Podcast
Questions and Answers
How would the removal of the anterior pituitary gland affect the ovarian cycle, and which specific hormones would be most directly impacted?
How would the removal of the anterior pituitary gland affect the ovarian cycle, and which specific hormones would be most directly impacted?
The removal of the anterior pituitary would halt the ovarian cycle due to the absence of LH and FSH. These hormones are crucial for follicular development and ovulation.
Explain the relationship between the corpus luteum and progesterone secretion, and describe what happens to both if fertilization does not occur.
Explain the relationship between the corpus luteum and progesterone secretion, and describe what happens to both if fertilization does not occur.
The corpus luteum secretes progesterone, which maintains the uterine lining. If fertilization doesn't occur, the corpus luteum degrades, causing a drop in progesterone levels, which leads to menstruation.
During a typical 28-day menstrual cycle, at what point is estrogen production highest, and what is the primary effect of this peak in estrogen on the uterus?
During a typical 28-day menstrual cycle, at what point is estrogen production highest, and what is the primary effect of this peak in estrogen on the uterus?
Estrogen production peaks just before ovulation. This high estrogen level causes the uterine lining (endometrium) to thicken in preparation for potential implantation.
How do oral contraceptives that contain synthetic progestins prevent pregnancy by affecting the ovarian cycle?
How do oral contraceptives that contain synthetic progestins prevent pregnancy by affecting the ovarian cycle?
Describe the roles of both FSH and LH in the development of a primary follicle, leading up to ovulation.
Describe the roles of both FSH and LH in the development of a primary follicle, leading up to ovulation.
Flashcards
Follicular Phase
Follicular Phase
The phase where follicles grow and develop in the ovary.
Ovulation
Ovulation
The stage where a mature follicle releases an egg.
Luteal Phase
Luteal Phase
The phase after ovulation when the corpus luteum forms.
Corpus Luteum
Corpus Luteum
Signup and view all the flashcards
Primordial Follicle
Primordial Follicle
Signup and view all the flashcards
Study Notes
- The menstrual cycle is a recurring process in females involving the ovaries and uterus, crucial for reproduction
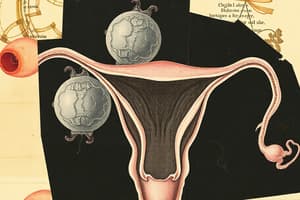
Ovarian Cycle Overview
- The ovarian cycle primarily focuses on the maturation and release of an oocyte (egg) from the ovary
- It includes follicular development, ovulation, and the formation/degeneration of the corpus luteum
- The cycle is regulated by hormones including follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
Primary Follicle Stage
- The ovarian cycle begins with primordial follicles, each containing a primary oocyte
- A primary follicle develops when the granulosa cells surrounding the primary oocyte become cuboidal in shape
- It marks the start of follicular development, driven by hormonal signals
Secondary Follicle Stage
- A primary follicle matures into a secondary follicle as the granulosa cells proliferate
- The theca cells differentiate outside of the follicle
- The oocyte is surrounded by a glycoprotein layer, the zona pellucida
Tertiary (Antral) Follicle Stage
- The tertiary follicle is distinguished by the formation of an antrum (fluid-filled cavity)
- The antrum is filled with follicular fluid, containing hormones and growth factors
- The oocyte is surrounded by the cumulus oophorus, a cluster of granulosa cells
Graafian (Mature) Follicle Stage
- The Graafian follicle is the final stage of follicular development before ovulation
- It has a large, well-formed antrum, and the oocyte is attached to the follicle wall
- The follicle is ready to release the oocyte during ovulation
Ovulation
- Ovulation is the process where the Graafian follicle ruptures and releases the secondary oocyte
- It is triggered by a surge in luteinizing hormone (LH) levels
- The oocyte is expelled from the ovary and enters the fallopian tube
Corpus Luteum Formation
- After ovulation, the remaining follicle cells transform into the corpus luteum
- Stimulated by LH, the corpus luteum primarily secretes progesterone and estrogen
- Progesterone prepares the uterine lining for potential implantation of a fertilized egg
Corpus Luteum Function
- Progesterone maintains the thickened endometrium of the uterus to support a pregnancy
- Estrogen produced by the corpus luteum also contributes to endometrial stability
- It inhibits new follicular development
Corpus Luteum Degeneration
- If fertilization does not occur, the corpus luteum degrades after approximately 14 days
- It transforms into the corpus albicans, a scar-like structure
- Progesterone and estrogen levels decline, leading to menstruation
Hormonal Control
- The ovarian cycle is regulated by the hypothalamic-pituitary-ovarian axis
- Gonadotropin-releasing hormone (GnRH) from the hypothalamus stimulates the pituitary gland to release FSH and LH
- FSH stimulates follicular development, while LH triggers ovulation and the formation/maintenance of the corpus luteum
- Estrogen and progesterone exert feedback control on the hypothalamus and pituitary to regulate the cycle
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.