Podcast
Questions and Answers
What is the primary function of acinar cells in the pancreas?
What is the primary function of acinar cells in the pancreas?
- Regulating blood sugar
- Producing digestive enzymes (correct)
- Secreting bicarbonate-rich fluid
- Transporting digestive enzymes
Gallstones are the leading cause of acute pancreatitis.
Gallstones are the leading cause of acute pancreatitis.
True (A)
Define acute pancreatitis.
Define acute pancreatitis.
Acute pancreatitis is the inflammation of the pancreas.
The pancreas functions as both an endocrine and _____ gland.
The pancreas functions as both an endocrine and _____ gland.
What role does bicarbonate-rich fluid play in pancreatic secretions?
What role does bicarbonate-rich fluid play in pancreatic secretions?
Proteases are kept in an inactive form to prevent damage to the pancreas.
Proteases are kept in an inactive form to prevent damage to the pancreas.
Name one key cause of acute pancreatitis.
Name one key cause of acute pancreatitis.
The activation of digestive enzymes within the pancreas can lead to _____ of pancreatic tissue.
The activation of digestive enzymes within the pancreas can lead to _____ of pancreatic tissue.
Match the digestive enzyme to its function:
Match the digestive enzyme to its function:
What factors contribute to the development of acute pancreatitis?
What factors contribute to the development of acute pancreatitis?
Which of the following can cause acute pancreatitis? (Select all that apply)
Which of the following can cause acute pancreatitis? (Select all that apply)
Hypercalcemia can inadvertently activate pancreatic enzymes.
Hypercalcemia can inadvertently activate pancreatic enzymes.
What is the hallmark symptom of acute pancreatitis?
What is the hallmark symptom of acute pancreatitis?
The process of autodigestion in acute pancreatitis is primarily caused by the activation of ______ enzymes.
The process of autodigestion in acute pancreatitis is primarily caused by the activation of ______ enzymes.
Match the symptoms of acute pancreatitis with their descriptions:
Match the symptoms of acute pancreatitis with their descriptions:
What is the primary complication that can arise from acute pancreatitis?
What is the primary complication that can arise from acute pancreatitis?
Cullen's sign indicates fluid accumulation in the abdomen.
Cullen's sign indicates fluid accumulation in the abdomen.
Name one drug associated with causing acute pancreatitis.
Name one drug associated with causing acute pancreatitis.
Acute pancreatitis can lead to the formation of ______, which may become infected.
Acute pancreatitis can lead to the formation of ______, which may become infected.
Which inflammatory mediators are released during the body response to inflammation in acute pancreatitis?
Which inflammatory mediators are released during the body response to inflammation in acute pancreatitis?
What is a classic symptom of pancreatitis?
What is a classic symptom of pancreatitis?
Elevated amylase levels are more specific than elevated lipase levels for diagnosing pancreatitis.
Elevated amylase levels are more specific than elevated lipase levels for diagnosing pancreatitis.
Name two risk factors for pancreatitis.
Name two risk factors for pancreatitis.
Elevated lipase levels need to be greater than _____ times the upper limit of normal to confirm a diagnosis of pancreatitis.
Elevated lipase levels need to be greater than _____ times the upper limit of normal to confirm a diagnosis of pancreatitis.
Match the laboratory findings with their implications for pancreatitis:
Match the laboratory findings with their implications for pancreatitis:
What imaging studies are used to assess the severity of pancreatitis?
What imaging studies are used to assess the severity of pancreatitis?
Patients with pancreatitis should be monitored for both symptoms and laboratory changes.
Patients with pancreatitis should be monitored for both symptoms and laboratory changes.
What laboratory finding may indicate a hemoconcentration in a patient with pancreatitis?
What laboratory finding may indicate a hemoconcentration in a patient with pancreatitis?
Signs of _____ may appear as low hemoglobin alongside elevated hematocrit in pancreatitis.
Signs of _____ may appear as low hemoglobin alongside elevated hematocrit in pancreatitis.
Which of the following is NOT a classic symptom of pancreatitis?
Which of the following is NOT a classic symptom of pancreatitis?
Which enzyme is primarily responsible for breaking down lipids?
Which enzyme is primarily responsible for breaking down lipids?
Acute pancreatitis can occur due to an obstruction of pancreatic ducts.
Acute pancreatitis can occur due to an obstruction of pancreatic ducts.
What is a common symptom of acute pancreatitis?
What is a common symptom of acute pancreatitis?
The pancreas can be classified as an endocrine and ______ gland.
The pancreas can be classified as an endocrine and ______ gland.
Match the following causes of acute pancreatitis with their descriptions:
Match the following causes of acute pancreatitis with their descriptions:
Which of the following statements about zymogens is true?
Which of the following statements about zymogens is true?
Alcohol abuse primarily leads to an increase in the production of bicarbonate-rich fluid in pancreatitis.
Alcohol abuse primarily leads to an increase in the production of bicarbonate-rich fluid in pancreatitis.
Name one mechanism that leads to autodigestion of pancreatic tissue.
Name one mechanism that leads to autodigestion of pancreatic tissue.
Zymogens are stored in ______ cells to prevent self-digestion of the pancreas.
Zymogens are stored in ______ cells to prevent self-digestion of the pancreas.
Elevated triglycerides in hypertriglyceridemia can lead to which issue in the pancreas?
Elevated triglycerides in hypertriglyceridemia can lead to which issue in the pancreas?
Which of the following is a systemic effect of extensive inflammation due to pancreatitis?
Which of the following is a systemic effect of extensive inflammation due to pancreatitis?
Elevated CRP levels indicate localized inflammation within the pancreas.
