Podcast
Questions and Answers
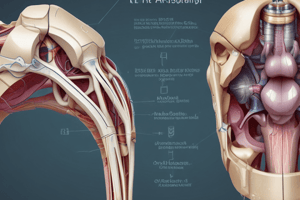
What are the two types of synovial joints?
What are the two types of synovial joints?
- Cartilagenous joints and Fibrous joints
- Synovial joints and Cartilagenous joints
- Rigid joints and Freely movable joints
- Stability joints and Mobility joints (correct)
What are three characteristics of synovial joints in the human body?
What are three characteristics of synovial joints in the human body?
- Most common joint in the human body, a direct union between bones, and surrounded by a fibrous capsule
- Most common joint in the human body, no direct union between articulating bones, and surrounded by a strong fibrous capsule (correct)
- Least common joint in the human body, a direct union between bones, and surrounded by cartilage.
- Least common joint in the human body, no direct union between articulating bones, and surrounded by a strong fibrous capsule
What is the main purpose of synovial fluid?
What is the main purpose of synovial fluid?
Synovial fluid provides lubrication to the joint, acts as a shock absorber, and provides nourishment to the articular cartilage.
Immobility of a joint can lead to a decrease in synovial fluid production.
Immobility of a joint can lead to a decrease in synovial fluid production.
What is the outer layer of the synovial joint capsule composed of?
What is the outer layer of the synovial joint capsule composed of?
What are the three main components of connective tissue?
What are the three main components of connective tissue?
What is the most abundant protein in the human body?
What is the most abundant protein in the human body?
What is the primary function of elastin?
What is the primary function of elastin?
What is the primary function of connective tissue?
What is the primary function of connective tissue?
What two factors primarily influence the susceptibility of connective tissue to injury?
What two factors primarily influence the susceptibility of connective tissue to injury?
Ligaments have a higher collagen content than tendons.
Ligaments have a higher collagen content than tendons.
What is the primary function of tendons?
What is the primary function of tendons?
The composition of the joint capsule may change depending on the stresses imposed upon it.
The composition of the joint capsule may change depending on the stresses imposed upon it.
Cartilage is a vascular tissue, meaning it has a good blood supply.
Cartilage is a vascular tissue, meaning it has a good blood supply.
What are the two main types of cartilage?
What are the two main types of cartilage?
The white fibrocartilage found in joints is often called bonding cement.
The white fibrocartilage found in joints is often called bonding cement.
Describe three characteristics of hyaline cartilage.
Describe three characteristics of hyaline cartilage.
Bone tissue can be described as rigid but also somewhat elastic.
Bone tissue can be described as rigid but also somewhat elastic.
What is Wolff's Law?
What is Wolff's Law?
Bone receives its nourishment from the capillaries within the bone itself, not from the hyaline cartilage.
Bone receives its nourishment from the capillaries within the bone itself, not from the hyaline cartilage.
What are three functions of bone tissue?
What are three functions of bone tissue?
Besides its structural roles, what other important functions does bone perform?
Besides its structural roles, what other important functions does bone perform?
Which of these is NOT a part of the bone?
Which of these is NOT a part of the bone?
What is the name of the shaft of the bone?
What is the name of the shaft of the bone?
Match the bone cell types with their functions:
Match the bone cell types with their functions:
The process of inflammation and repair is a specific response, meaning it always proceeds in the same way.
The process of inflammation and repair is a specific response, meaning it always proceeds in the same way.
What are four factors that influence the timetable for the inflammation and repair process?
What are four factors that influence the timetable for the inflammation and repair process?
What is the result of injury to soft tissue?
What is the result of injury to soft tissue?
Why does injured soft tissue not regenerate itself?
Why does injured soft tissue not regenerate itself?
Scar tissue is composed mainly of collagen.
Scar tissue is composed mainly of collagen.
What is the nonspecific repair mechanism of scar formation?
What is the nonspecific repair mechanism of scar formation?
What are the three phases of the inflammation and repair process?
What are the three phases of the inflammation and repair process?
During the inflammation phase, the injured area swells and becomes warm.
During the inflammation phase, the injured area swells and becomes warm.
The inflammation phase is initiated by the release of histamine.
The inflammation phase is initiated by the release of histamine.
What is the primary function of leukocytes during the second stage of inflammation?
What is the primary function of leukocytes during the second stage of inflammation?
What are the four main clinical manifestations of inflammation?
