Podcast
Questions and Answers
What is the expected movement of the soft palate during an examination?
What is the expected movement of the soft palate during an examination?
- It should move downwards.
- It may shift to one side.
- It should remain motionless.
- It should move up symmetrically. (correct)
Which cranial nerve is assessed by having the patient shrug their shoulders?
Which cranial nerve is assessed by having the patient shrug their shoulders?
- Cranial Nerve VII
- Cranial Nerve V
- Cranial Nerve XI (correct)
- Cranial Nerve XII
What does a deviation of the tongue indicate during the hypoglossal nerve examination?
What does a deviation of the tongue indicate during the hypoglossal nerve examination?
- Normal functionality of the muscles.
- Strength in the muscle on the opposite side.
- Inflammation in the throat area.
- Weakness or paralysis on the same side. (correct)
Quantitative Sensory Testing (QST) can be specifically beneficial in assessing which of the following conditions?
Quantitative Sensory Testing (QST) can be specifically beneficial in assessing which of the following conditions?
What does the assessment of QST offer insight into?
What does the assessment of QST offer insight into?
What is the primary purpose of a thorough history in patient management?
What is the primary purpose of a thorough history in patient management?
Which of the following statements best describes cranial nerve dysfunction?
Which of the following statements best describes cranial nerve dysfunction?
What type of pain is defined as 'pain caused by a lesion or disease of the somatosensory nervous system'?
What type of pain is defined as 'pain caused by a lesion or disease of the somatosensory nervous system'?
Which of the following best differentiates dysesthesia from paresthesia?
Which of the following best differentiates dysesthesia from paresthesia?
Which aspect is NOT a part of the cranial nerve examination?
Which aspect is NOT a part of the cranial nerve examination?
What is the significance of Quantitative Sensory Testing (QST) in relation to nerve disorders?
What is the significance of Quantitative Sensory Testing (QST) in relation to nerve disorders?
What type of abnormal sensation is described as 'an unpleasant abnormal sensation, whether spontaneous or evoked'?
What type of abnormal sensation is described as 'an unpleasant abnormal sensation, whether spontaneous or evoked'?
Which of the following symptoms would be most indicative of possible cranial nerve dysfunction?
Which of the following symptoms would be most indicative of possible cranial nerve dysfunction?
What defines hyperalgesia?
What defines hyperalgesia?
What are the three modalities carried by cranial nerves?
What are the three modalities carried by cranial nerves?
What condition results from damage to the olfactory nerve?
What condition results from damage to the olfactory nerve?
What is allodynia characterized by?
What is allodynia characterized by?
Which cranial nerve is responsible for the sense of smell?
Which cranial nerve is responsible for the sense of smell?
What is a common cause of temporary anosmia?
What is a common cause of temporary anosmia?
Which of the following is NOT a sensory modality carried by cranial nerves?
Which of the following is NOT a sensory modality carried by cranial nerves?
What is the primary function of branchial motor nerves?
What is the primary function of branchial motor nerves?
Which of the following structures primarily depends on the intact cerebral hemispheres and upper brain stem?
Which of the following structures primarily depends on the intact cerebral hemispheres and upper brain stem?
What does hypoalgesia refer to?
What does hypoalgesia refer to?
What happens to the contralateral pupil when light is shone directly on one pupil with intact sensory and motor pathways?
What happens to the contralateral pupil when light is shone directly on one pupil with intact sensory and motor pathways?
Which condition is characterized by ptosis, mydriasis, and a 'down and out' gaze?
Which condition is characterized by ptosis, mydriasis, and a 'down and out' gaze?
What does the corneal reflex test primarily evaluate?
What does the corneal reflex test primarily evaluate?
Which cranial nerve is responsible for the sensory component of discriminative touch and pain in the face?
Which cranial nerve is responsible for the sensory component of discriminative touch and pain in the face?
In upper motor neuron lesions affecting the facial nerve, which muscle continues to function and why?
In upper motor neuron lesions affecting the facial nerve, which muscle continues to function and why?
