Podcast
Questions and Answers
Which diagnostic imaging technique for nonalcoholic fatty liver disease (NAFLD) has the highest sensitivity?
Which diagnostic imaging technique for nonalcoholic fatty liver disease (NAFLD) has the highest sensitivity?
- Liver biopsy
- MRI (correct)
- Ultrasonography
- CT scan
What is the specificity of ultrasonography when diagnosing NAFLD?
What is the specificity of ultrasonography when diagnosing NAFLD?
- 73%
- 82-100%
- 92%
- 95% (correct)
For patients undergoing a liver biopsy to evaluate for NASH, what is the sensitivity of a single biopsy?
For patients undergoing a liver biopsy to evaluate for NASH, what is the sensitivity of a single biopsy?
- 73% (correct)
- 92%
- 7.7%
- 85%
Which of the following methods provides the lowest positive likelihood ratio (LR+) for advanced fibrosis?
Which of the following methods provides the lowest positive likelihood ratio (LR+) for advanced fibrosis?
In comparing diagnostic techniques for NAFLD, which tool ranks highest in terms of positive likelihood ratio (LR+)?
In comparing diagnostic techniques for NAFLD, which tool ranks highest in terms of positive likelihood ratio (LR+)?
Which parameter is NOT included in the NAFLD Fibrosis Score (NFS)?
Which parameter is NOT included in the NAFLD Fibrosis Score (NFS)?
What is the main purpose of the Fibrosis-4 (FIB-4) Index?
What is the main purpose of the Fibrosis-4 (FIB-4) Index?
Which statement about ultrasound elastography is true?
Which statement about ultrasound elastography is true?
What indicates a likely advanced fibrosis diagnosis according to the FIB-4 Index?
What indicates a likely advanced fibrosis diagnosis according to the FIB-4 Index?
Which of the following is a characteristic of transient elastography?
Which of the following is a characteristic of transient elastography?
Which noninvasive test has the highest sensitivity for predicting the risk of advanced fibrosis?
Which noninvasive test has the highest sensitivity for predicting the risk of advanced fibrosis?
What is the appropriate action when noninvasive tests yield an indeterminate result regarding fibrosis risk?
What is the appropriate action when noninvasive tests yield an indeterminate result regarding fibrosis risk?
Which scoring system is unlikely to require a liver biopsy in patients with low risk of fibrosis?
Which scoring system is unlikely to require a liver biopsy in patients with low risk of fibrosis?
Which noninvasive method uses the AST/ALT ratio to assess risk of liver fibrosis?
Which noninvasive method uses the AST/ALT ratio to assess risk of liver fibrosis?
When should a liver biopsy be performed according to the clinical guidelines for patients suspected of having NASH?
When should a liver biopsy be performed according to the clinical guidelines for patients suspected of having NASH?
Which noninvasive test has the highest specificity for detecting liver fibrosis?
Which noninvasive test has the highest specificity for detecting liver fibrosis?
Which of the following scoring systems would be incorrectly associated with a low probability of fibrosis?
Which of the following scoring systems would be incorrectly associated with a low probability of fibrosis?
How does the use of noninvasive tests potentially impact the need for liver biopsy in NAFLD patients?
How does the use of noninvasive tests potentially impact the need for liver biopsy in NAFLD patients?
Which physical exam finding has the highest positive likelihood ratio (LR+) associated with Hepatocellular Disease diagnosis?
Which physical exam finding has the highest positive likelihood ratio (LR+) associated with Hepatocellular Disease diagnosis?
Which exam finding has the lowest sensitivity when diagnosing Chronic Liver Disease?
Which exam finding has the lowest sensitivity when diagnosing Chronic Liver Disease?
What is the specificity of palmar erythema in the diagnosis of Hepatocellular Disease?
What is the specificity of palmar erythema in the diagnosis of Hepatocellular Disease?
Which of the following findings has a specificity of 100% associated with Chronic Liver Disease?
Which of the following findings has a specificity of 100% associated with Chronic Liver Disease?
Which physical exam finding is likely to have the highest sensitivity when diagnosing Hepatocellular Disease?
