anxiety, infection, drugs, acid-base imbalance, fever, and aspirin poisoning
- Hypoventilation occurs when alveolar ventilation is inadequate to meet the body's oxygen demand
- Can be caused by atelectasis and collapsed alveoli
- Hypoxia is inadequate tissue oxygenation at the cellular level
- Can be caused by anemia, carbon monoxide poisoning, pneumonia, and spinal cord injury
- Cyanosis is a blue discoloration of the skin and mucous membranes
- Can be caused by desaturated hemoglobin in capillaries and is a late sign of hypoxia
Alterations in Cardiac Functioning
- Disturbances in conduction (dysrhythmias) are caused by electrical impulses that do not originate from the Sinoatrial (SA) node
- Altered cardiac output occurs when insufficient volume is ejected into systemic and pulmonary circulation
- Impaired valvular function includes stenosis and regurgitation
- Myocardial Ischemia occurs when blood to the myocardium does not meet myocardial oxygen needs
- Includes conditions such as angina and Myocardial Infarction
Developmental Factors
- Infants and Toddlers - Risk for upper respiratory infections and nasal congestion
- School-aged children and adolescents - Risk for respiratory infections & secondhand smoke
- Young & middle-aged adults - Smokng, unhealthy diet and stress
- Older adults - Calcification of valves, SA node & costal cartilage. Osteoporosis
Risk Factors
- Includes smoking, substance abuse, and stress
Environmental Factors
- Includes air pollution from air particles
Aspiration
- Should ensure proper posture when eating
- Evaluate by determining if patients can swallow
- Feed through feeding tubes
Nursing History
- It is also important to know what the patients symptoms are (I.e. Wheezing)
- Also imporatnt to determine health risks (allergies, and medications)
Implementations
- Flu shots prevent pnemonia and influenza
- It is vital to eliminate hazardous environmets that can hinder on breathing
Implementations: Acute Care
- Care includes, dyspnea, humidification, airway maintenence, and chest physio treament
Suctioning
- Used when patients are unable to clear respiratory secretions from the airways by coughing
Artificial airways
- Include Endotracheal Tubes
Maintenence and Promotion of Lung Expansion
- It is important to promote ambulation and positioning and incentive spirometry
Breathing treatment
- It is important to treat hypoxia, it can be due to a combustible from a flame
- Supply of oxygen is due to tanks or wall-piped systems
Oxygen Devices
- Comes in the form of
- Nasal Cannula
- Venturi Mask
- Non rebreather mask
- Ambu bam and face mask
- Aerosol mask
CPR
- Pumping 30 breaths at a time
Restorative Care
- Nutrition is important as well as breathing treatment
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.