What are the four main clinical manifestations of inflammation?
What is the treatment protocol for the acute stage of injury, often referred to as the maximum protection phase?
What is the treatment protocol for the acute stage of injury, often referred to as the maximum protection phase?
Describe the role of fibroblasts during the fibroplasia phase of tissue repair.
Describe the role of fibroblasts during the fibroplasia phase of tissue repair.
The synthesis, orientation, and deposition of new collagen during the fibroplasia phase is initially random.
The synthesis, orientation, and deposition of new collagen during the fibroplasia phase is initially random.
Fibroblasts disappear when enough scar tissue is laid down, marking the beginning of the remodeling phase.
Fibroblasts disappear when enough scar tissue is laid down, marking the beginning of the remodeling phase.
What is the treatment protocol commonly used during the subacute phase of injury?
What is the treatment protocol commonly used during the subacute phase of injury?
What happens during the scar maturation phase?
What happens during the scar maturation phase?
Physical therapy plays a pivotal role in promoting correct scar tissue remodeling.
Physical therapy plays a pivotal role in promoting correct scar tissue remodeling.
The strength and extensibility of the final scar tissue are largely determined by the patient's diligence with their home exercise program.
The strength and extensibility of the final scar tissue are largely determined by the patient's diligence with their home exercise program.
Despite the remodeling process, scar tissue is never as strong as the tissue it replaces.
Despite the remodeling process, scar tissue is never as strong as the tissue it replaces.
Striated muscles are capable of regenerating myofibrils to restore full function after injury.
Striated muscles are capable of regenerating myofibrils to restore full function after injury.
What are the three grades of muscle strains?
What are the three grades of muscle strains?
Tendons require that the injured ends are brought together and the gliding function restored.
Tendons require that the injured ends are brought together and the gliding function restored.
What are the three terms used to describe tendon injuries?
What are the three terms used to describe tendon injuries?
What are the three grades of ligament sprains?
What are the three grades of ligament sprains?
Mature cartilage is capable of regenerating itself.
Mature cartilage is capable of regenerating itself.
Nerve injuries may heal if the cell body is not affected and the ends of the axon are close together.
Nerve injuries may heal if the cell body is not affected and the ends of the axon are close together.
Physical therapy interventions and progressions must be based on the physiologic responses of the tissues to injury and on an understanding of how various tissues heal.
Physical therapy interventions and progressions must be based on the physiologic responses of the tissues to injury and on an understanding of how various tissues heal.
As PTAs, it's important to understand the healing process to effectively supervise the rehab process.
As PTAs, it's important to understand the healing process to effectively supervise the rehab process.
Flashcards
Stability Joints
Stability Joints
Articulating surfaces are congruent, dense, thick joint capsule, and many ligaments for support.
Mobility Joints
Mobility Joints
Articulating surfaces are incongruent, loose capsule, and very few ligaments.
Synovial Joint Characteristics
Synovial Joint Characteristics
Most common type of joint in the human body, no direct union between articulating bones, surrounded by a strong fibrous capsule.
Synovial Fluid Purpose
Synovial Fluid Purpose
Signup and view all the flashcards
Stratum Fibrosum
Stratum Fibrosum
Signup and view all the flashcards
Stratum Synovium
Stratum Synovium
Signup and view all the flashcards
Effects of Immobilization
Effects of Immobilization
Signup and view all the flashcards
Cartilage
Cartilage
Signup and view all the flashcards
White Fibrocartilage
White Fibrocartilage
Signup and view all the flashcards
Yellow Fibrocartilage
Yellow Fibrocartilage
Signup and view all the flashcards
Hyaline Cartilage
Hyaline Cartilage
Signup and view all the flashcards
Bone Tissue Characteristics
Bone Tissue Characteristics
Signup and view all the flashcards
Wolff's Law
Wolff's Law
Signup and view all the flashcards
Bone Nourishment
Bone Nourishment
Signup and view all the flashcards
Epiphysis
Epiphysis
Signup and view all the flashcards
Diaphysis
Diaphysis
Signup and view all the flashcards
Metaphysis
Metaphysis
Signup and view all the flashcards
Osteoblasts
Osteoblasts
Signup and view all the flashcards
Osteoclasts
Osteoclasts
Signup and view all the flashcards
Osteocyte
Osteocyte
Signup and view all the flashcards
Tissue Response to Injury
Tissue Response to Injury
Signup and view all the flashcards
Connective Tissue Repair
Connective Tissue Repair
Signup and view all the flashcards
Scar Tissue
Scar Tissue
Signup and view all the flashcards
Inflammation Phase
Inflammation Phase
Signup and view all the flashcards
Inflammation
Inflammation
Signup and view all the flashcards
Fibroplasia
Fibroplasia
Signup and view all the flashcards
Scar Maturation
Scar Maturation
Signup and view all the flashcards
Stretching exercises
Stretching exercises
Signup and view all the flashcards
Strengthening exercises
Strengthening exercises
Signup and view all the flashcards
Isometric exercises
Isometric exercises
Signup and view all the flashcards
Stabilization exercises
Stabilization exercises
Signup and view all the flashcards
Study Notes
Orthopedics: Disabilities and Treatment
- Orthopedic surgery and research are constantly evolving.
