Podcast
Questions and Answers
Which characteristic distinguishes the mucosa of the anterior two-thirds of the tongue from the posterior one-third?
Which characteristic distinguishes the mucosa of the anterior two-thirds of the tongue from the posterior one-third?
- The anterior two-thirds is derived from endoderm.
- The anterior two-thirds is derived from ectoderm. (correct)
- The anterior two-thirds is termed lymphatic.
- The anterior two-thirds contains extensive lymphoid nodules.
Which statement accurately describes filiform papillae?
Which statement accurately describes filiform papillae?
- They are not arranged in parallel rows.
- They facilitate mastication through mechanical functions. (correct)
- They are mushroom-shaped.
- They contain numerous taste buds.
The reddish appearance of fungiform papillae is primarily attributed to which characteristic?
The reddish appearance of fungiform papillae is primarily attributed to which characteristic?
- The thick keratinized epithelium covering the surface.
- The presence of Von Ebner's glands.
- The lack of connective tissue core.
- The thin nonkeratinized epithelium and rich capillary network. (correct)
What is the primary function of the serous salivary gland ducts associated with circumvallate papillae, known as Von Ebner's glands?
What is the primary function of the serous salivary gland ducts associated with circumvallate papillae, known as Von Ebner's glands?
Foliate papillae are characterized by which feature?
Foliate papillae are characterized by which feature?
Which lingual papillae type does not typically contain taste buds?
Which lingual papillae type does not typically contain taste buds?
Taste buds are typically found in all of the following locations except:
Taste buds are typically found in all of the following locations except:
Which of the following best describes the structure of taste buds?
Which of the following best describes the structure of taste buds?
What is the role of neuroepithelial cells within taste buds?
What is the role of neuroepithelial cells within taste buds?
Which taste sensation is primarily detected at the tip of the tongue?
Which taste sensation is primarily detected at the tip of the tongue?
Which cranial nerve mediates taste sensations of the posterior one-third of the tongue?
Which cranial nerve mediates taste sensations of the posterior one-third of the tongue?
What histological feature characterizes the lingual crypts found in the posterior third of the tongue?
What histological feature characterizes the lingual crypts found in the posterior third of the tongue?
Which glands are associated with the lingual follicles in the posterior third of the tongue?
Which glands are associated with the lingual follicles in the posterior third of the tongue?
Which main tissue components form the dentogingival junction?
Which main tissue components form the dentogingival junction?
What is the fate of the reduced enamel epithelium after the ameloblasts have completed enamel formation?
What is the fate of the reduced enamel epithelium after the ameloblasts have completed enamel formation?
What structure is formed by the fusion of the reduced enamel epithelium and the oral epithelium during tooth eruption?
What structure is formed by the fusion of the reduced enamel epithelium and the oral epithelium during tooth eruption?
Which term describes the reduced enamel epithelium after the crown of the tooth emerges into the oral cavity?
Which term describes the reduced enamel epithelium after the crown of the tooth emerges into the oral cavity?
How does the gingival sulcus form during tooth eruption?
How does the gingival sulcus form during tooth eruption?
Which statement best describes the sulcular epithelium?
Which statement best describes the sulcular epithelium?
What characteristic of junctional epithelium facilitates the easy passage of neutrophils and crevicular fluid?
What characteristic of junctional epithelium facilitates the easy passage of neutrophils and crevicular fluid?
What event defines active eruption?
What event defines active eruption?
What is the term for the separation of the primary attachment epithelium from the enamel surface?
What is the term for the separation of the primary attachment epithelium from the enamel surface?
In the context of the attachment epithelium, what defines the first stage of apical migration?
In the context of the attachment epithelium, what defines the first stage of apical migration?
What event characterizes the fourth stage of apical migration of the attachment epithelium?
What event characterizes the fourth stage of apical migration of the attachment epithelium?
In the first and second stages of apical migration, how does the size of the clinical crown compare to the anatomic crown?
In the first and second stages of apical migration, how does the size of the clinical crown compare to the anatomic crown?
Around how many days of gestation does the primitive oral cavity develop in human embryos?
Around how many days of gestation does the primitive oral cavity develop in human embryos?