Elevated CRP levels indicate localized inflammation within the pancreas.
What is the hallmark symptom of acute pancreatitis?
What is the hallmark symptom of acute pancreatitis?
The acronym 'I GET SMASHED' is used to remember the causes of acute pancreatitis. One of the causes represented by 'M' is ______.
The acronym 'I GET SMASHED' is used to remember the causes of acute pancreatitis. One of the causes represented by 'M' is ______.
Match the following complications of acute pancreatitis with their descriptions:
Match the following complications of acute pancreatitis with their descriptions:
Which of the following medications is associated with causing acute pancreatitis?
Which of the following medications is associated with causing acute pancreatitis?
Cullen's sign and Grey Turner's sign are indicators of gastrointestinal bleeding in pancreatitis.
Cullen's sign and Grey Turner's sign are indicators of gastrointestinal bleeding in pancreatitis.
Name one rare cause of acute pancreatitis.
Name one rare cause of acute pancreatitis.
In acute pancreatitis, inflammation can lead to the formation of ______, which can become infected.
In acute pancreatitis, inflammation can lead to the formation of ______, which can become infected.
Match the following inflammatory mediators with their effects:
Match the following inflammatory mediators with their effects:
What is a common symptom of pancreatitis?
What is a common symptom of pancreatitis?
Gallstones are one of the risk factors for developing pancreatitis.
Gallstones are one of the risk factors for developing pancreatitis.
What laboratory level is primarily used to confirm a diagnosis of pancreatitis?
What laboratory level is primarily used to confirm a diagnosis of pancreatitis?
Elevated lipase levels need to be greater than _____ times the upper limit of normal to confirm a diagnosis of pancreatitis.
Elevated lipase levels need to be greater than _____ times the upper limit of normal to confirm a diagnosis of pancreatitis.
Match the following diagnostic indicators with their implications for pancreatitis:
Match the following diagnostic indicators with their implications for pancreatitis:
Which imaging studies are important in assessing pancreatitis?
Which imaging studies are important in assessing pancreatitis?
Nausea and vomiting are not associated with pancreatitis.
Nausea and vomiting are not associated with pancreatitis.
What condition may cause elevated hematocrit in a patient with pancreatitis?
What condition may cause elevated hematocrit in a patient with pancreatitis?
Pancreatitis can lead to complications that may require _____ interventions.
Pancreatitis can lead to complications that may require _____ interventions.
Which of the following statements about lipase and amylase is true?
Which of the following statements about lipase and amylase is true?
Which of the following is NOT a cause of acute pancreatitis?
Which of the following is NOT a cause of acute pancreatitis?
Ethanol alters the viscosity of pancreatic secretions, potentially leading to obstruction.
Ethanol alters the viscosity of pancreatic secretions, potentially leading to obstruction.
What do acinar cells primarily produce?
What do acinar cells primarily produce?
In acute pancreatitis, the pancreas undergoes ______ due to the activation of digestive enzymes.
In acute pancreatitis, the pancreas undergoes ______ due to the activation of digestive enzymes.
Which of the following enzymes is responsible for breaking down carbohydrates?
Which of the following enzymes is responsible for breaking down carbohydrates?
Match the following enzymes with their respective functions:
Match the following enzymes with their respective functions:
Gallstones are considered the leading cause of acute pancreatitis.
Gallstones are considered the leading cause of acute pancreatitis.
Name one mechanism that can lead to the autodigestion of pancreatic tissue.
Name one mechanism that can lead to the autodigestion of pancreatic tissue.
Zymogens are stored in ______ cells to protect the pancreas from self-digestion.
Zymogens are stored in ______ cells to protect the pancreas from self-digestion.
Which of the following complications can arise from acute pancreatitis?
Which of the following complications can arise from acute pancreatitis?
Which of the following classic symptoms is associated with pancreatitis?
Which of the following classic symptoms is associated with pancreatitis?
Elevated amylase levels are more specific than elevated lipase levels for diagnosing pancreatitis.
Elevated amylase levels are more specific than elevated lipase levels for diagnosing pancreatitis.
What laboratory level must be elevated to confirm a diagnosis of pancreatitis?
What laboratory level must be elevated to confirm a diagnosis of pancreatitis?
Patients with pancreatitis may show signs of ______ bleeding which can be indicated by low hemoglobin.
Patients with pancreatitis may show signs of ______ bleeding which can be indicated by low hemoglobin.
Match the following risk factors with their descriptions:
Match the following risk factors with their descriptions:
Which imaging studies assist in assessing the severity of pancreatitis?
Which imaging studies assist in assessing the severity of pancreatitis?
Monitoring for symptoms and laboratory changes is crucial for managing pancreatitis.
Monitoring for symptoms and laboratory changes is crucial for managing pancreatitis.
Name one imaging study used in the assessment of pancreatitis severity.
Name one imaging study used in the assessment of pancreatitis severity.
The hematocrit levels in a complete blood count (CBC) may show ______ due to plasma leakage.
The hematocrit levels in a complete blood count (CBC) may show ______ due to plasma leakage.
What is one common risk factor for pancreatitis?
What is one common risk factor for pancreatitis?
What is a common symptom of acute pancreatitis that radiates to the back?
What is a common symptom of acute pancreatitis that radiates to the back?
The mumps virus has no effect on pancreatic cells.
The mumps virus has no effect on pancreatic cells.
Name a drug class that is known to cause acute pancreatitis.
Name a drug class that is known to cause acute pancreatitis.
The acronym 'I GET SMASHED' helps to remember the causes of acute pancreatitis, where 'E' stands for ______.
The acronym 'I GET SMASHED' helps to remember the causes of acute pancreatitis, where 'E' stands for ______.