What is anisocoria?
What is anisocoria?
Which of the following is indicative of lower motor neuron lesions affecting the facial nerve?
Which of the following is indicative of lower motor neuron lesions affecting the facial nerve?
What is the primary function of cranial nerve VIII?
What is the primary function of cranial nerve VIII?
What is the normal response of pupils during accommodation?
What is the normal response of pupils during accommodation?
In terms of hearing loss, which condition results from an obstruction in the transmission of sound?
In terms of hearing loss, which condition results from an obstruction in the transmission of sound?
What is the most common cause of unilateral facial paralysis?
What is the most common cause of unilateral facial paralysis?
Which feature is NOT associated with classic Ramsay Hunt Syndrome?
Which feature is NOT associated with classic Ramsay Hunt Syndrome?
Which condition is characterized by the triad of miosis, partial ptosis, and loss of hemifacial sweating?
Which condition is characterized by the triad of miosis, partial ptosis, and loss of hemifacial sweating?
What is the average onset age for Trigeminal Neuralgia?
What is the average onset age for Trigeminal Neuralgia?
What is the primary cause of Cavernous Sinus Syndrome?
What is the primary cause of Cavernous Sinus Syndrome?
Which cranial nerve is affected in the paralysis associated with Superior Orbital Fissure Syndrome?
Which cranial nerve is affected in the paralysis associated with Superior Orbital Fissure Syndrome?
Which symptom is typically associated with Trigeminal Neuralgia?
Which symptom is typically associated with Trigeminal Neuralgia?
What condition can lead to bilateral symptoms in Trigeminal Neuralgia?
What condition can lead to bilateral symptoms in Trigeminal Neuralgia?
Which of the following is NOT a common complication associated with local anesthesia?
Which of the following is NOT a common complication associated with local anesthesia?
Which condition is a known cause of unilateral facial pain?
Which condition is a known cause of unilateral facial pain?
Flashcards
Accurate Diagnosis
Accurate Diagnosis
A thorough evaluation involving obtaining a detailed history of the patient's symptoms and complaints, which can help avoid unnecessary investigations and save costs.
Cranial Nerves
Cranial Nerves
The 12 pairs of nerves that originate directly from the brain, responsible for controlling various functions like sensory perception, motor control, and autonomic functions.
Cranial Nerve Exam
Cranial Nerve Exam
A systematic examination of the 12 cranial nerves, assessing their functionality through various tests and observations.
Cranial Nerve Disorders
Cranial Nerve Disorders
Signup and view all the flashcards
Quantitative Sensory Testing (QST)
Quantitative Sensory Testing (QST)
Signup and view all the flashcards
Neuropathic Pain
Neuropathic Pain
Signup and view all the flashcards
Anesthesia
Anesthesia
Signup and view all the flashcards
Paresthesia
Paresthesia
Signup and view all the flashcards
Dysesthesia
Dysesthesia
Signup and view all the flashcards
Allodynia
Allodynia
Signup and view all the flashcards
Hyperalgesia
Hyperalgesia
Signup and view all the flashcards
Hypoalgesia
Hypoalgesia
Signup and view all the flashcards
General Sensory Nerves
General Sensory Nerves
Signup and view all the flashcards
Visceral Sensory Nerves
Visceral Sensory Nerves
Signup and view all the flashcards
Special Sensory Nerves
Special Sensory Nerves
Signup and view all the flashcards
Somatic Motor Nerves
Somatic Motor Nerves
Signup and view all the flashcards
Branchial Motor Nerves
Branchial Motor Nerves
Signup and view all the flashcards
CN II (Optic Nerve)
CN II (Optic Nerve)
Signup and view all the flashcards
CN III (Oculomotor Nerve)
CN III (Oculomotor Nerve)
Signup and view all the flashcards
Accommodation
Accommodation