Which embryonic germ layer gives rise to the epithelium covering the hard palate and anterior two-thirds of the tongue?
Which embryonic germ layer gives rise to the epithelium covering the hard palate and anterior two-thirds of the tongue?
Approximately how many weeks into gestation does the lingual epithelium begin to show specialization with the appearance of circumvallate and foliate papillae?
Approximately how many weeks into gestation does the lingual epithelium begin to show specialization with the appearance of circumvallate and foliate papillae?
What changes are typically observed in the oral mucosa with age?
What changes are typically observed in the oral mucosa with age?
Which of the following oral complaints is more common in elderly patients, particularly postmenopausal women?
Which of the following oral complaints is more common in elderly patients, particularly postmenopausal women?
The color of the vermilion border is red due to many factors. Which of the following is one of these factors?
The color of the vermilion border is red due to many factors. Which of the following is one of these factors?
What is the clinical significance of increased redness in the alveolar mucosa compared to the skin?
What is the clinical significance of increased redness in the alveolar mucosa compared to the skin?
Which feature distinguishes the oral mucosa from skin in terms of glandular components?
Which feature distinguishes the oral mucosa from skin in terms of glandular components?
What are Fordyce's spots?
What are Fordyce's spots?
What is linea alba?
What is linea alba?
Why is the floor of the mouth suited for rapid absorption of some medications?
Why is the floor of the mouth suited for rapid absorption of some medications?
Which of the following best describes why lining mucosa gapes when surgically incised?
Which of the following best describes why lining mucosa gapes when surgically incised?
What is the effect of massaging the gingiva or brushing on keratinization?
What is the effect of massaging the gingiva or brushing on keratinization?
What is the difference between keratosis and parakeratosis?
What is the difference between keratosis and parakeratosis?
Where are nerve endings most concentrated in the oral cavity?"
Where are nerve endings most concentrated in the oral cavity?"
Flashcards
Superior tongue surface
Superior tongue surface
The superior surface of the tongue is rough and irregular.
Tongue division
Tongue division
The tongue is divided into anterior two thirds (body) and posterior one third (base).
Filiform papillae
Filiform papillae
Numerous cone-shaped fine pointed papillae that covers the anterior part of the tongue. They facilitate mastication.
Function of Filiform papillae
Function of Filiform papillae
Signup and view all the flashcards
Fungiform papillae
Fungiform papillae
Signup and view all the flashcards
Circumvallate papillae
Circumvallate papillae
Signup and view all the flashcards
Foliate papillae
Foliate papillae
Signup and view all the flashcards
Taste buds
Taste buds
Signup and view all the flashcards
Supporting cells
Supporting cells
Signup and view all the flashcards
Neuroepithelial cells
Neuroepithelial cells
Signup and view all the flashcards
Foramen cecum
Foramen cecum
Signup and view all the flashcards
Lymph nodules
Lymph nodules
Signup and view all the flashcards
Dentogingival junction
Dentogingival junction
Signup and view all the flashcards
Reduced enamel epithelium
Reduced enamel epithelium
Signup and view all the flashcards
Shift of dentogingival junction
Shift of dentogingival junction
Signup and view all the flashcards
Migration of attachment epithelium
Migration of attachment epithelium
Signup and view all the flashcards
Gingival sulcus on enamel
Gingival sulcus on enamel
Signup and view all the flashcards
Endoderm
Endoderm
Signup and view all the flashcards
Age Changes
Age Changes
Signup and view all the flashcards
Age changes in elderly women
Age changes in elderly women
Signup and view all the flashcards
Clinical consideration
Clinical consideration
Signup and view all the flashcards
Salivary glands
Salivary glands
Signup and view all the flashcards
Sebaceous glands
Sebaceous glands
Signup and view all the flashcards
linea alba
linea alba
Signup and view all the flashcards
Regular massaging
Regular massaging
Signup and view all the flashcards
Study Notes
- The oral mucous membrane lecture covers macro/micro anatomy, Lingual papillae, taste buds, dentogingival junction, changes, and clinical considerations.
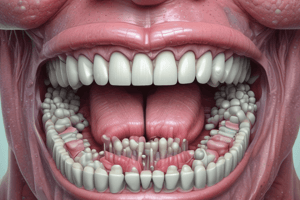
Macroanatomy of the Dorsal Surface of the Tongue
- The tongue's superior surface is rough and irregular.