Match the following causes of acute pancreatitis with their descriptions:
Match the following causes of acute pancreatitis with their descriptions:
Which inflammatory mediator may lead to systemic effects such as fever during acute pancreatitis?
Which inflammatory mediator may lead to systemic effects such as fever during acute pancreatitis?
Hypertriglyceridemia is not a recognized cause of acute pancreatitis.
Hypertriglyceridemia is not a recognized cause of acute pancreatitis.
What is the typical presentation of Cullen’s sign?
What is the typical presentation of Cullen’s sign?
The process of ______ describes the breakdown of pancreatic tissue when enzymes are prematurely activated.
The process of ______ describes the breakdown of pancreatic tissue when enzymes are prematurely activated.
Match the following complications of acute pancreatitis with their effects:
Match the following complications of acute pancreatitis with their effects:
What is the primary function of the bicarbonate-rich fluid secreted by ductal cells in the pancreas?
What is the primary function of the bicarbonate-rich fluid secreted by ductal cells in the pancreas?
Ethanol leads to autodigestion of the pancreas by directly activating zymogens.
Ethanol leads to autodigestion of the pancreas by directly activating zymogens.
Which type of enzymes are produced by acinar cells in the pancreas?
Which type of enzymes are produced by acinar cells in the pancreas?
Gallstones can obstruct the flow of digestive juices, most commonly leading to ______ pancreatitis.
Gallstones can obstruct the flow of digestive juices, most commonly leading to ______ pancreatitis.
Match the pancreatic enzyme to its function:
Match the pancreatic enzyme to its function:
What condition may result from elevated triglycerides in the context of acute pancreatitis?
What condition may result from elevated triglycerides in the context of acute pancreatitis?
Trauma can cause acute pancreatitis by directly releasing zymogens from acinar cells.
Trauma can cause acute pancreatitis by directly releasing zymogens from acinar cells.
Name one primary mechanism by which acute pancreatitis develops.
Name one primary mechanism by which acute pancreatitis develops.
Acinar cells store digestive enzymes in an inactive form known as ______.
Acinar cells store digestive enzymes in an inactive form known as ______.
Which of the following is a common clinical symptom of acute pancreatitis?
Which of the following is a common clinical symptom of acute pancreatitis?
Which of the following is a rare cause of acute pancreatitis?
Which of the following is a rare cause of acute pancreatitis?
Elevated calcium levels can lead to the activation of pancreatic enzymes.
Elevated calcium levels can lead to the activation of pancreatic enzymes.
What is the hallmark symptom of acute pancreatitis?
What is the hallmark symptom of acute pancreatitis?
The acronym 'I GET SMASHED' helps remember the causes of acute pancreatitis, where 'E' stands for _____.
The acronym 'I GET SMASHED' helps remember the causes of acute pancreatitis, where 'E' stands for _____.
Match the following systemic effects of acute pancreatitis with their descriptions:
Match the following systemic effects of acute pancreatitis with their descriptions:
Which medication is commonly associated with causing acute pancreatitis?
Which medication is commonly associated with causing acute pancreatitis?
In acute pancreatitis, inflammation can lead to the formation of _____, which can become infected.
In acute pancreatitis, inflammation can lead to the formation of _____, which can become infected.
Cullen's sign indicates elevated levels of bilirubin in the bloodstream.
Cullen's sign indicates elevated levels of bilirubin in the bloodstream.
Name one cytokine that plays a role in the inflammatory response during acute pancreatitis.
Name one cytokine that plays a role in the inflammatory response during acute pancreatitis.
Which of the following symptoms may occur if a gallstone obstructs the bile duct during pancreatitis?
Which of the following symptoms may occur if a gallstone obstructs the bile duct during pancreatitis?
Which of the following are classic symptoms of pancreatitis? (Select all that apply)
Which of the following are classic symptoms of pancreatitis? (Select all that apply)
Elevated lipase levels are less important than elevated amylase levels in diagnosing pancreatitis.
Elevated lipase levels are less important than elevated amylase levels in diagnosing pancreatitis.
What imaging studies are commonly used to assess the severity of pancreatitis?
What imaging studies are commonly used to assess the severity of pancreatitis?
In acute pancreatitis, common risk factors include _____, alcohol use, and hypertriglyceridemia.
In acute pancreatitis, common risk factors include _____, alcohol use, and hypertriglyceridemia.
Match the following laboratory findings with their implications for pancreatitis:
Match the following laboratory findings with their implications for pancreatitis:
What is required for confirming a diagnosis of pancreatitis?
What is required for confirming a diagnosis of pancreatitis?
Monitoring changes in laboratory results is not necessary for managing pancreatitis patients.
Monitoring changes in laboratory results is not necessary for managing pancreatitis patients.
Name one common complication of acute pancreatitis.
Name one common complication of acute pancreatitis.
Signs of retroperitoneal bleeding in pancreatitis may be indicated by low hemoglobin alongside elevated _____ levels.
Signs of retroperitoneal bleeding in pancreatitis may be indicated by low hemoglobin alongside elevated _____ levels.
Which of the following is a primary risk factor for developing pancreatitis?
Which of the following is a primary risk factor for developing pancreatitis?
Study Notes
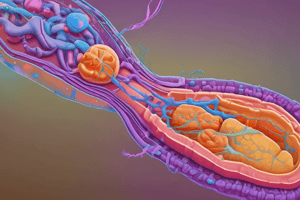
Overview of Acute Pancreatitis
- Acute pancreatitis is the inflammation of the pancreas.
- The pancreas is a heterochronic gland functioning as both an endocrine and exocrine gland, focusing mainly on its exocrine role in digestion.
