Podcast
Questions and Answers
What is a characteristic feature of disorders affecting the neuromuscular junction?
What is a characteristic feature of disorders affecting the neuromuscular junction?
- Muscle weakness with normal muscle bulk (correct)
- Impaired sensory function
- Loss of deep tendon reflexes
- Increased muscle tone and rigidity
Which of the following symptoms is typically NOT associated with peripheral nerve disorders?
Which of the following symptoms is typically NOT associated with peripheral nerve disorders?
- Numbness and tingling in extremities
- Involuntary muscle contractions
- Vision changes (correct)
- Muscle wasting
In the context of central nervous system disorders, which condition is characterized by progressive muscle weakness?
In the context of central nervous system disorders, which condition is characterized by progressive muscle weakness?
- Myasthenia gravis
- Amyotrophic lateral sclerosis (ALS) (correct)
- Multiple sclerosis
- Guillain-Barré syndrome
Which of the following statements about myasthenia gravis is true?
Which of the following statements about myasthenia gravis is true?
What underlying mechanism is often involved in disorders of the neuromuscular junction?
What underlying mechanism is often involved in disorders of the neuromuscular junction?
Flashcards
Nervous system disorders
Nervous system disorders
Conditions affecting the brain, spinal cord, nerves, and muscles.
Central nervous system
Central nervous system
The brain and spinal cord.
Peripheral nervous system
Peripheral nervous system
Nerves branching out from the central nervous system, connecting to the rest of the body.
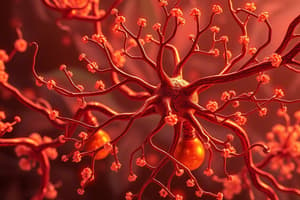
Neuromuscular junctions
Neuromuscular junctions
Signup and view all the flashcards
Nursing 302
Nursing 302
Signup and view all the flashcards
Study Notes
Disorders of the Central and Peripheral and Neuromuscular Junctions
- This is a topic in Nursing 302.
Traumatic Brain Injury (TBI)
- TBI is an alteration in brain function caused by external force (e.g., motor vehicle accidents, falls).
- Primary injury: direct impact (focal or diffuse).
- Secondary injury: indirect result of the primary injury.
- Most common injury location: frontal lobe.
- Focal brain injury (observable injury): lesion or contusion.
- Open (penetrating) trauma: breaks the dura, exposing cranial contents to the environment.
- Closed (blunt) trauma: dura remains intact, brain tissues not exposed.
- Coup injury: injury directly below the impact point.
- Contrecoup injury: injury on the opposite side of impact.
- Contusions can cause epidural, subdural, or intracerebral hematomas.
- Diagnosis: history, Glasgow Coma Scale (GCS) score, CT/MRI/PET scan, EEG, intracranial pressure (ICP).
- Treatment goal: control ICP and manage symptoms; potential surgery.
Hematomas
- Epidural: bleeding between the dura mater and the skull (typically caused by an artery); usually involves loss of consciousness at the time of initial injury; medical emergency.
- Symptoms: worsening headache, vomiting, drowsiness, confusion, seizures, and hemiparesis (weakness on one side of the body).
- Diagnosis: CT, MRI.
- Treatment: monitoring and evaluation, pain management, potential surgery.
- Subdural: bleeding between the dura mater and brain; acts like growing masses, increasing ICP; can cause pressure on blood vessels.
- Symptoms: headache, drowsiness, restlessness/agitation, slowed thought, confusion, loss of consciousness, breathing pattern changes, pupil changes.
- Diagnosis: CT, MRI.
- Treatment: percutaneous drainage or craniotomy (for chronic bleeds).
- Intracerebral: bleeding within the brain; increases ICP, decreased level of consciousness (LOC).
- Treatment: decreasing ICP and allowing the hematoma to reabsorb slowly.
Open Brain Injury
- Trauma that penetrates the dura mater.
- Compound skull fracture: opens a path between cranial contents and the environment.
- Basilar skull fracture: fracture to the base of the skull.
- Symptoms: CSF leaking from ears or nose, Battle's sign, periorbital hematoma (raccoon eyes).
- Treatment: bed rest and close observation for meningitis and other complications.
Diffuse Axonal Injury (DAI)
- Widespread brain injury, severity corresponds to the amount of shearing force.
- Causes: high levels of acceleration/deceleration or rotational forces (e.g., whiplash).