- Athletes of all ages and sizes compete at various levels.
- Workman's compensation is relevant to workplace injuries.
- Geriatric considerations relate to older adults' health.
- Traumatic injuries are a significant concern.
- The anatomy of the body's various components is crucial to orthopedic practices.
Synovial Joint Classification
- Stability Joints:
- Articulating surfaces are congruent.
- Have a dense, thick capsule.
- Supported with numerous ligaments.
- Mobility Joints:
- Articulating surfaces are incongruent.
- Have a loose capsule.
- Supported with very few ligaments.
- Synovial Joint Characteristics:
- The most common joint type.
- No direct connection between bones,
- Surrounded by a strong fibrous capsule.
- Allows for free motion of the joint.
- A synovial membrane secretes synovial fluid.
- Hyaline cartilage covers articular surfaces, decreasing friction.
Synovial Joint Components
- Includes stratum fibrosum (outer layer)
- Dense fibrous tissue
- Poorly vascularized
- Richly innervated by joint receptors that detect:
- Compression or tension
- Pain
- Movement (rate and direction)
- Vibration
- Includes stratum synovium (inner layer)
- Highly vascularized
- Poorly innervated
- Purpose is to produce synovial fluid.
Purpose of Synovial Fluid
- Lubricates the joint.
- Acts as a shock absorber.
- Nourishes articular cartilage.
Effects of Immobilization (on Synovial Fluid)
- No synovial fluid is produced when a joint is immobilized.
- This leads to lack of nourishment for the hyaline cartilage.
- This will result in osteoarthritis.
Hyaline Cartilage
- Crucial for joint movement and health.
- Is avascular, causing slow or limited repair capabilities.
Joint Capsule and Supporting Tissue
- Adaptive shortening occurs due to disuse atrophy.
- Disuse atrophy causes muscle and ligament weakness.
- Diseases or injuries can cause joint/muscle contractures.
Ligaments / Tendons / Stratum Fibrosum
- Makeup of connective tissue.
- Collagen
- Elastin
- Collagen/Elastin Mix
Collagen
- A main component of fibrous connective tissue.
- The most abundant protein.
- High tensile strength.
Elastin
- Provides elastic properties.
- Allows fibers to deform and return to their original shape.
Collagen/Elastin Mix
- Synovial joints primarily consist of both collagen and elastin.
- Proportion of elastin to collagen varies depending on the joint.
- Elastin is a smaller portion of the fibrous component.
Function of Connective Tissue
- Maintains the joint's stability.
Susceptibility to Injury (of Joints)
- Susceptibility depends on the elastin amount and arrangement of collagen fibers.
- Ligaments have more elastin than tendons.
Tendons
- Higher collagen content.
- Collagen has a parallel arrangement suitable for high unidirectional tensile forces to be withstood.
Joint Capsule
- Varies greatly in composition.
- The composition changes depending on stresses imposed.
- Joints designed for stability have more collagen than joints designed for mobility.
Cartilage (Overview)
- Solid type of connective tissue.
- Avascular (no blood supply) limits its repair capability.
Cartilage Types
- Fibrocartilage:
- Forms joints that permit little motion.
- Forms intervertebral discs.
- White fibrocartilage.
- Yellow fibrocartilage.
- Hyaline Cartilage (Articular):
- Most abundant cartilage type.
- Forms a thin covering on many bones.
- Resilient, smooth, and low friction.
- Crucial for articulation between bones.
- Consists of three distinct layers or zones.
Bone Tissue Characteristics
- Hardest form of connective tissue.