Pancreatic Structure and Function
- The ductal system consists of main and accessory pancreatic ducts that transport digestive enzymes to the duodenum.
- Two major components of pancreatic secretions include digestive enzymes and a bicarbonate-rich fluid.
- Acinar cells produce digestive enzymes, while ductal cells secrete bicarbonate-rich fluid.
Enzyme Production
- Enzymes produced by acinar cells are stored as zymogens (inactive form) to prevent auto-digestion of the pancreas.
- Types of digestive enzymes:
- Lipases: Break down lipids.
- Amylases: Break down carbohydrates.
- Proteases: Break down proteins, kept inactive by protease inhibitors within granules.
Mechanism of Pancreatitis Development
- Pancreatitis develops when digestive enzyme secretion is altered, leading to autodigestion of pancreatic tissue.
- Two primary mechanisms:
- Obstruction of pancreatic ducts: Increases pressure, causing lysosomes to fuse with granules, activating proteases prematurely.
- Direct damage to acinar cells: Can release zymogens that activate inappropriately, causing tissue destruction.
Key Causes of Acute Pancreatitis
- Gallstones: Most common cause, obstructs the flow of digestive juices leading to activation of proteases.
- Ethanol (Alcohol Abuse): Stimulates acinar cells and increases viscosity of secretions, leading to obstructions and autodigestion.
- Activates neutrophils that produce reactive oxygen species, destroying acinar cells.
- Trauma: Penetrating injuries directly damage acinar cells, leading to the release of zymogens.
- Hypertriglyceridemia: Elevated triglycerides can clog pancreatic capillaries, reducing oxygen supply and causing ischemic damage.
- Corticosteroids: Cause thick secretions from ductal cells, increasing the chance of duct obstruction.
- Mumps Virus: Directly affects both ductal and acinar cells, leading to cell destruction and enzyme activation.
- Autoimmune Conditions: Antibodies can damage ductal and acinar cells, facilitating activation of zymogens.
- Scorpion Stings: Rarely, toxins can destroy epithelial cells, leading to similar harmful effects as described above.
Summary
-
Acute pancreatitis is a serious inflammatory condition characterized by autodigestion of the pancreas due to various obstructions or cellular damage.
-
Understanding the anatomy and functions of pancreatic structures is critical for comprehending the pathophysiology of this condition.### Causes of Acute Pancreatitis
-
Drugs: Certain medications can lead to pancreatitis. Key drugs include:
- Sulfa Drugs: Examples like Bactrim and sulfasalazine.
- HIV Medications: Particularly NRTIs and protease inhibitors.
- Diabetic Medications: GLP-1 receptor agonists.
-
Endoscopic Retrograde Cholangiopancreatography (ERCP): A procedure used to diagnose and remove gallstones, which can lead to pancreatic tissue damage if complications arise during the process.
-
Hypercalcemia: Elevated calcium levels can stimulate pancreatic enzymes, leading to inadvertent activation and damage to pancreatic tissue.
Pathophysiology of Acute Pancreatitis
- Inflammation Process: Damage to the pancreas triggers an inflammatory response, which exacerbates tissue destruction and enzymatic activation.
- Digestive Enzyme Activation: Normally inactive enzymes in the pancreas should only activate in the duodenum, but certain conditions can lead to premature activation within the pancreas itself.
Symptoms of Acute Pancreatitis
-
Epigastric Abdominal Pain: The hallmark symptom, characterized by:
- Constant pain that radiates to the back.
- Worsens when lying supine and improves when leaning forward.
-
Nausea and Vomiting: Resulting from inflammation and potential obstruction of the digestive tract.
-
Jaundice: May occur if a gallstone obstructs the bile duct, leading to an accumulation of bilirubin in the bloodstream.
Complications of Acute Pancreatitis
-
Systemic Effects: Extensive inflammation can cause systemic complications, including:
- Hypotension: Due to vasodilation and fluid loss.
- Tachycardia: Reflex response to low blood pressure.
-
Disseminated Intravascular Coagulation (DIC): Characterized by widespread clotting within blood vessels leading to bleeding due to consumption of clotting factors.
-
Effects on Nearby Structures: Inflammation can compress adjacent structures like the duodenum, potentially causing:
- Abdominal Distension: Due to food blockage.
- Decreased Bowel Sounds: Reflecting reduced gastrointestinal motility.
Mnemonic for Causes of Acute Pancreatitis
- "I GET SMASHED":
- I: Idiopathic
- G: Gallstones (most common cause)
- E: Ethanol (alcohol)
- T: Trauma
- S: Steroids
- M: Mumps virus
- A: Autoimmune conditions (e.g., SLE, rheumatoid arthritis)
- S: Scorpion bites (rare)
- H: Hypertriglyceridemia and hypercalcemia
- D: Drugs (sulfa, HIV medications) and ERCP.
Body Response to Inflammation
-
Vasodilation and Permeability Changes: Inflammatory mediators lead to:
- Widening blood vessels, causing lower systemic vascular resistance and blood pressure.
- Increased vessel permeability causing fluid leakage into tissues, resulting in edema.
-
Sympathetic Nervous System Activation: Reduced blood volume and pressure stimulate sympathetic responses, leading to increased heart rate.
-
Cytokine Release: Inflammatory mediators like IL-1, IL-6, and TNF-alpha can have systemic effects, including inducing fever and further affecting coagulation.### Complications of Pancreatitis
-
Body temperature increase can inhibit bacteria survival, leading to hypothalamus stimulation and fever.
-
Common clinical manifestations include hypotension and tachycardia.
-
Increased cytokine levels cause leukocytosis due to enhanced white blood cell production from bone marrow.