Which physical exam finding is likely to have the highest sensitivity when diagnosing Hepatocellular Disease?
Which risk factor is most closely associated with the development of NAFLD in both obese and non-obese individuals?
Which risk factor is most closely associated with the development of NAFLD in both obese and non-obese individuals?
Which of the following complications is NOT commonly associated with NAFLD?
Which of the following complications is NOT commonly associated with NAFLD?
What is a significant factor in the increased severity of NAFLD among different ethnicities?
What is a significant factor in the increased severity of NAFLD among different ethnicities?
What alternative designation has been proposed for NAFLD that captures its metabolic aspects?
What alternative designation has been proposed for NAFLD that captures its metabolic aspects?
When should patients with NAFLD be referred to a specialist?
When should patients with NAFLD be referred to a specialist?
Which diagnostic criteria is essential for evaluating the progression of NAFLD?
Which diagnostic criteria is essential for evaluating the progression of NAFLD?
What is the primary purpose of patient education in the context of NAFLD management?
What is the primary purpose of patient education in the context of NAFLD management?
What role does physical activity play in the context of NAFLD development?
What role does physical activity play in the context of NAFLD development?
Which of the following criteria is NOT part of the diagnosis for metabolic syndrome?
Which of the following criteria is NOT part of the diagnosis for metabolic syndrome?
What is the new terminology for NAFLD that reflects its strong association with metabolic syndrome?
What is the new terminology for NAFLD that reflects its strong association with metabolic syndrome?
Which of the following is NOT considered a maternal protective factor for reducing NAFLD risk?
Which of the following is NOT considered a maternal protective factor for reducing NAFLD risk?
Which of the following exposures is associated with increased risk for NAFLD?
Which of the following exposures is associated with increased risk for NAFLD?
Which genetic factor is NOT associated with NAFLD according to the content provided?
Which genetic factor is NOT associated with NAFLD according to the content provided?
Which of the following conditions is NOT associated with NAFLD?
Which of the following conditions is NOT associated with NAFLD?
What is one of the recognized protective factors against the development of NAFLD?
What is one of the recognized protective factors against the development of NAFLD?
Which dietary factor is linked to an increased risk of developing NAFLD?
Which dietary factor is linked to an increased risk of developing NAFLD?
What is the strongest predictor of the progression of nonalcoholic fatty liver disease (NAFLD)?
What is the strongest predictor of the progression of nonalcoholic fatty liver disease (NAFLD)?
When steatosis is the only finding on a liver biopsy, how is the disease characterized?
When steatosis is the only finding on a liver biopsy, how is the disease characterized?
Which complication is NOT associated with nonalcoholic fatty liver disease (NAFLD)?
Which complication is NOT associated with nonalcoholic fatty liver disease (NAFLD)?
What percentage of patients with nonalcoholic steatohepatitis (NASH) may progress to cirrhosis?
What percentage of patients with nonalcoholic steatohepatitis (NASH) may progress to cirrhosis?
Which of the following factors contributes to an increased mortality risk in patients with end-stage liver cirrhosis and hepatocellular carcinoma?
Which of the following factors contributes to an increased mortality risk in patients with end-stage liver cirrhosis and hepatocellular carcinoma?
Which of the following statements accurately describes the natural history of nonalcoholic fatty liver disease?
Which of the following statements accurately describes the natural history of nonalcoholic fatty liver disease?
What is the relationship between NAFLD and type 2 diabetes mellitus?
What is the relationship between NAFLD and type 2 diabetes mellitus?
What is the estimated annual risk of developing hepatocellular carcinoma in patients with NAFLD?
What is the estimated annual risk of developing hepatocellular carcinoma in patients with NAFLD?
What is a key lifestyle modification recommended for individuals with Non-Alcoholic Fatty Liver Disease (NAFLD)?
What is a key lifestyle modification recommended for individuals with Non-Alcoholic Fatty Liver Disease (NAFLD)?
Which of the following should be monitored every six months for patients with NASH who have advanced cirrhosis?
