Podcast
Questions and Answers
During which period does the nervous system first begin to form?
During which period does the nervous system first begin to form?
- Late childhood
- Early embryonic development (correct)
- Early childhood
- Infancy
Which of the following is a primary function regulated by the autonomic nervous system (ANS)?
Which of the following is a primary function regulated by the autonomic nervous system (ANS)?
- Voluntary muscle movement
- Involuntary body functions (correct)
- Language comprehension
- Conscious thought processing
What is the main function of the sympathetic nervous system (SNS)?
What is the main function of the sympathetic nervous system (SNS)?
- To promote digestion
- To conserve energy
- To initiate the 'rest and digest' response
- To activate the 'fight or flight' response (correct)
Dura mater, arachnoid membrane and pia mater provide what?
Dura mater, arachnoid membrane and pia mater provide what?
What is the role of cerebral spinal fluid (CSF) in the brain?
What is the role of cerebral spinal fluid (CSF) in the brain?
What is the primary function of myelination?
What is the primary function of myelination?
When assessing a child for a neurological condition, which of the following would be the MOST important to assess FIRST?
When assessing a child for a neurological condition, which of the following would be the MOST important to assess FIRST?
A child is described as being sluggish and apathetic. Which level of consciousness best describes this?
A child is described as being sluggish and apathetic. Which level of consciousness best describes this?
What is proprioception?
What is proprioception?
Which condition involves a child being born with an absence of both cerebral hemispheres?
Which condition involves a child being born with an absence of both cerebral hemispheres?
A child is born with a defect in the bony spinal column resulting an abnormal protrusion. What neural tube defect does the child most likely have?
A child is born with a defect in the bony spinal column resulting an abnormal protrusion. What neural tube defect does the child most likely have?
What is a nursing consideration for a child with a neural tube defect?
What is a nursing consideration for a child with a neural tube defect?
What is the priority intervention for a child who has experienced a near drowning event?
What is the priority intervention for a child who has experienced a near drowning event?
Which intervention is key in the nursing care of premature infants at risk for intraventricular hemorrhage (IVH)?
Which intervention is key in the nursing care of premature infants at risk for intraventricular hemorrhage (IVH)?
What is the primary treatment goal for lead poisoning in children?
What is the primary treatment goal for lead poisoning in children?
Which assessment finding is MOST indicative of meningococcal meningitis in a child?
Which assessment finding is MOST indicative of meningococcal meningitis in a child?
What is a key nursing intervention in managing a child with meningitis?
What is a key nursing intervention in managing a child with meningitis?
What is the primary recommendation regarding the use of salicylates (aspirin) in children?
What is the primary recommendation regarding the use of salicylates (aspirin) in children?
In the evaluation of Reye Syndrome, what signs are present in Stage 1?
In the evaluation of Reye Syndrome, what signs are present in Stage 1?
What is the initial intervention in managing a child with a suspected spinal cord injury (SCI)?
What is the initial intervention in managing a child with a suspected spinal cord injury (SCI)?
What is the primary concern related to secondary brain injury after a traumatic brain injury (TBI)?
What is the primary concern related to secondary brain injury after a traumatic brain injury (TBI)?
What is a key measure to prevent head injuries in toddlers?
What is a key measure to prevent head injuries in toddlers?
What does post-concussion syndrome describe?
What does post-concussion syndrome describe?
What is a localized bruising of the brain tissue called?
What is a localized bruising of the brain tissue called?
A child presents with bradycardia, irregular respirations, and a widening pulse pressure. These are signs of increased intracranial pressure, known as:
A child presents with bradycardia, irregular respirations, and a widening pulse pressure. These are signs of increased intracranial pressure, known as:
Which intervention is MOST important when caring for a child with a traumatic brain injury (TBI)?
Which intervention is MOST important when caring for a child with a traumatic brain injury (TBI)?
The nurse recognizes that the most common solid malignancy during childhood is?
The nurse recognizes that the most common solid malignancy during childhood is?
A child under seven is diagnosed with a brain tumor. Which type of tumor is most likely?
A child under seven is diagnosed with a brain tumor. Which type of tumor is most likely?
What is a key nursing consideration when caring for a child with a brain tumor?
What is a key nursing consideration when caring for a child with a brain tumor?
Which type of headache may indicate head CT?
Which type of headache may indicate head CT?
What is the MOST appropriate action for a nurse to recommend to a child experiencing cluster headaches?