-
Liver responds to inflammation by producing acute phase reactant proteins; key proteins include C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
-
Elevated CRP and ESR indicate generalized inflammation.
-
Cytokines can lead to systemic vasodilation and increased capillary permeability, resulting in pulmonary edema, a serious complication from pancreatitis.
-
Severe pulmonary edema may lead to acute respiratory distress syndrome (ARDS), the leading cause of pancreatitis-related mortality.
-
In extreme cases, pancreatic necrosis can lead to fistula formation through the diaphragm, potentially causing pleural effusion.
Abdominal Complications
- Fluid accumulation in the abdomen from increased permeability results in ascites, leading to abdominal distension.
- Reduced effective arterial blood volume from hypotension can impair kidney perfusion, potentially causing pre-renal acute kidney injury (AKI).
Inflammatory Responses and Necrosis
- Damage to pancreas releases enzymes (proteases and lipases) that can cause liquefactive necrosis, breaking down peripancreatic fat.
- Free fatty acids released from fat breakdown can bind calcium, causing hypocalcemia through a saponification reaction.
- Inflammation can lead to fluid collections, forming encapsulated collections known as pancreatic pseudocysts.
- Pseudocysts can become infected, leading to pancreatic abscesses, characterized by fever, severe pain, and leukocytosis.
Vascular Complications
- Proteases from inflammation can damage blood vessels, possibly leading to hemorrhagic necrosis and significant bleeding.
- Retroperitoneal hemorrhage may present as Cullen's sign (bruising around the belly button) or Grey Turner’s sign (flank bruising), indicating serious vascular complications.
Diagnosis of Pancreatitis
- Classic symptoms include epigastric pain radiating to the back, worsening in supine position, along with nausea and vomiting.
- Risk factors include gallstones, alcohol use, and hypertriglyceridemia.
- Diagnosis confirmed through elevated lipase levels (> three times the upper limit of normal); amylase levels can also be elevated but are less specific.
- Imaging studies assist in assessing severity and identifying complications.
- Complete blood count (CBC) may show hemoconcentration due to plasma leakage, reflected as an elevated hematocrit.
- Signs of retroperitoneal bleeding may appear as low hemoglobin alongside elevated hematocrit.
Key Takeaways
- Monitoring for symptoms and laboratory changes is crucial in managing patients with pancreatitis.
- Awareness of potential complications can guide proper intervention and treatment strategies.
- Laboratory diagnostics, primarily lipase levels and imaging, play a critical role in confirming diagnosis and assessing severity.
Overview of Acute Pancreatitis
- Acute pancreatitis is an inflammatory condition affecting the pancreas, mainly its exocrine function.
- The pancreas functions as both an endocrine and exocrine gland but predominantly focuses on digestion through enzyme secretion.
Pancreatic Structure and Function
- The ductal system includes main and accessory pancreatic ducts that deliver digestive enzymes to the duodenum.
- Key components of pancreatic secretions:
- Digestive enzymes produced by acinar cells.
- Bicarbonate-rich fluid secreted by ductal cells.
Enzyme Production
- Digestive enzymes are stored as zymogens to avoid the autodigestion of pancreatic tissue.
- Types of digestive enzymes include:
- Lipases for lipid breakdown.
- Amylases for carbohydrate breakdown.
- Proteases for protein breakdown, controlled by protease inhibitors.
Mechanism of Pancreatitis Development
- Development occurs when enzyme secretion is altered, leading to autodigestion of pancreatic tissue.
- Mechanisms include:
- Obstruction of pancreatic ducts, causing pressure buildup and premature enzyme activation.
- Direct damage to acinar cells, allowing inappropriate zymogen activation.
Key Causes of Acute Pancreatitis
- Gallstones: Primary cause, obstructing digestive juice flow.
- Ethanol (Alcohol Abuse): Increases enzyme output and secretion viscosity.
- Trauma: Physical injury damages acinar cells.
- Hypertriglyceridemia: Clogs capillaries, leading to ischemic damage.
- Corticosteroids: Thickens secretions, raising duct obstruction risk.
- Mumps Virus: Harms both ductal and acinar cells.
- Autoimmune Conditions: Antibodies can lead to zymogen activation.
- Scorpion Stings: Rare cases leading to cell destruction.
Summary of Acute Pancreatitis
- Characterized by autodigestion of the pancreas due to obstructions or cellular damage.
- Knowledge of pancreatic anatomy and functions is vital for understanding the pathophysiology.
Causes of Acute Pancreatitis
- Certain drugs can induce pancreatitis, including:
- Sulfa Drugs: E.g., Bactrim.
- HIV Medications: NRTIs and protease inhibitors.
- Diabetic Medications: GLP-1 receptor agonists.
- ERCP: Can cause tissue damage during gallstone removal.
- Hypercalcemia: Elevated calcium stimulates enzyme activation.
Pathophysiology of Acute Pancreatitis
- Damage invokes an inflammatory response, exacerbating tissue destruction.
- Normally inactive enzymes may activate within the pancreas, leading to complications.
Symptoms of Acute Pancreatitis
- Epigastric Abdominal Pain: Constant, radiates to the back; worsens supine, improves leaning forward.
- Nausea and Vomiting: Related to inflammation and possible digestive tract obstruction.
- Jaundice: Possible if a gallstone blocks the bile duct.
Complications of Acute Pancreatitis
- Systemic Effects:
- Hypotension: Due to vasodilation and fluid loss.
- Tachycardia: Reflexive response to low blood pressure.
- Disseminated Intravascular Coagulation (DIC): Clotting disorder leading to bleeding.
- Effects on Nearby Structures: Compression may cause abdominal distension and decreased bowel sounds.