- Results in:
- Axonal damage (shearing, tearing, or stretching of nerve fibers).
- Acute brain swelling.
- Potential long-term neurodegenerative processes.
Concussion
- Interchangeable term for TBI.
- Severity considers duration of loss of consciousness, GCS score, post-traumatic amnesia, and brain imaging results.
- Goal of treatment: maintain cerebral perfusion & oxygenation and promote neuroprotection.
- Mild: no loss of consciousness or loss of consciousness for less than 30 minutes; GCS 13-15; confusion lasts for 1-several minutes; possible retrograde amnesia; symptoms: headache, nausea, vomiting, impaired ability to concentrate, difficulty sleeping.
- Moderate: any loss of consciousness lasting 30 minutes to 6 hours; GCS 9-12; confusion and post-traumatic amnesia lasting for more than 24 hours; symptoms: deficits in selective attention, vigilance, working memory, data processing, vision or perception, and language; mood and affect changes (mild to severe).
- Severe: loss of consciousness lasting more than 6 hours; GCS 3-8; associated with signs of brainstem damage; symptoms: changes in pupils, posturing, reflexes, cardiac and respiratory systems; increased ICP; communication and coordination problems.
- Diagnosis: usually includes blood tests to assess if a CT scan is needed.
Complications of TBI
- Post-concussion syndrome: lasts for weeks to months after concussion; symptoms include headache, fatigue, anxiety, irritability, insomnia, inability to concentrate, and forgetfulness.
- Post-traumatic seizures: can occur within days or up to 2-5 years post-injury; hyperexcitable state.
- Chronic traumatic encephalopathy: progressive dementing disease, often associated with repeated brain injury (sports injuries, blast trauma, work-related head trauma).
- Symptoms are violent behaviors, loss of control, depression, memory loss, and cognitive changes, changes in motor function.
Spinal Cord Injury
- Causes: MVA, sports, violence, falls (especially in individuals over 70 years old).
- Risk Factors: male, ages 20-39.
- Primary spinal cord injury: initial mechanical trauma and immediate tissue destruction.
- Secondary spinal cord injury: pathophysiological cascade of events following initial injury (edema, ischemia, excitotoxicity, inflammation, cell death.
- Vertebral injuries: result from acceleration, deceleration, or deformation forces during impact (fractures, dislocations, bone fragments causing compression).
Clinical Manifestations of Spinal Cord Injury
- Spinal shock: normal activity of the spinal cord ceases at and below the level of injury; sites lack continuous nervous discharges from the brain; complete loss of reflex function (skeletal, bladder, bowel, thermal control, and autonomic control) below the level of lesion.
- Neurogenic shock: occurs with injury above T6; caused by absence of sympathetic activity; symptoms include vasodilation, hypotension, bradycardia, and failure of temperature regulation.
- Autonomic hyperreflexia (dysreflexia): massive, uncompensated cardiovascular response to stimulation of the sympathetic nervous system; sudden HTN (up to 300 mm Hg systolic), pounding headache, blurred vision, sweating, bradycardia; usually triggered by distended bladder or rectum.
Diagnosis and Treatment of Spinal cord injury
- Diagnosis: physical exam and imaging studies.
- Treatment: immediate immobilization; surgical fixation and decompression (may be necessary); therapeutic hypothermia; nutrition; lung function; skin integrity; bladder and bowel management; rehabilitation.
Stroke
- Result of cerebrovascular disease; interruption in blood flow to brain cells.
- Third leading cause of death in Canada.
- The sooner circulation returns, the better chances for complete recovery.
- Risk Factors: poorly controlled hypertension, polycythemia/thrombocythemia, hyperlipidemia, congestive heart failure (CHF)/peripheral vascular disease (PVD), atherosclerosis, arrhythmias (Atrial Fibrillation), diabetes, lack of exercise, hormonal contraceptive use, smoking, family history.
- Classification: Ischemic (thrombotic or embolic), Hemorrhagic, Transient Ischemic Attacks (TIA).
Transient Ischemic Attacks (TIAs)
- Brief interruption in blood supply to the brain; recurrent episode of neurological dysfunction (no more than 1 hour); resolves within 12-24 hours.
- Warning sign of an impending thrombotic stroke.
- Clinical manifestations can include double vision/unilateral blindness, staggering/uncoordinated gait, weakness/numbness on one side, dizziness, slurred speech, and sudden confusion.