- Composed of fibrous connective tissue and inorganic substances.
- Somewhat elastic despite its rigidity.
Wolff's Law
- Bone deposition occurs in areas of stress.
- Bone resorption occurs in areas of reduced stress.
- Bone models and remodels throughout life in response to stress.
Bone Nourishment
- Bone receives nourishment from capillaries within the bone, not from hyaline cartilage.
Bone Function
- Provides a rigid framework.
- Serves as levers.
- Protects vulnerable internal organs
- Contains sites for blood cell development.
- Acts as a mineral reservoir for the body.
Bone Terms
- Epiphysis: The distal end of a bone.
- Diaphysis: The shaft of a bone; a hollow tube of compact bone surrounding the medullary cavity.
- Metaphysis: The region where the diaphysis and epiphysis meet in mature bones.
Bone Cells
- Osteoblasts: Produce bone tissue.
- Osteoclasts: Resorb bone tissue.
- Osteocytes: Mature osteoblasts embedded within the bone matrix.
Tissue Response to Injury
- Injury to soft tissue initiates a series of responses collectively known as inflammation and repair.
Timeline for Tissue Healing
- The timetable is variable for each patient.
- Factors like injury extent, disease, and medications impact the healing process.
Healing Process (Soft Tissue)
- Injured soft tissue does not regenerate; repair occurs instead.
- Healing is nonspecific, with scar tissue replacing the damaged tissues.
- Scar tissue is mainly collagen, which is rigid and limits motion.
Components of Inflammation and Repair
- Inflammation Phase: Area swells and becomes warm.
- Rid the area of microorganisms, foreign matter, and debris.
- Preparing the area for repair.
- Characterized by four symptoms: pain, redness, warmth, and swelling.
- Fibroplasia Phase: Formation of new fibrous connective tissue.
- Scar Maturation Phase: Remodeling of connective tissue.
Inflammation Phase (Stages)
- 1st stage: immediate vasoconstriction followed by vasodilation, platelet aggregation and clot formation.
- 2nd stage: infiltration of leukocytes, like neutrophils, monocytes, and macrophages, to phagocytose debris.
- 3rd stage: Release of growth factors by macrophages to stimulate epithelial cell growth, angiogenesis, and fibroblast attraction.
Treatment for Acute Stage (of Injury)
- PRICE: Protection, Rest, Ice, Compression, Elevation.
Subacute Phase (Treatment Stages)
- Continuing with ROM (range of motion) exercises, stretching.
- Beginning strengthening exercises (like isometrics, using therabands, and stabilization exercises).
- Exercise programs progress gradually.
Scar Maturation (Remodeling) Phase
- New collagen and connective tissue gradually reorganize along the lines of physical stress.
- Active stress or muscular contractions, with progressive joint motion (PROM > AAROM > AROM), promote organized, stronger, more functional collagen arrangements.
Remodeling Phase (Return to Activity)
- Aggressive ROM and strengthening exercises.
- Regaining activity-specific skills.
Physical Therapy Role
- Physical therapy is crucial for scar tissue remodeling and improving tensile strength.
- The more organized collagen fibers, the stronger the tensile strength.
Additional Notes
- The final scar strength and extensibility depend greatly on the patient's diligence in home exercises.
- Despite remodeling, scar tissue is never as strong as the original tissue.
Specialized Tissue Repair
- Striated muscle. -Limited ability to regenerate myofibrils. -Edges must be closely approximated for repair. -Scar formation will occur to heal wound tissue.
- Nerves.
- If the cell body and axon ends are close together, the nerve may heal.
- Healing is very slow (3-4 mm per day).
- Some cartilages have some regeneration abilities.
-Mature cartilage cannot regenerate.
- Will often lose anatomical characteristics.
- Will lose cushion abilities.
Sprains
- Grade I, II, and III sprains
Strains
- Grade I, II, and III strains
Ligaments
- Treatment of ruptures and avulsions (rupture has same repair process as tendons)
- Fixation with screws for avulsions
Tendons
- Repair treatment.
- Union of severed ends required.
- Prevent tendon sheath adhesions.
Terms (related to tendons)
- Tendinitis
- Tendinosis
- Tenosynovitis
Orthopaedic Considerations in Various Populations (general concepts)
- Athletes: Injury prevention and rehabilitation programs required.
- Workers: Workman's compensation and injury prevention.
- Geriatric patients: Special considerations in treatment and care.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.