Mnemonic for Causes of Acute Pancreatitis
- "I GET SMASHED":
- I: Idiopathic
- G: Gallstones
- E: Ethanol
- T: Trauma
- S: Steroids
- M: Mumps virus
- A: Autoimmune conditions
- S: Scorpion stings
- H: Hypertriglyceridemia and hypercalcemia
- D: Drugs and ERCP.
Body Response to Inflammation
- Vasodilation and Permeability Changes:
- Lowers systemic vascular resistance and blood pressure.
- Increases vessel permeability, causing tissue edema.
- Sympathetic Nervous System Activation: Increased heart rate due to reduced blood volume.
- Cytokine Release: Inflammatory mediators inducing systemic effects like fever.
Abdominal Complications
- Ascites leading to abdominal distension from fluid accumulation.
Inflammatory Responses and Necrosis
- Damage releases proteases and lipases, causing necrosis and fat breakdown.
- Free fatty acids bind calcium, resulting in hypocalcemia from saponification.
- Formation of pancreatic pseudocysts is possible, which can become infected.
Vascular Complications
- Inflammation-related protease damage may cause hemorrhagic necrosis and bleeding.
- Retroperitoneal hemorrhage may present as Cullen's sign or Grey Turner's sign.
Diagnosis of Pancreatitis
- Classic symptoms include epigastric pain radiating to the back, nausea, and vomiting.
- Risk factors: gallstones, alcohol, hypertriglyceridemia.
- Diagnosis confirmed with elevated lipase levels; amylase can also be elevated.
- Imaging and CBC can assess the severity and identify complications.
Key Takeaways
- Close monitoring for symptoms and laboratory changes is essential in managing pancreatitis.
- Understanding potential complications aids in treatment strategy.
- Lipase testing and imaging are critical for confirming diagnosis and assessing severity.
Overview of Acute Pancreatitis
- Acute pancreatitis is an inflammatory condition affecting the pancreas, mainly its exocrine function.
- The pancreas functions as both an endocrine and exocrine gland but predominantly focuses on digestion through enzyme secretion.
Pancreatic Structure and Function
- The ductal system includes main and accessory pancreatic ducts that deliver digestive enzymes to the duodenum.
- Key components of pancreatic secretions:
- Digestive enzymes produced by acinar cells.
- Bicarbonate-rich fluid secreted by ductal cells.
Enzyme Production
- Digestive enzymes are stored as zymogens to avoid the autodigestion of pancreatic tissue.
- Types of digestive enzymes include:
- Lipases for lipid breakdown.
- Amylases for carbohydrate breakdown.
- Proteases for protein breakdown, controlled by protease inhibitors.
Mechanism of Pancreatitis Development
- Development occurs when enzyme secretion is altered, leading to autodigestion of pancreatic tissue.
- Mechanisms include:
- Obstruction of pancreatic ducts, causing pressure buildup and premature enzyme activation.
- Direct damage to acinar cells, allowing inappropriate zymogen activation.
Key Causes of Acute Pancreatitis
- Gallstones: Primary cause, obstructing digestive juice flow.
- Ethanol (Alcohol Abuse): Increases enzyme output and secretion viscosity.
- Trauma: Physical injury damages acinar cells.
- Hypertriglyceridemia: Clogs capillaries, leading to ischemic damage.
- Corticosteroids: Thickens secretions, raising duct obstruction risk.
- Mumps Virus: Harms both ductal and acinar cells.
- Autoimmune Conditions: Antibodies can lead to zymogen activation.
- Scorpion Stings: Rare cases leading to cell destruction.
Summary of Acute Pancreatitis
- Characterized by autodigestion of the pancreas due to obstructions or cellular damage.
- Knowledge of pancreatic anatomy and functions is vital for understanding the pathophysiology.
Causes of Acute Pancreatitis
- Certain drugs can induce pancreatitis, including:
- Sulfa Drugs: E.g., Bactrim.
- HIV Medications: NRTIs and protease inhibitors.
- Diabetic Medications: GLP-1 receptor agonists.
- ERCP: Can cause tissue damage during gallstone removal.
- Hypercalcemia: Elevated calcium stimulates enzyme activation.
Pathophysiology of Acute Pancreatitis
- Damage invokes an inflammatory response, exacerbating tissue destruction.
- Normally inactive enzymes may activate within the pancreas, leading to complications.
Symptoms of Acute Pancreatitis
- Epigastric Abdominal Pain: Constant, radiates to the back; worsens supine, improves leaning forward.
- Nausea and Vomiting: Related to inflammation and possible digestive tract obstruction.
- Jaundice: Possible if a gallstone blocks the bile duct.
Complications of Acute Pancreatitis
- Systemic Effects:
- Hypotension: Due to vasodilation and fluid loss.
- Tachycardia: Reflexive response to low blood pressure.
- Disseminated Intravascular Coagulation (DIC): Clotting disorder leading to bleeding.
- Effects on Nearby Structures: Compression may cause abdominal distension and decreased bowel sounds.
Mnemonic for Causes of Acute Pancreatitis
- "I GET SMASHED":
- I: Idiopathic
- G: Gallstones
- E: Ethanol
- T: Trauma
- S: Steroids
- M: Mumps virus
- A: Autoimmune conditions
- S: Scorpion stings
- H: Hypertriglyceridemia and hypercalcemia
- D: Drugs and ERCP.
Body Response to Inflammation
- Vasodilation and Permeability Changes:
- Lowers systemic vascular resistance and blood pressure.
- Increases vessel permeability, causing tissue edema.
- Sympathetic Nervous System Activation: Increased heart rate due to reduced blood volume.
- Cytokine Release: Inflammatory mediators inducing systemic effects like fever.