Which of the following should be monitored every six months for patients with NASH who have advanced cirrhosis?
What initial laboratory test is crucial in assessing a patient suspected of having NAFLD?
What initial laboratory test is crucial in assessing a patient suspected of having NAFLD?
What is the primary intervention for managing comorbid conditions in patients with NAFLD?
What is the primary intervention for managing comorbid conditions in patients with NAFLD?
How often should patients with NASH be followed by specialists to manage their condition?
How often should patients with NASH be followed by specialists to manage their condition?
In the context of suspected NAFLD, which factor is NOT commonly reviewed during the patient history assessment?
In the context of suspected NAFLD, which factor is NOT commonly reviewed during the patient history assessment?
Which of the following interventions is typically discouraged in the management of patients with NASH?
Which of the following interventions is typically discouraged in the management of patients with NASH?
What is the significance of calculating BMI and waist circumference during the assessment of NAFLD?
What is the significance of calculating BMI and waist circumference during the assessment of NAFLD?
What should be considered if liver function tests are chronically elevated or the family history is positive for cirrhosis in a suspected NAFLD case?
What should be considered if liver function tests are chronically elevated or the family history is positive for cirrhosis in a suspected NAFLD case?
What potential outcome could arise from failure to manage NAFLD appropriately?
What potential outcome could arise from failure to manage NAFLD appropriately?
Flashcards are hidden until you start studying
Study Notes
Noninvasive Testing for Liver Fibrosis
- Noninvasive tests for fibrosis can help identify patients at higher risk for developing advanced fibrosis.
- These can reduce the need for liver biopsies.
- Some tests include: AST/ALT ratio, AST/platelet count ratio index (APRI), BARD score, Enhanced liver fibrosis (ELF) panel, Fibrosis-4 (FIB-4) index, FibroTest (FibroSure), Fibrometer, Magnetic resonance elastography, Nonalcoholic fatty liver disease fibrosis score (NFS), and Ultrasound elastography.
Comparing Diagnostic Accuracy
- Noninvasive test accuracy varies between tests.
- The best performing noninvasive tests include the ELF panel, Fibrometer, and Magnetic resonance elastography.
- Ultrasound, CT, and MRI have similar diagnostic accuracy for NAFLD.
- Liver biopsy is the gold standard but has limitations in terms of sensitivity and specificity.
NAFLD Fibrosis Score (NFS)
- Helps estimate scarring in the liver.
- Score based on age, BMI, impaired fasting glucose or diabetes, AST, ALT, platelet count, and albumin.
- High score (> 0.676) increases the likelihood of advanced fibrosis.
Fibrosis-4 (FIB-4) Index
- Used in patients with liver disease to measure fibrosis and need for a biopsy.
- Score based on age, AST, ALT, and platelet count.
- High score (> 3.25) suggests advanced fibrosis, and a low score (< 1.45) suggests low risk of advanced fibrosis.
Ultrasound Elastography
- Measures liver stiffness, indicative of fibrosis stage.
- Uses ultrasound waves passing through the liver.
- Several types include transient elastography (FibroScan), point shear wave elastography, and two-dimensional shear wave elastography.
- Cut-off values for fibrosis stages vary based on the technique and equipment manufacturer.
NAFLD Definition
- Non-alcoholic fatty liver disease (NAFLD) is a prevalent liver condition characterized by excessive fat accumulation in the liver.
- NAFLD is considered the liver manifestation of metabolic syndrome.
- New terminology for NAFLD: Metabolic-associated (or metabolic dysfunction-associated) fatty liver disease (MAFLD).