What is the MOST appropriate action for a nurse to recommend to a child experiencing cluster headaches?
An 11 year old child is diagnosed with moderate cognitive impairment. What is the range of their possible mental age?
An 11 year old child is diagnosed with moderate cognitive impairment. What is the range of their possible mental age?
What nursing consideration is important for a child diagnosed with Cognitive Impairment (CI)?
What nursing consideration is important for a child diagnosed with Cognitive Impairment (CI)?
What describes Hydrocephalus?
What describes Hydrocephalus?
What intervention is important for a child with Hydrocephalus?
What intervention is important for a child with Hydrocephalus?
What assessment is MOST indicative of Hydrocephalus?
What assessment is MOST indicative of Hydrocephalus?
A child is displaying decerebrate posturing and has sunset eyes. These are indications of what condition?
A child is displaying decerebrate posturing and has sunset eyes. These are indications of what condition?
What is a nursing action important for a patient with IICP?
What is a nursing action important for a patient with IICP?
Select all the manifestations of seizures.
Select all the manifestations of seizures.
A child is having a seizure. Which intervention is MOST important?
A child is having a seizure. Which intervention is MOST important?
A 17 year old states they want to start driving. What seizure consideration is important for the patient and the nurse to consider?
A 17 year old states they want to start driving. What seizure consideration is important for the patient and the nurse to consider?
Flashcards
Nervous System Development
Nervous System Development
The nervous system begins to form during early embryonic development.
Brain Function
Brain Function
The brain consists of the cerebrum, which is the center of conciousness.
ANS Function
ANS Function
The Autonomic Nervous System (ANS) controls involuntary body functions.
Sympathetic Nervous System (SNS)
Sympathetic Nervous System (SNS)
Signup and view all the flashcards
Brain Membranes
Brain Membranes
Signup and view all the flashcards
Pressure Balance
Pressure Balance
Signup and view all the flashcards
Myelination
Myelination
Signup and view all the flashcards
Cerebral Palsy (CP)
Cerebral Palsy (CP)
Signup and view all the flashcards
Types of Cerebral Palsy
Types of Cerebral Palsy
Signup and view all the flashcards
Anencephaly
Anencephaly
Signup and view all the flashcards
Microcephaly
Microcephaly
Signup and view all the flashcards
Evaluate Neural Defects
Evaluate Neural Defects
Signup and view all the flashcards
Intraventricular Hemorrhage (IVH)
Intraventricular Hemorrhage (IVH)
Signup and view all the flashcards
Lead Poisoning
Lead Poisoning
Signup and view all the flashcards
Meningitis
Meningitis
Signup and view all the flashcards
Reye Syndrome
Reye Syndrome
Signup and view all the flashcards
Reye Intervention
Reye Intervention
Signup and view all the flashcards
Complete Spinal Cord Injury (SCI)
Complete Spinal Cord Injury (SCI)
Signup and view all the flashcards
Traumatic Brain Injury (TBI)
Traumatic Brain Injury (TBI)
Signup and view all the flashcards
Protecting the Head
Protecting the Head
Signup and view all the flashcards
Concussion
Concussion
Signup and view all the flashcards
Contusion
Contusion
Signup and view all the flashcards
Brain Tumors
Brain Tumors
Signup and view all the flashcards
Migraines Evaluation
Migraines Evaluation
Signup and view all the flashcards
Cognitive Impairment (CI)
Cognitive Impairment (CI)
Signup and view all the flashcards
Hydrocephalus
Hydrocephalus
Signup and view all the flashcards
Increased Intercranial Pressure (IICP)
Increased Intercranial Pressure (IICP)
Signup and view all the flashcards
Seizure Disorder
Seizure Disorder
Signup and view all the flashcards
Seizure Interventions
Seizure Interventions
Signup and view all the flashcards
Study Notes
- This chapter discusses neurological conditions in children.
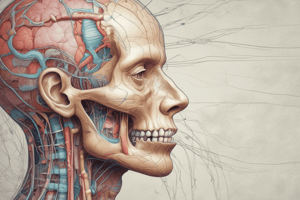
Nervous System Development
- Early embryonic development marks the beginning of nervous system formation.
- During intrauterine development the fetus responds to stimuli.
- The nervous system continues to develop after birth.
- The central nervous system (CNS) includes the brain and spinal cord.
Central Nervous System (CNS)
- The CNS consists of the brain and spinal cord.
- The brain contains the cerebrum which is the center of consciousness.