Abdominal Complications
- Ascites leading to abdominal distension from fluid accumulation.
Inflammatory Responses and Necrosis
- Damage releases proteases and lipases, causing necrosis and fat breakdown.
- Free fatty acids bind calcium, resulting in hypocalcemia from saponification.
- Formation of pancreatic pseudocysts is possible, which can become infected.
Vascular Complications
- Inflammation-related protease damage may cause hemorrhagic necrosis and bleeding.
- Retroperitoneal hemorrhage may present as Cullen's sign or Grey Turner's sign.
Diagnosis of Pancreatitis
- Classic symptoms include epigastric pain radiating to the back, nausea, and vomiting.
- Risk factors: gallstones, alcohol, hypertriglyceridemia.
- Diagnosis confirmed with elevated lipase levels; amylase can also be elevated.
- Imaging and CBC can assess the severity and identify complications.
Key Takeaways
- Close monitoring for symptoms and laboratory changes is essential in managing pancreatitis.
- Understanding potential complications aids in treatment strategy.
- Lipase testing and imaging are critical for confirming diagnosis and assessing severity.
Overview of Acute Pancreatitis
- Acute pancreatitis is an inflammatory condition affecting the pancreas, mainly its exocrine function.
- The pancreas functions as both an endocrine and exocrine gland but predominantly focuses on digestion through enzyme secretion.
Pancreatic Structure and Function
- The ductal system includes main and accessory pancreatic ducts that deliver digestive enzymes to the duodenum.
- Key components of pancreatic secretions:
- Digestive enzymes produced by acinar cells.
- Bicarbonate-rich fluid secreted by ductal cells.
Enzyme Production
- Digestive enzymes are stored as zymogens to avoid the autodigestion of pancreatic tissue.
- Types of digestive enzymes include:
- Lipases for lipid breakdown.
- Amylases for carbohydrate breakdown.
- Proteases for protein breakdown, controlled by protease inhibitors.
Mechanism of Pancreatitis Development
- Development occurs when enzyme secretion is altered, leading to autodigestion of pancreatic tissue.
- Mechanisms include:
- Obstruction of pancreatic ducts, causing pressure buildup and premature enzyme activation.
- Direct damage to acinar cells, allowing inappropriate zymogen activation.
Key Causes of Acute Pancreatitis
- Gallstones: Primary cause, obstructing digestive juice flow.
- Ethanol (Alcohol Abuse): Increases enzyme output and secretion viscosity.
- Trauma: Physical injury damages acinar cells.
- Hypertriglyceridemia: Clogs capillaries, leading to ischemic damage.
- Corticosteroids: Thickens secretions, raising duct obstruction risk.
- Mumps Virus: Harms both ductal and acinar cells.
- Autoimmune Conditions: Antibodies can lead to zymogen activation.
- Scorpion Stings: Rare cases leading to cell destruction.
Summary of Acute Pancreatitis
- Characterized by autodigestion of the pancreas due to obstructions or cellular damage.
- Knowledge of pancreatic anatomy and functions is vital for understanding the pathophysiology.
Causes of Acute Pancreatitis
- Certain drugs can induce pancreatitis, including:
- Sulfa Drugs: E.g., Bactrim.
- HIV Medications: NRTIs and protease inhibitors.
- Diabetic Medications: GLP-1 receptor agonists.
- ERCP: Can cause tissue damage during gallstone removal.
- Hypercalcemia: Elevated calcium stimulates enzyme activation.
Pathophysiology of Acute Pancreatitis
- Damage invokes an inflammatory response, exacerbating tissue destruction.
- Normally inactive enzymes may activate within the pancreas, leading to complications.
Symptoms of Acute Pancreatitis
- Epigastric Abdominal Pain: Constant, radiates to the back; worsens supine, improves leaning forward.
- Nausea and Vomiting: Related to inflammation and possible digestive tract obstruction.
- Jaundice: Possible if a gallstone blocks the bile duct.
Complications of Acute Pancreatitis
- Systemic Effects:
- Hypotension: Due to vasodilation and fluid loss.
- Tachycardia: Reflexive response to low blood pressure.
- Disseminated Intravascular Coagulation (DIC): Clotting disorder leading to bleeding.
- Effects on Nearby Structures: Compression may cause abdominal distension and decreased bowel sounds.
Mnemonic for Causes of Acute Pancreatitis
- "I GET SMASHED":
- I: Idiopathic
- G: Gallstones
- E: Ethanol
- T: Trauma
- S: Steroids
- M: Mumps virus
- A: Autoimmune conditions
- S: Scorpion stings
- H: Hypertriglyceridemia and hypercalcemia
- D: Drugs and ERCP.
Body Response to Inflammation
- Vasodilation and Permeability Changes:
- Lowers systemic vascular resistance and blood pressure.
- Increases vessel permeability, causing tissue edema.
- Sympathetic Nervous System Activation: Increased heart rate due to reduced blood volume.
- Cytokine Release: Inflammatory mediators inducing systemic effects like fever.
Abdominal Complications
- Ascites leading to abdominal distension from fluid accumulation.
Inflammatory Responses and Necrosis
- Damage releases proteases and lipases, causing necrosis and fat breakdown.
- Free fatty acids bind calcium, resulting in hypocalcemia from saponification.
- Formation of pancreatic pseudocysts is possible, which can become infected.
Vascular Complications
- Inflammation-related protease damage may cause hemorrhagic necrosis and bleeding.
- Retroperitoneal hemorrhage may present as Cullen's sign or Grey Turner's sign.
Diagnosis of Pancreatitis
- Classic symptoms include epigastric pain radiating to the back, nausea, and vomiting.
