Podcast
Questions and Answers
How can cerebrospinal fluid rhinorrhea be quickly diagnosed?
How can cerebrospinal fluid rhinorrhea be quickly diagnosed?
- Using a towel instead of a handkerchief
- By checking the drying pattern of the fluid on a handkerchief (correct)
- Through an MRI examination
- By observing the color of the fluid
What type of fracture requires a neurosurgical consultation for proper diagnosis?
What type of fracture requires a neurosurgical consultation for proper diagnosis?
- Fracture of the mandibular condyle
- Fracture in the middle cranial fossa (correct)
- Fracture of the nasal bones
- Fracture of the zygomatic arch
Which neurological sign indicates possible neurological trauma?
Which neurological sign indicates possible neurological trauma?
- Stable pupils
- Positive Babinski reflex (correct)
- Normal reflexes
- Mild headache
When is movement of the maxilla considered dangerous in the presence of cerebrospinal rhinorrhea?
When is movement of the maxilla considered dangerous in the presence of cerebrospinal rhinorrhea?
What should be done if there is doubt regarding the presence of cerebrospinal fluid in collected material?
What should be done if there is doubt regarding the presence of cerebrospinal fluid in collected material?
Why is it dangerous to perform maxillary fracture reduction when cerebrospinal rhinorrhea is present?
Why is it dangerous to perform maxillary fracture reduction when cerebrospinal rhinorrhea is present?
Which of the following is a common procedure before confirming a fracture through radiographic examination?
Which of the following is a common procedure before confirming a fracture through radiographic examination?
What is the role of the neurologist in managing a patient with a suspected cranial fracture?
What is the role of the neurologist in managing a patient with a suspected cranial fracture?
What is a crucial consideration in jaw fractures that distinguishes them from fractures in other body parts?
What is a crucial consideration in jaw fractures that distinguishes them from fractures in other body parts?
Which of the following is a disadvantage of open reduction in the treatment of fractures?
Which of the following is a disadvantage of open reduction in the treatment of fractures?
What is often used to guide the reduction in jaw fractures during treatment?
What is often used to guide the reduction in jaw fractures during treatment?
Which method of fixation is frequently the first step in managing jaw fractures?
Which method of fixation is frequently the first step in managing jaw fractures?
What technique is used when intermaxillary fixation is insufficient for jaw fractures?
What technique is used when intermaxillary fixation is insufficient for jaw fractures?
Which fixation method has been largely abandoned for managing angle fractures?
Which fixation method has been largely abandoned for managing angle fractures?
In what situation is fixation by medullary pins most commonly utilized?
In what situation is fixation by medullary pins most commonly utilized?
What is a common risk associated with open reduction surgical procedures?
What is a common risk associated with open reduction surgical procedures?
What factor significantly contributes to the reduced incidence of jaw fractures in boxers?
What factor significantly contributes to the reduced incidence of jaw fractures in boxers?
Which region of the mandible has the highest reported incidence of fractures?
Which region of the mandible has the highest reported incidence of fractures?
What primary muscle is responsible for displacing the posterior jaw fragment upward during a fracture?
What primary muscle is responsible for displacing the posterior jaw fragment upward during a fracture?
What primarily causes the displacement of mandibular fracture fragments?
What primarily causes the displacement of mandibular fracture fragments?
Why are symphysis fractures particularly difficult to fixate?
Why are symphysis fractures particularly difficult to fixate?
Which muscle primarily contributes to the medial displacement of the posterior fragment in a mandible fracture?
Which muscle primarily contributes to the medial displacement of the posterior fragment in a mandible fracture?
In cases of condylar fracture, what is the typical direction of displacement for the condyle?
In cases of condylar fracture, what is the typical direction of displacement for the condyle?
Which region experiences the lowest incidence of fractures within the mandible?
Which region experiences the lowest incidence of fractures within the mandible?
What is an important indicator of a recently acquired bony deformity in mandibular fractures?
What is an important indicator of a recently acquired bony deformity in mandibular fractures?
Which sign is considered pathognomonic of a mandibular fracture?
Which sign is considered pathognomonic of a mandibular fracture?
What symptom is frequently associated with fractures through the angle or ramus region of the mandible?
What symptom is frequently associated with fractures through the angle or ramus region of the mandible?
In which situation is reduction and fixation typically not performed together?
In which situation is reduction and fixation typically not performed together?
What is a common effect of injury to the inferior alveolar nerve during a mandibular fracture?
What is a common effect of injury to the inferior alveolar nerve during a mandibular fracture?
What is the primary goal of the apparatus used in the treatment of a simple mandibular fracture?
What is the primary goal of the apparatus used in the treatment of a simple mandibular fracture?
Which of the following is a significant symptom when condylar movements are restricted?
Which of the following is a significant symptom when condylar movements are restricted?
What treatment strategy is often employed for simple mandibular fractures?
What treatment strategy is often employed for simple mandibular fractures?
What is a primary concern when skeletal pin fixation is performed by an inexperienced person?
What is a primary concern when skeletal pin fixation is performed by an inexperienced person?
What is one of the advantages of using internal wiring compared to a plaster headcap for maxillary fractures?
What is one of the advantages of using internal wiring compared to a plaster headcap for maxillary fractures?
What was one of the complications associated with open operations on bones before World War II?
What was one of the complications associated with open operations on bones before World War II?