Signup and view all the flashcards
Ptosis
Ptosis
Signup and view all the flashcards
Anisocoria
Anisocoria
Signup and view all the flashcards
CN V (Trigeminal Nerve) Sensory Component
CN V (Trigeminal Nerve) Sensory Component
Signup and view all the flashcards
CN VII (Facial Nerve)
CN VII (Facial Nerve)
Signup and view all the flashcards
Bell's Palsy
Bell's Palsy
Signup and view all the flashcards
Conductive Hearing Loss
Conductive Hearing Loss
Signup and view all the flashcards
Sensorineural Hearing Loss
Sensorineural Hearing Loss
Signup and view all the flashcards
Soft Palate and Uvula Movement
Soft Palate and Uvula Movement
Signup and view all the flashcards
Gag Reflex
Gag Reflex
Signup and view all the flashcards
Trapezius Muscle
Trapezius Muscle
Signup and view all the flashcards
Trapezius Strength Test
Trapezius Strength Test
Signup and view all the flashcards
Sternocleidomastoid Strength Test
Sternocleidomastoid Strength Test
Signup and view all the flashcards
Ramsay Hunt Syndrome
Ramsay Hunt Syndrome
Signup and view all the flashcards
Trigeminal Neuralgia
Trigeminal Neuralgia
Signup and view all the flashcards
Cavernous Sinus Syndrome
Cavernous Sinus Syndrome
Signup and view all the flashcards
Horner's Syndrome
Horner's Syndrome
Signup and view all the flashcards
Superior Orbital Fissure Syndrome
Superior Orbital Fissure Syndrome
Signup and view all the flashcards
Facial Nerve (CN VII)
Facial Nerve (CN VII)
Signup and view all the flashcards
Trigeminal Nerve (CN V)
Trigeminal Nerve (CN V)
Signup and view all the flashcards
Olfactory Nerve (CN I)
Olfactory Nerve (CN I)
Signup and view all the flashcards
Optic Nerve (CN II)
Optic Nerve (CN II)
Signup and view all the flashcards
Study Notes
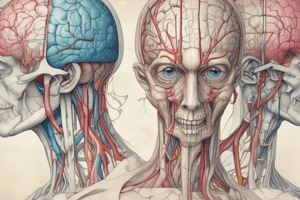
Cranial Nerve Exam
- The presentation covers the examination of the 12 cranial nerves.
- Accurate diagnosis is the most important step in patient management.
- A thorough history is essential, along with observation, recording, and analysis of findings.
- Orofacial pain frequently involves neuropathic disorders, requiring a cranial nerve examination.
- The examination is needed to assess the physiologic and anatomical implications of any dysfunction of the cranial nerves to aid in diagnosis.
- Neuropathic pain is pain from a lesion or disease of the somatosensory nervous system- as defined by the IASP(International Association for the Study of Pain)
- Cranial nerve dysfunction can manifest in motor or sensory changes.
Neurological Screening
- Abnormal muscle movement from cranial nerve stimulation indicates possible motor pathway issues.
- Patients reporting sensory changes can be tested for anesthesia, paresthesia, dysesthesia, allodynia, and hyperalgesia.
- Anesthesia is pain in an area that is insensitive.
- Paresthesia is an abnormal sensation that can be spontaneous or evoked.
- Dysesthesia is an unpleasant abnormal sensation, which should always be unpleasant, should be distinguished from pain and paresthesia.
- Allodynia is pain from a stimulus that does not normally cause it.
- Hyperalgesia is increased pain from a stimulus that normally causes pain.
- Hypoalgesia is a raised threshold for pain reception.
Cranial Nerves
- The human body has 12 pairs of cranial nerves.
- They supply both sensory and motor innervation to the head and neck.
- Six distinct modalities are carried : three sensory and three motor.
- General sensory nerves carry senses like touch, pain, temperature, pressure, and proprioception.
- Visceral sensory nerves handle sensory input from the viscera (internal organs) excluding pain.
- Special sensory nerves carry smell, sight, taste, hearing, and balance.
- Somatic nerves supply voluntary muscle originate from somites.
- Branchial nerves supply voluntary muscle originate from branchial arches
- Parasympathetic nerves supply involuntary smooth muscle.