- Risk factors: gallstones, alcohol, hypertriglyceridemia.
- Diagnosis confirmed with elevated lipase levels; amylase can also be elevated.
- Imaging and CBC can assess the severity and identify complications.
Key Takeaways
- Close monitoring for symptoms and laboratory changes is essential in managing pancreatitis.
- Understanding potential complications aids in treatment strategy.
- Lipase testing and imaging are critical for confirming diagnosis and assessing severity.
Overview of Acute Pancreatitis
- Acute pancreatitis is an inflammatory condition affecting the pancreas, mainly its exocrine function.
- The pancreas functions as both an endocrine and exocrine gland but predominantly focuses on digestion through enzyme secretion.
Pancreatic Structure and Function
- The ductal system includes main and accessory pancreatic ducts that deliver digestive enzymes to the duodenum.
- Key components of pancreatic secretions:
- Digestive enzymes produced by acinar cells.
- Bicarbonate-rich fluid secreted by ductal cells.
Enzyme Production
- Digestive enzymes are stored as zymogens to avoid the autodigestion of pancreatic tissue.
- Types of digestive enzymes include:
- Lipases for lipid breakdown.
- Amylases for carbohydrate breakdown.
- Proteases for protein breakdown, controlled by protease inhibitors.
Mechanism of Pancreatitis Development
- Development occurs when enzyme secretion is altered, leading to autodigestion of pancreatic tissue.
- Mechanisms include:
- Obstruction of pancreatic ducts, causing pressure buildup and premature enzyme activation.
- Direct damage to acinar cells, allowing inappropriate zymogen activation.
Key Causes of Acute Pancreatitis
- Gallstones: Primary cause, obstructing digestive juice flow.
- Ethanol (Alcohol Abuse): Increases enzyme output and secretion viscosity.
- Trauma: Physical injury damages acinar cells.
- Hypertriglyceridemia: Clogs capillaries, leading to ischemic damage.
- Corticosteroids: Thickens secretions, raising duct obstruction risk.
- Mumps Virus: Harms both ductal and acinar cells.
- Autoimmune Conditions: Antibodies can lead to zymogen activation.
- Scorpion Stings: Rare cases leading to cell destruction.
Summary of Acute Pancreatitis
- Characterized by autodigestion of the pancreas due to obstructions or cellular damage.
- Knowledge of pancreatic anatomy and functions is vital for understanding the pathophysiology.
Causes of Acute Pancreatitis
- Certain drugs can induce pancreatitis, including:
- Sulfa Drugs: E.g., Bactrim.
- HIV Medications: NRTIs and protease inhibitors.
- Diabetic Medications: GLP-1 receptor agonists.
- ERCP: Can cause tissue damage during gallstone removal.
- Hypercalcemia: Elevated calcium stimulates enzyme activation.
Pathophysiology of Acute Pancreatitis
- Damage invokes an inflammatory response, exacerbating tissue destruction.
- Normally inactive enzymes may activate within the pancreas, leading to complications.
Symptoms of Acute Pancreatitis
- Epigastric Abdominal Pain: Constant, radiates to the back; worsens supine, improves leaning forward.
- Nausea and Vomiting: Related to inflammation and possible digestive tract obstruction.
- Jaundice: Possible if a gallstone blocks the bile duct.
Complications of Acute Pancreatitis
- Systemic Effects:
- Hypotension: Due to vasodilation and fluid loss.
- Tachycardia: Reflexive response to low blood pressure.
- Disseminated Intravascular Coagulation (DIC): Clotting disorder leading to bleeding.
- Effects on Nearby Structures: Compression may cause abdominal distension and decreased bowel sounds.
Mnemonic for Causes of Acute Pancreatitis
- "I GET SMASHED":
- I: Idiopathic
- G: Gallstones
- E: Ethanol
- T: Trauma
- S: Steroids
- M: Mumps virus
- A: Autoimmune conditions
- S: Scorpion stings
- H: Hypertriglyceridemia and hypercalcemia
- D: Drugs and ERCP.
Body Response to Inflammation
- Vasodilation and Permeability Changes:
- Lowers systemic vascular resistance and blood pressure.
- Increases vessel permeability, causing tissue edema.
- Sympathetic Nervous System Activation: Increased heart rate due to reduced blood volume.
- Cytokine Release: Inflammatory mediators inducing systemic effects like fever.
Abdominal Complications
- Ascites leading to abdominal distension from fluid accumulation.
Inflammatory Responses and Necrosis
- Damage releases proteases and lipases, causing necrosis and fat breakdown.
- Free fatty acids bind calcium, resulting in hypocalcemia from saponification.
- Formation of pancreatic pseudocysts is possible, which can become infected.
Vascular Complications
- Inflammation-related protease damage may cause hemorrhagic necrosis and bleeding.
- Retroperitoneal hemorrhage may present as Cullen's sign or Grey Turner's sign.
Diagnosis of Pancreatitis
- Classic symptoms include epigastric pain radiating to the back, nausea, and vomiting.
- Risk factors: gallstones, alcohol, hypertriglyceridemia.
- Diagnosis confirmed with elevated lipase levels; amylase can also be elevated.
- Imaging and CBC can assess the severity and identify complications.
Key Takeaways
- Close monitoring for symptoms and laboratory changes is essential in managing pancreatitis.
- Understanding potential complications aids in treatment strategy.
- Lipase testing and imaging are critical for confirming diagnosis and assessing severity.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the key aspects of acute pancreatitis, including its definition, pancreatic structure and functions, and enzyme production. It examines how the pancreas functions as both an endocrine and exocrine gland and the mechanisms involved in the development of pancreatitis.