Podcast
Questions and Answers
What is the characteristic of arterial hemorrhage?
What is the characteristic of arterial hemorrhage?
- Bright red, continuous
- Bright red, spurting/pulsatile (correct)
- Dark red, continuous
- Dark red, spurting/pulsatile
What type of bleeding occurs 7-10 days after surgery?
What type of bleeding occurs 7-10 days after surgery?
- Reactionary hemorrhage
- Capillary hemorrhage
- Secondary hemorrhage (correct)
- Primary hemorrhage
Which of the following is a factor contributing to intraoperative bleeding?
Which of the following is a factor contributing to intraoperative bleeding?
- Antibiotics
- Hypertension (correct)
- Anesthesia
- Hypotension
What is associated with many significant abnormalities of the coagulation system?
What is associated with many significant abnormalities of the coagulation system?
What type of bleeding is characterized by dark red, continuous bleeding?
What type of bleeding is characterized by dark red, continuous bleeding?
What type of bleeding occurs during surgery and is usually the result of the incision, retraction, or preparation of the soft or hard tissue?
What type of bleeding occurs during surgery and is usually the result of the incision, retraction, or preparation of the soft or hard tissue?
What is the primary reason for the risk of aspiration during dental implant procedures?
What is the primary reason for the risk of aspiration during dental implant procedures?
What is the most likely outcome if the swallowed object is not removed from the stomach?
What is the most likely outcome if the swallowed object is not removed from the stomach?
What is the primary symptom of aspiration into the lungs?
What is the primary symptom of aspiration into the lungs?
What is the first step in treating a patient who has lost an instrument in their mouth?
What is the first step in treating a patient who has lost an instrument in their mouth?
What is the purpose of using floss ligatures to all possible implant components?
What is the purpose of using floss ligatures to all possible implant components?
What is the primary function of a pharyngeal screen during a dental implant procedure?
What is the primary function of a pharyngeal screen during a dental implant procedure?
What is the recommended minimum distance from the adjacent tooth root or tooth structure when placing an implant?
What is the recommended minimum distance from the adjacent tooth root or tooth structure when placing an implant?
What is the primary reason for antibiotic therapy in patients with emphysema who have undergone oral implantology?
What is the primary reason for antibiotic therapy in patients with emphysema who have undergone oral implantology?
What is the likely consequence of placing an implant too close to an adjacent tooth root?
What is the likely consequence of placing an implant too close to an adjacent tooth root?
What is the average time frame for resolution of emphysema following oral implantology?
What is the average time frame for resolution of emphysema following oral implantology?
What is the primary purpose of supportive therapy in patients with emphysema following oral implantology?
What is the primary purpose of supportive therapy in patients with emphysema following oral implantology?
What is the main cause of insufficient implant–root apex distance?
What is the main cause of insufficient implant–root apex distance?
What should be done to treat moderate to severe pain that is expected or persists?
What should be done to treat moderate to severe pain that is expected or persists?
Why should patients be advised to avoid using a straw when drinking fluids?
Why should patients be advised to avoid using a straw when drinking fluids?
What should patients be instructed to do to reduce secondary bleeding episodes?
What should patients be instructed to do to reduce secondary bleeding episodes?
What is a possible cause of nausea after surgery?
What is a possible cause of nausea after surgery?
Why should patients be advised to limit their activities for a minimum of 24 hours?
Why should patients be advised to limit their activities for a minimum of 24 hours?
What should patients be instructed to do to minimize bleeding during the first 24 hours?
What should patients be instructed to do to minimize bleeding during the first 24 hours?
What is the primary reason for the importance of minimizing bone defect in the first molar area during implant surgery?
What is the primary reason for the importance of minimizing bone defect in the first molar area during implant surgery?
What is the result of compromised bone implant contact (BIC) during initial fixation of the implant?
What is the result of compromised bone implant contact (BIC) during initial fixation of the implant?
What is a potential consequence of autoimmune reactions in relation to dental implants?
What is a potential consequence of autoimmune reactions in relation to dental implants?
What is the primary reason for occlusal overloading in the posterior maxilla?
What is the primary reason for occlusal overloading in the posterior maxilla?
What is the consequence of untreated peri-implantitis around a maxillary posterior implant?
What is the consequence of untreated peri-implantitis around a maxillary posterior implant?
What is the primary strategy for preventing displacement and migration of implants into the maxillary sinus?
What is the primary strategy for preventing displacement and migration of implants into the maxillary sinus?
Flashcards are hidden until you start studying
Study Notes
Bleeding Complications
- Arterial hemorrhage: bright red, spurting/pulsatile
- Venous hemorrhage: dark red, continuous
- Capillary hemorrhage: bright red, continuous
- Primary hemorrhage: occurs during surgery, usually due to incision, retraction, or preparation of soft or hard tissue
- Reactionary hemorrhage: occurs within hours after surgery, often in patients with systemic bleeding issues, on anticoagulant therapy, or with postoperative trauma to the surgical area
- Secondary hemorrhage: occurs 7-10 days after surgery, often due to infection
Factors Contributing to Intraoperative Bleeding
- Hypertension
- Medications: anticoagulants, antiplatelet drugs, NSAIDs
- Systemic bleeding disorders: hemophilia, von Willebrand's disease, factor deficiencies
- Liver disorders: liver disease (e.g., cirrhosis, acute liver failure) associated with coagulation system abnormalities
Swallowing/Aspiration of Implant Components
- Etiology: due to small size of abutments, screws, drivers, and other implant components
- Possible outcomes: swallowed into the stomach or aspirated into the lungs
- Prevention: use of floss ligatures, throat packs (4 × 4 gauze), or pharyngeal screens, and high-vacuum function
- Treatment: supportive therapy with heat and analgesics, antibiotic therapy, monitoring for respiratory or cardiac distress
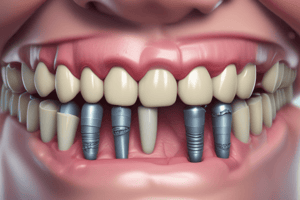
Insufficient Implant–Root Apex Distance
- Etiology: poor treatment planning, poor surgical technique, or placement of too wide of an implant body
- Complications: damage to adjacent periodontal ligament, loss of implant, loss of tooth
- Prevention: maintain at least 1.5 mm distance from adjacent tooth root or tooth structure
Post-Surgical Bleeding
- Patients should be cautioned about bleeding during the first 24 hours
- Recommendations: minimize wearing an interim prosthesis, avoid using a straw, spitting, and vigorous rinsing
- Elevate head, limit activities for a minimum of 24 hours
Nausea After Surgery
- Etiology: prophylactic medications (Augmentin, Clindamycin) or swallowing excessive amounts of blood
- Prevention: unclear, but critical in the first molar area
Late (After Surgery) Migration
- Etiology: negative pressure, autoimmune reaction, occlusal overloading, peri-implantitis
- Prevention: ideal treatment planning, surgical technique, and prevention of displacement and migration of implants into the maxillary sinus
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.