Why was there a trend away from using gadgets like bicycle spokes for treating complicated jaw fractures after World War II?
Why was there a trend away from using gadgets like bicycle spokes for treating complicated jaw fractures after World War II?
What has contributed to the popularity of open reduction procedures since World War II?
What has contributed to the popularity of open reduction procedures since World War II?
What is a potential drawback of open reduction procedures mentioned in the content?
What is a potential drawback of open reduction procedures mentioned in the content?
How were maxillary fractures traditionally maintained before the introduction of internal wiring?
How were maxillary fractures traditionally maintained before the introduction of internal wiring?
In skeletal pin fixation, how long and what diameter is the screw pin typically described?
In skeletal pin fixation, how long and what diameter is the screw pin typically described?
Study Notes
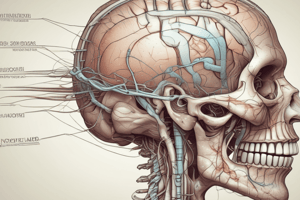
Cranial Fracture
- Neurosurgical consultation is necessary to differentiate a middle cranial fossa fracture, a fracture of the mandibular condyle, and a primary wound in the external auditory canal.
- Patients diagnosed with a cranial fracture should be treated by a neurologist or neurosurgeon.
- Treatment for other wounds or fractures should only be initiated when the patient is considered out of danger, potentially a week or two later.
Cerebrospinal Rhinorrhea
- A fractured cribriform plate of the ethmoid bone in a complicated maxillary fracture can result in cerebrospinal fluid leaking from the nostrils.
- A handkerchief placed under the nose can identify cerebrospinal fluid due to its lack of starching when dried, compared to mucus.
- A glucose test can confirm the presence of cerebrospinal fluid.
- Movement of the maxilla in cases of cerebrospinal rhinorrhea is dangerous due to the risk of infection.
- Antibiotics now allow for earlier maxillary fracture reduction, minimizing potentially dangerous delayed healing.
Neurological Signs and Symptoms
- Neurological consultation is recommended if signs of neurological trauma are present, including lethargy, severe headache, vomiting, positive Babinski reflex, and dilated pupils.
- Radiographic examination is performed if a fracture is suspected, including posteroanterior jaw and right and left lateral oblique jaw images.
Open Reduction
- Open reduction offers the advantage of cleaning out debris between bone ends that could impede healing.
- Open reduction disadvantages include the removal of the protective clot, risk of infection, increased hospital time, and scarring.
Fixation
- Jaw fractures are typically fixed using wires, arch bars, or splints, allowing for the use of intermaxillary traction to aid reduction.
- Open reduction and direct bone wiring are used only when additional fixation is required.
- Medullary pins are sometimes used for mandibular symphysis fractures and rarely for mandibular angle fractures.
- Skeletal pin fixation is a common method, consisting of screws driven through the bone and connected by a metal rod.
- Maxillary fractures are often fixed using a plaster headcap or internal wiring.
- Internal wiring can be suspended over the zygomatic arches or through holes drilled into unfractured bone.
- Internal wiring allows for less visible fixation and movement during healing compared to a plaster headcap.
- Open reduction was favored in the years after World War II due to the advancements in antibiotics and metals tolerated by tissues.
- The use of open reduction is declining due to the risk of resistant infections and the lack of significantly better results.
- Increased calcification in athletes can reduce the risk of jaw fractures due to increased bone density and protective gear.
Mandibular Fracture Locations
- The most common mandibular fracture locations are the angle (31%), condyle (18%), and molar region (15%).
- The most frequent bilateral fracture is in the angle-mental regions.
Displacement
- Muscle pull plays a significant role in mandibular fracture displacement, creating an imbalance of forces when the bone is fractured.
- The masseter and medial pterygoid muscles displace the posterior fragment upward.
- The suprahyoid muscles displace the anterior fragment downward.
- The medial pterygoid muscle displaces the posterior fragment medially.
- The mylohyoid muscle can displace fragments in the anterior portion of the jaw medially.
- The superior constrictor of the pharynx also contributes to medial pull.
- Difficulty in fixing symphysis fractures results from the bilateral posterior and lateral pull of the suprahyoid and digastric muscles.
Signs and Symptoms
- A history of injury is a common indicator.
- Occlusion provides insight into recent bony deformity.
- Abnormal mobility with palpation of the mandible is a reliable sign.
- Pain with mandibular movement or face palpation is a common symptom.
- Crepitus during manipulation or mandibular function is pathognomonic of a fracture.
- Disability is characterized by difficulty in mastication due to pain or abnormal mobility.
- Trismus, or reflex spasm, is frequently observed in angle or ramus fractures.
- Laceration of the gingiva may occur in the region of the fracture.
- Anesthesia in the gingiva and lip can occur due to inferior alveolar nerve injury.
- Ecchymosis in the gingiva or mucosa can indicate a fracture site.
- Excessive salivation and foul breath may also be present.
Treatment
- Simple mandibular fractures typically involve simultaneous reduction and fixation.
- Intermaxillary fixation using wires, arch bars, or splints is the initial step for fixation.
- Intermaxillary traction and tooth occlusion aid in reducing the fracture.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on cranial fractures and cerebrospinal rhinorrhea. This quiz covers essential details regarding diagnosis, treatment protocols, and complications associated with these conditions. Ideal for medical students and professionals in the neurosurgery field.