- The tongue's mucous membrane has different embryologic origins and is divided by the V-shaped groove, also known as the sulcus terminalis or terminal groove.
- The anterior two thirds of the tongue, also known as the body, is derived from the ectoderm of the first pharyngeal arch and is termed “papillary."
- The posterior one third, also known as the base, is derived from the endoderm of the third pharyngeal arch; it is termed “lymphatic."
- The lymphatic section contains extensive nodules of lymphoid tissue- the lingual tonsils.
Types of Lingual Papillae
- Filliform
- Fungiform
- Circumvallate
- Foliate
Filiform Papillae
- Numerous cone-shaped fine pointed papillae, which make up most of the papillae, cover the anterior part of the tongue.
- They are about 2 to 3 mm high from the tongue's surface and arranged in parallel rows toward the midline.
- Histologically, it has a connective tissue core covered by keratinized stratified squamous epithelium, which becomes thicker at its tips, forming tufts at the apex.
- These do not contain taste buds but have mechanical functions that facilitate mastication.
Fungiform Papillae
- Round, reddish prominence, mushroom-shaped interspersed between the filiform papillae, protrude the tongue's surface.
- Few in number but more numerous near the tongue tip.
- Histologically, it has a connective tissue core rich in capillaries.
- The superior surfaces are covered by a thin nonkeratinized epithelium, but the lateral surfaces are covered by keratinized epithelium.
- One to three taste buds are on the superior surfaces of each papilla.
- A rich capillary network visible through the nonkeratinized epithelium gives it its color, which facilitates taste sensation.
Circumvallate Papillae (Walled Papilla)
- 8 to 10 papillae are in front of the V-shaped terminal sulcus.
- Large approx 3mm in diameter.
- They do not protrude above the tongue's surface but are bounded by a deep circular furrow, connecting them to the tongue's substances by a narrow base.
- Histologically, superior surfaces have keratinized epithelium.
- The lateral surfaces are covered by nonkeratinized epithelium that contains numerous taste buds.
- The ducts of Von Ebner’s serous salivary gland open into the trough, washing out the soluble food elements, also becoming the main source of salivary lipase.
Foliate Papillae
- Present on the lateral border of the posterior parts of the tongue, appearing as parallel clefts typically 4-11 papillae.
- They bound narrow folds of the mucous membrane and contain a few taste buds on their lateral walls.
Taste Buds
- Small, barrel-shaped intraepithelial organs that extend from the basal lamina to the epithelium's surface.
- They are about 80 μm high and 40 μm thick and found on the dorsal surface of the tongue in all papillae except filiform and also seen on the soft palate, epiglottis, larynx, and pharynx.
- The surface is covered by flat cells, which surround a small opening called the taste pore.
- Each taste bud may have more than one taste pore.
- Taste buds contain supporting, neuroepithelial, and basal cells
Primary Taste Sensation
- The sensations are sweet, salty, bitter, and sour.
- Sweet: at the tip of the tongue, by fungiform papillae.
- Salty: anteriorly, at the lateral border of the tongue, also by fungiform papillae.
- Bitter: in the middle part of the tongue and soft palate by circumvallate papillae and taste buds.
- Sour: posteriorly, at the lateral border of the tongue via foliate papillae.
- Sweet and salty are mediated by the chorda tympani nerve (branch of the facial nerve).
- Bitter and sour sensations are mediated by the glossopharyngeal nerve.
Posterior Third of the Tongue
- The foramen cecum represents remnants of the thyroglossal duct on the tongue at the angle of the V-shaped terminal groove.
- Posterior to the terminal sulcus is irregular and studded with rounded or oval prominences (the lingual follicles).
- Lymph nodules contain a germinal center, with a small pit at the center, the lingual crypts, lined by nonkeratinized stratified squamous epithelium.
- Lymphocytes migrate to the crypts through the epithelium.
- Ducts of the small posterior lingual mucous glands (Weber glands) open into the crypts.
- The lingual follicles together form the lingual tonsils.
Dentogingival Junction
- Formed of gingival epithelium, sulcular epithelium, junctional epithelium, and connective tissue components.