- This innervation to the cranial muscles enables coordinated movements.
Cranial Nerves - Specific Information
- Olfactory Nerve (CN I): Evaluates the sense of smell and checks nasal passages for patency. Non-irritant stimuli like coffee or chocolate are used.
- Optic Nerve (CN II): Assesses vision (acuity, fields, pupillary light reflex, fundus), involving four procedures: measurement of visual acuity, testing of visual fields, testing of the pupillary light reflex, and visualization of the fundus.
- Oculomotor, Trochlear, and Abducens Nerves (CN III, IV, VI): Eyelid position, pupillary response to light (direct and consensual responses), and extraocular movements are examined.
- Trigeminal nerve (CN V): Sensory components include pain, temperature, and touch on the forehead, cheeks, and jaw; motor components involve strength testing of the masseter and temporalis muscles.
- Facial Nerve (CN VII): Evaluates movements of facial muscles. In the examination, one checks raising the eyebrows, frowning, tightly closing the eyes, smiling, showing teeth, and puffing out cheeks.
- Vestibulocochlear Nerve (CN VIII): Assesses balance (walking heel-to-toe along a straight line) and hearing (using the Weber and Rinne tests).
- Glossopharyngeal and Vagus Nerves (CN IX, X): Examines voice for hoarseness; oropharyngeal examination and gag reflex are performed.
- Spinal Accessory Nerve (CN XI): Evaluates trapezius and sternocleidomastoid muscle strength, checking for atrophy, symmetry, and fasciculation.
- Hypoglossal Nerve (CN XII): Checks tongue movement and protrusion, noting deviation.
Cranial Nerve Examination Techniques
- The presentation provides detailed descriptions for testing each cranial nerve.
- Specific examples of how to assess cranial nerve function are illustrated through diagrams and demonstrations.
- Videos are provided for further study on cranial nerve exams.
Quantitative Sensory Testing (QST)
- QST is a protocol for assessing thermal and mechanical sensory function.
- QST assesses pain mechanisms by evaluating a patient's response to standardized stimuli.
- QST is useful in various conditions including neuropathic pain, polyneuropathy, postherpetic neuralgia, CRPS, chronic back pain, and knee osteoarthritis.
Cranial Nerve Dysfunctions
- Local anesthesia complications, neuralgias (like facial pain), infarcts/strokes, infections (bacterial/viral), toxins (drugs), trauma, and tumors can cause cranial nerve dysfunction.
- Bell's palsy: Idiopathic facial paralysis, the most frequent cause of unilateral facial palsy, is characterized by acute onset, unilateral weakness, sensory disturbance (taste), and often secretory reduction (salivary gland function).
- Ramsay Hunt Syndrome: A herpes zoster complication affecting the geniculate ganglion, characterized by ear pain, facial paralysis, and possible hearing loss.
- Trigeminal Neuralgia: A painful condition affecting the face unilaterally in the branches of the trigeminal nerve, characterized by brief, severe, electric shock-like pain.
- Cavernous Sinus Syndrome: A rare condition with eye muscle dysfunction, congestion, and potential trigeminal sensory loss, frequently due to local infections or trauma.
- Horner's Syndrome: Characterized by miosis (constricted pupils), partial ptosis (drooping eyelid), and hemifacial sweating loss due to sympathetics nerves damage.
- Superior Orbital Fissure Syndrome: A rare syndrome caused by damage to the cranial nerves passing through the superior orbital fissure, causing eye muscle problems and sensory loss.
Key Messages
- Proper understanding of cranial nerve anatomy and function is crucial for accurate interpretations of diagnostic findings.
- The knowledge is essential for proper patient diagnosis and appropriate medical referral or treatment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers essential aspects of neurology examinations, focusing on cranial nerve assessments and Quantitative Sensory Testing (QST). Test your knowledge on assessing nerve function, understanding pain types, and interpreting cranial nerve dysfunctions. Ideal for students and professionals in the medical field.