- Treatment: preventing a thrombotic stroke - aspirin (antiplatelet) and/or anticoagulants.
Ischemic Stroke
- Thrombotic: arterial occlusions (blockages) caused by thrombi formed in arteries that supply blood to the brain/intracranial vessels; most often from atherosclerosis; causes congestion and edema in the affected vessel and ischemia in the affected brain tissue.
- Embolic: embolus breaks off from a thrombus outside the brain (heart, aorta, carotid artery), cuts off circulation, causing necrosis and edema; septic embolus may lead to encephalitis.
Pathophysiology and Treatment of Ischemic Stroke
- Pathophysiology: cerebral infarction results when an area of the brain loses blood supply due to vascular blockage; prompt infusion of thrombolytic agents may restore perfusion and prevent necrosis. The infusion should occur within 4 hours of the stroke onset.
- Diagnosis: cerebral angiography, CT, MRI.
- Treatment: restoring brain perfusion (e.g.tPA); preventing recurrent ischemic events (anticoagulants); physical rehabilitation to help patient adapt to deficits (hemiparesis, speech impairments); surgery (if needed), depending on the extent of the stroke.
Hemorrhagic Stroke
- Sudden rupture of a cerebral artery, leading to diminished blood supply to the area served by that artery.
- Risk Factors: hypertension, aneurysms, cocaine use, trauma.
- Pathophysiology: blood accumulates within the brain, causing greater damage (potential increased ICP). The event eventually resolves on its own through reabsorption.
- Diagnosis: cerebral angiography, CT, MRI.
- Treatment: stop or reduce the bleed; control blood pressure; surgery (if needed), depending on the extent of damage.
Migraines
-
Familial, episodic disorder; recurrent, episodic headaches lasting 4-72 hours; most common in women 25-55 years old.
-
Triggers: altered sleep patterns, overexertion, weather changes, stress/relaxation, hormonal changes (menstrual periods), excess afferent stimulation (bright lights, strong smells), chemicals (alcohol, nitrates).
-
Phases: premonitory, migraine aura (visual, sensory, or motor), headache, recovery.
-
Diagnosis: medical history of headaches; symptoms may include unilateral throbbing pain, worse with movement, moderate to severe pain, nausea/vomiting, photophobia/phonophobia.
-
Treatment: avoid triggers, pharmacological management.
Cluster Headaches
- Occur in clusters of days, followed by a long period of spontaneous remission.
- Usually affect men between 20 and 50 years old.
- Trigeminal activation and autonomic dysfunction; unilateral pain and associated autonomic manifestations, such as tearing, rhinorrhea, and ptosis on the affected side.
Meningitis
- Inflammation of the meninges in the brain and spinal cord; reduced blood flow to the brain; tissue swelling causing increased intracranial pressure (ICP).
- Spread through droplets (bacterial infections); quick spread due to CSF circulation.
- Causes: bacteria, viruses, fungi, parasites, and toxins.
- Risk Factors: malnutrition, immunosuppression, CNS trauma.
Meningitis (Clinical Manifestations)
- In Children <2 years old: Fever, anorexia/refusal to eat, vomiting/diarrhea, listlessness, pale appearance, disinterested, bulging fontanels, cry.
- In children and young adults: fever/chills, headache, photophobia, nuchal rigidity (neck stiffness), positive Kernig's & Brudzinski signs, tachycardia, ICP deterioration, generalized convulsions, increased ICP, cranial nerve dysfunction, projectile vomiting.
- Nursing Assessment: nutrition, fluid/electrolyte imbalances, transmission.
Meningitis (Diagnosis & Treatment)
- Diagnosis: history, positive Brudzinski's/Kernig signs, lumbar puncture (LP) with evaluation of cloudy or milky cerebrospinal fluid (CSF), high protein level, low glucose level, presence or absence of an organism detected via Gram stain/culture, CT, MRI, EEG, chest x-ray, white blood cell count (WBC), blood culture.
- Treatment: intravenous (IV) antibiotics, bed rest, management of fever, fluid therapy, isolating infected to prevent spread.
Brain or Spinal Cord Abscess
- Localized collection of pus in the brain or spinal cord parenchyma. Brain abscess: epidural, subdural, or intracerebral. Spinal cord abscess: rare; epidural (often begins with osteomyelitis in a vertebra) or intramedullary (in the spinal cord).