Development of Junctional Epithelium
- After ameloblasts form enamel they secrete a basal lamina, develop hemidesmosomes, and attach to the enamel surface, via the primary enamel cuticle.
- Ameloblasts then shorten, and the enamel organ reduces to a few layers called the reduced enamel epithelium.
- This reduced enamel epithelium covers the entire enamel surface and remains attached to the primary enamel cuticle.
- During eruption, the tip of the tooth approaches the oral mucosa and the reduced enamel epithelium and oral epithelium meet and fuse.
- The remnant of the primary enamel cuticle post eruption is Nasmyth’s membrane.
- The epithelium that covers the tip of the crown degenerates in its center, then the crown emerges through the epithelium-lined canal without hemorrhage.
- The reduced enamel epithelium remains attached to the part of enamel that has not yet erupted.
Primary Attached Epithelium
- Once the tip of the crown emerges, the reduced enamel epithelium forms the primary attached epithelium.
- The reduced enamel epithelium becomes gradually shorter as the tooth erupts.
- A shallow groove, the gingival sulcus, may develop between the gingiva and the tooth’s surface and extend around its circumference.
- The attachment epithelium bounds its base, as well as the gingival margin laterally.
Gingival Epithelium
- Keratinized stratified squamous epithelium.
- The gingival sulcus is a shallow groove between the tooth and the normal gingiva that extends from the free surface of the junctional epithelium coronally to the level of the free gingival margin, averagely 1.8 mm deep.
- Sulcus deepening is called a periodontal pocket.
- The bottom of the sulcus is usually on the cervical half of the anatomical crown but with age, the sulcus bottom gradually migrates.
Sulcular Epithelium
- Nonkeratinized stratified squamous epithelium, with few layers in thickness.
- Lacks epithelial ridges, forming a smooth interface with the lamina propria.
- It is thinner than gingival epithelium.
Junctional Epithelium
- Non-differentiating, nonkeratinizing lining, which forms a collar around the tooth.
- Made of a layer of flattened squamous cells parallel to the teeth surfaces, supported by straight basement membrane toward the CT (external basal lamina).
- The surface cells attach the gingiva to the tooth via hemidesmosomes and basal lamina (internal basal lamina).
- The intermediate filaments differ from those found in keratinizing oral epithelia.
- Turnover rate of 5–6 days, therefore it regenerates readily.
- It has high permeability and large intercellular spaces to allow neutrophils to flow and crevicular (gingival) fluid easily.
Shift of the Dentogingival Junction
- At first, after the tip of the enamel emerges through the mucous membrane, the epithelium covers almost the entire enamel.
- The tooth then erupts until it reaches the occlusal plane.
- The attachment epithelium then separates gradually as the crown emerges into the oral cavity.
- Later, when the tooth reaches the occlusal plane, 1/3 or 1/4 of the enamel remains covered by the gingiva.
- The teeth's actual movements toward the occlusal plane are active eruption.
- The separation of the primary attachment epithelium from the enamel is passive eruption, allowing further separation with aging and gum recession.
Migration of Attachment Epithelium
- The apical migration of the sulcus is due to basal cell detachment, which occurs when the junctional epithelium moves apically, replicating a new basal lamina and reestablishing epithelial attachment.
- The four stages of apical migration of epithelial attachment are:
- First stage: The bottom of the gingival sulcus is on the enamel, while the apical end of the attachment epithelium stays at the cement-enamel junction. Persists up to one year of age in primary teeth and 20-30 years of age In permanent teeth.
- Second stage: The bottom of the gingival sulcus remains on the enamel, while the apical end of the attachment epithelium has shifted to the surfaces of the cementum, which may persist to the age of 40 years.
- Third stage: The bottom of the gingival sulcus is at the cement-enamel junction; also, the epithelium attachment is entirely on the cementum.
- The clinical enamel is fully exposed.
- Fourth stage:
- Gingival recession occurs, and the entire attachment is on the cementum.
- The rate of crown exposure and recession varies in different persons, where the 4th stage may be observed in persons in their 20's, while another can remain in the 1st or 2nd stage after 50 years.
- In the first and second stages, the clinical crown is smaller than the anatomic crown.