NAFLD: Risk Factors and Causes
- Maternal risk factors:
- Maternal obesity
- High maternal early-pregnancy glucose concentrations
- Maternal protective factors:
- Breastfeeding for more than 6 months (avoidance of early supplemental milk formula)
- Reduces NAFLD risk in offspring and in mother
- Exposures:
- Drugs (corticosteroids, amiodarone, diltiazem, methotrexate, tamoxifen, irinotecan, oxaliplatin, antiretroviral therapy)
- Toxins (vinyl chloride, carbon tetrachloride, yellow phosphorus, inorganic arsenic exposure)
- Dietary and nutritional factors:
- Excessive dietary fructose consumption
- Malnutrition
- Starvation and refeeding syndrome
- Total parenteral nutrition
- Genetic factors:
- Polymorphisms of genes encoding:
- Apolipoprotein C3
- Patatin-like phospholipase domain-containing 3 (PNPLA3)
- TM6SF2
- HSD17B13
- MBOAT1
- GCKR
- Polymorphisms of genes encoding:
- Associated conditions:
- Cushing syndrome
- Hypopituitarism
- Polycystic ovarian syndrome
- Hypothyroidism
- Hypobetalipoproteinemia (low apolipoprotein B and LDL cholesterol)
- Obstructive sleep apnea
- Gut dysbiosis
- Altered bile acid metabolism
- Cholecystectomy
- Psoriasis
NAFLD: Protective Factors
- Physical activity protects against the development of NAFLD.
- May be due to improved insulin sensitivity, reduced inflammation, and increased energy expenditure.
NAFLD: Timing and Clinical Course
- NAFLD is a slowly progressive disease, often silent when only steatosis is present.
- Early stages (simple steatosis or NAFL) are reversible.
- Progression:
- NAFL --> 20% develop NASH --> 20% progress to cirrhosis --> possible liver failure and liver cancer.
- Key risk factors for advanced hepatic fibrosis and cirrhosis:
- Advanced age
- Obesity
- Diabetes mellitus
- Strongest predictor of progression is the degree of inflammation on the first liver biopsy.
NAFLD Complications
- Cardiovascular disease:
- Increased risk for heart attack, stroke, and other cardiovascular events.
- Hepatocellular carcinoma:
- Annual risk of 1-2% in NAFLD patients.
- End-stage liver disease and liver failure:
- Develops over 10 years in 45% of patients with NASH.
- Other Complications:
- Chronic kidney disease
- Colorectal cancers
- Type 2 diabetes mellitus
NAFLD: Management and Patient Education
-
Interprofessional approach is crucial:
- Encourage lifestyle changes and manage comorbid conditions.
- Key interventions:
- Weight loss
- Dietary fructose restriction
- Increased dietary fiber
- Moderate exercise
- Alcohol abstinence
- Discontinuation of hepatotoxic drugs
- Optimal treatment of diabetes and hyperlipidemia
-
NASH patients require specialist follow-up:
- Hepatologists or gastroenterologists.
-
Liver transplantation may be necessary in advanced cases:
- NAFLD is the second most common reason for liver transplantation in North America.
-
Surveillance for hepatocellular carcinoma is vital:
- Liver ultrasound every six months for NASH patients with cirrhosis.
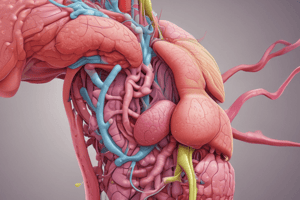
NAFLD: Diagnosis and Assessment
- Assess for likelihood of NAFLD:
- Thorough history taking, including alcohol intake, medication review, and family history.
- Physical exam:
- Calculate BMI and measure waist circumference.
- Laboratory tests:
- Liver function testing (ALT, AST)
- Fasting glucose or HbA1C
- Lipid profile
- Ferritin and iron/TIBC
- Hepatitis B surface antigen (HBsAg) and hepatitis C virus antibody (anti-HCV) testing
- Additional testing if indicated:
- Antinuclear antibody and smooth muscle antibody testing
- Alpha1-antitrypsin and ceruloplasmin levels
- Imaging:
- Liver ultrasonography
- Liver biopsy:
- May be required for definitive diagnosis and staging.
When to Refer a Patient with NAFLD
- Patients with NASH should be referred to a specialist.
- Consider referral if:
- Elevated liver enzymes (AST, ALT), especially if chronically.
- Family history of cirrhosis
- Evidence of liver fibrosis or cirrhosis based on imaging or clinical findings.
- Suspicion of other liver disorders.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.