- Risk factors: immunosuppression, IV drug users.
- Pathophysiology: microorganisms entering the CNS, frequently by direct extension along the wall of a vein; infectious emboli may occur and carry organisms from other locations.
- Symptoms (and stage):
- Early: low-grade fever, headache, nausea/vomiting, neck pain/stiffness, confusion/drowsiness, sensory deficits, and communication deficits.
- Later: decreased attention span, memory deficits, decreased visual acuity and narrowed visual fields, papilledema, ocular palsy, ataxia, seizures, and dementia
- Diagnosis: imaging studies.
- Treatment: antibiotics, surgical aspiration/excision, ICP management, and supportive care.
Encephalitis
- Acute febrile illness, usually viral; nervous system involvement.
- Causes: mosquito, tick, or fly bites, herpes simplex type 1, live attenuated vaccines (MMR or varicella).
- Clinical manifestations:
- Mild: malaise, headache, body aches, nausea/vomiting.
- Severe: fever, delirium, decreased LOC, seizures, paralysis, increasing ICP signs.
- Diagnosis: history, CSF examination and culture, white blood cell (WBC) count, CT or MRI.
- Treatment: specific to the type of virus.
Multiple Sclerosis (MS)
- Progressive, inflammatory demyelination of the white matter of the central nervous system (CNS).
- Acquired autoimmune, loss of myelin disrupts nerve conduction in neurons, leading to the death of neurons and brain atrophy.
- Characterized by exacerbations and remissions.
- Clinical manifestations: vision problems (optic neuritis, paresthesia, initial symptoms!), emotional lability, dysphagia, muscle weakness and spasticity (potential paralysis), hyperreflexia, urinary or bowel problems, gait ataxia, and fatigue.
- Diagnosis: history, clinical exam, MRI to detect lesions, CSF analysis shows elevated IgG levels.
- Treatment: prevent exacerbations and preserve neurological functioning; medications (steroids); bed rest/massage, preventing fatigue, bowel/bladder training, and physical therapy.
- Key symptom: initial two symptoms may be vision problems and paresthesia.
Myasthenia Gravis
- Acquired chronic autoimmune disease causing progressive, sporadic weakness and abnormal fatigue of voluntary skeletal muscles.
- An IgG antibody targets acetylcholine receptors in neuromuscular junctions, thus making them insensitive to acetylcholine, blocking neuromuscular transmission.
- Clinical manifestations:
- Weakness and fatigue of muscles; diplopia (double vision), difficulty chewing/swallowing; drooping jaw, bobbing head.
- Potential complications (crises): myasthenia crisis (increased symptoms like respiratory distress, tachycardia, decreased gag reflex, visual changes) or cholinergic crisis (hypotension, bradycardia, diarrhea, abdominal cramping, increased respiratory secretions).
- Diagnosis: Tensilon test (IV injection of a medication to temporarily improve muscle function), electromyography (EMG), nerve conduction studies.
- Treatment: anticholinesterase drugs, steroids, intravenous immunoglobulin (IVIG).
Alterations of Neurological Function in Children
- This is a topic in Chapter 17 but there’s no detail here for these notes.
Defects of Neural Tube Closure
- Spina bifida: failure of neural tube closure; causes: genetics, folic acid deficiency.
- Types:
- Anencephaly: missing skull and brain.
- Encephalocele: herniation of brain and meninges through skull defect.
- Meningocele: sac-like cyst of meninges; lack of nerve tissue defect.
- Myelomeningocele: sac-like cyst with meninges, spinal fluid (CSF) and spinal cord with nerves. (increased risk for infection and neuronal damage).
Encephalopathies
- Encephalopathy: alteration in brain pathology.
- Static encephalopathy: condition caused by a fixed lesion without active or ongoing disease; causes: brain malformations, brain injuries (during gestation/birth), anoxia, trauma, infections, toxins, and metabolic disturbances.
- Cerebral palsy: disorder of movement, muscle tone, and posture; risk factors: prenatal/perinatal cerebral hypoxia, hemorrhage, infection, genetic abnormalities, and/or low birth weight; types: spasticity, dystonia, ataxia, mixed; symptoms include seizures, mild to severe intellectual/visual impairment, communication disorders, respiratory problems, bowel, and bladder problems, along with orthopedic disabilities.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.