- In the third stage, the clinical crown is equal to the anatomic crown.
- In the fourth stage, the clinical crown is larger than the anatomical crown due to gingival recession and part of the root being exposed.
Development of the Oral Mucosa
- Primitive oral cavity develops by fusion of the embryonic stomodeum with the foregut after rupture of the buccopharyngeal membrane at ~26 days of gestation.
- The result is the formation of a lining derived from ectoderm and endoderm.
- The endoderm forms the posterior third of the tongue, floor of the mouth, palato-glossal folds, and soft palate.
- The epithelium covering the hard palate, cheeks, gingiva, lip, and anterior 2/3 of the tongue originates from the ectoderm.
- At weeks 5-6 of gestation, the primitive oral cavity has an epithelium with two layers.
- By eight weeks, thickening occurs in the region of the vestibular dental lamina complex.
- At weeks 10-14, the oral vestibule develops.
- Specialization of the lingual epithelium occurs at around seven weeks.
- Circumvallate and foliate papillae appear, followed by fungiform papillae.
- Taste buds develop within these papillae.
- Filiform papillae appear at approximately ten weeks.
- Between weeks 8-12, capillary buds and collagen fibers can be detected.
Age Change of Oral Mucosa
- The epithelium appears thinner with flat epithelial ridges.
- The surface of the oral mucosa becomes smoother and drier.
- The tongue's surface becomes smoother and dryer.
- A reduced number of filiform papillae exaggerate the appearance of fungiform papillae.
- Vascular changes and development of varicosities can be prominent.
- Fordyce’s spots of the lips and cheeks increase.
- Elderly patients, particularly postmenopausal women, may have symptoms of mouth dryness, burning sensations, and abnormal taste.
Clinical Consideration
- The oral mucosa is more deeply colored than the skin; the vermilion border of the lips is red.
- Gingiva is pale pink, alveolar mucosa is red, and the soft palate is red, with this coloration resulting from combined factors.
- The concentration and state of dilation of small blood vessels in the underlying connective tissue.
- The thickness of the epithelium with the degree of keratinization.
- The amount of melanin pigment in the epithelium.
- Color gives an indication as to the clinical condition of the mucosa.
Clinical Notes
- The oral mucosa has a moister surface than skin.
- Skin contains numerous sebaceous glands, and sweat glands
- Oral mucosa is represented primarily by the minor salivary glands.
- Salivary glands concentrate in various regions of the oral cavity, and the openings of their ducts at the mucosal surface are sometimes evident on clinical examination.
- Sebaceous glands are present in the upper lip and buccal mucosa in about three-quarters of adults and have been described occasionally in the alveolar mucosa and dorsum of the tongue.
- Sebaceous glands appear as pale-yellow spots, known as Fordyce’s spots.
- Healthy gingiva: pattern of fine surface stippling.
- The linea alba (white line) is a keratinized region that may represent the effect of abrasion from rough tooth restorations or cheek biting.
- Local injections of anesthetics or biopsies of oral mucosa are easier to perform in loose lining mucosa.
- Injection into masticatory mucosa is more difficult and painful.
- Lining mucosa gapes when surgically incised because it is loosely bound, requiring suturing.
- Masticatory mucosa does not cause gaping wounds due to the firmness of its attachment.
- Accumulation of fluid with inflammation is painful in masticatory mucosa, but in lining mucosa, the fluid disperses and, as such, may not be very apparent.
- Permeability of oral mucosa varies: the floor of the mouth is for rapid absorption because the epithelium is thin and nonkeratinized.
- Capillaries present in the dermis are near the surface of the mucosa.
Factors Affecting Keratinization
- Regular massaging of the gingiva or brushing
- Oral mucosa keratinizes due to continuous stress of friction, such as in the linea alba.
- The palate of smokers becomes hyperkeratotic.
- The presence of mild inflammation increases keratinization; however, inflammation reduces keratinization.
Keratosis and Parakeratosis
- Keratosis: keratinization occurring in normally non-keratinized tissue
- Parakeratosis: where normally keratinized tissue such as the epidermis becomes parakeratinized.
- Nerve endings are at their maximum in the anterior portion of the oral cavity and lips and taste food to a higher degree when compared to the posterior part.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.