- The cerebrum is divided into two hemispheres, containing the frontal lobe, temporal lobe, parietal lobe, occipital lobe, diencephalon (thalamus and hypothalamus), cerebellum, and brainstem.
Peripheral Nervous System (PNS)
- The PNS includes 12 pairs of cranial nerves and 31 pairs of spinal nerves.
Cranial Nerves
- I: Olfactory
- II: Optic
- III: Oculomotor
- IV: Trochlear
- V: Trigeminal
- VI: Abducens
- VII: Facial
- IX: Glossopharyngeal
- X: Vagus
- XI: Spinal accessory
- XII: Hypoglossal
Autonomic Nervous System (ANS)
- The ANS regulates involuntary body functions.
Sympathetic Nervous System (SNS)
- The SNS triggers emergency responses to stimuli
- The SNS initiates the "fight or flight" response.
Parasympathetic Nervous System
- The parasympathetic nervous system influences muscle tone with the relaxation of sphincter muscles.
- The parasympathetic nervous system is responsible for "rest and digest".
Autonomic Innervation of Selected Body Structures
- Eye pupil (iris)
- Sympathetic dilates
- Parasympathetic constricts
- Heart
- Sympathetic increases rate and force
- Parasympathetic decreases rate
- Lung bronchioles
- Sympathetic dilates
- Parasympathetic constricts
- Gut wall
- Sympathetic decreases motility
- Parasympathetic increases motility
- Gut sphincter
- Sympathetic constricts
- Parasympathetic relaxes
- Bladder detrusor
- Sympathetic relaxes
- Parasympathetic contracts
- Bladder-urethra smooth sphincter
- Sympathetic constricts
- Parasympathetic relaxes
- Penis
- Sympathetic ejaculation
- Parasympathetic erection
- Gallbladder bile & duct
- Sympathetic relaxes
- Parasympathetic contracts
- Salivary glands
- Sympathetic concentrates viscous saliva
- Parasympathetic increases abundant watery saliva
- Nasal & lacrimal glands
- Sympathetic vasoconstricts
- Parasympathetic causes abundant secretion
Brain Anatomy
- The brain exhibits dura mater, arachnoid membrane, and pia matter which are three protective membranes.
- Cerebral spinal fluid (CSF) forms in the brains the lateral ventricles.
Intracranial Pressure Balance
- Intracranial pressure balance is maintained by production and absorption of CSF within the brain.
- Blood vessel dilation and constriction within the brain maintain intracranial pressure.
- Production and circulation of hormones increase or decrease urine production to balance intracranial pressure.
Myelination
- Myelination is needed for motor control, coordination, and cognitive maturity.
- Myelination is the creation of a protective coating around nerve fibers.
Pediatric Neurological Assessment
- Comprehensive assessment for children: Detailed health history, physical examination, lab studies, diagnostic tests and reflexes (Moro's, sucking, fencing/tonic, plantar, palmer, Babinski's, rooting, stepping, crawling, and step).
Levels of Consciousness
- Full conscious is normal consciousness where person is alert, oriented, and communicating.
- Confusion is reduced awareness of being, bewildered and unable to think clearly.
- Disorientation means not oriented to personal, place, or time with a deepened state of confusion.
- Lethargic is being sluggish, or apathetic, and unable to stay aroused.
- Obtunded is loss of sensitivity to one's surroundings.
- Coma is deep unconsciousness/.
The Senses
- The various senses include: auditory, olfactory, tactile, visual, gustatory, and proprioception (sense of space).
Congenital Neurological Disorders
- Congenital Neurological Disorders include these conditions: Cerebral Palsy, Anencephaly, Microcephaly, Encephalocele, Spina Bifida Type 1 Meningocele, and Type 2 Meningocele.
Cerebral Palsy (CP)
- CP can occur during fetal development or during the birthing process.
- CP is caused by anoxia before, during, and after the birth process up to the second year of life.
- Types of cerebral palsy may be described as Ataxic, Spastic, Hypotonic, Dyskinetic, and Mixed.
Evaluating Cerebral Palsy
- Tight muscles that do not stretch may indicate CP
- "Scissors" movements of arms and legs may indicate CP
- Joint contractures in which the joints do not open and do not have the full range of motion (ROM) may indicate CP
- Paralysis or muscle weakness may indicate CP
- The presence of tremors, floppy extremities combined with overextended joint areas, or the presence of pain may indicate CP
Cerebral Palsy Interventions/Considerations
- Treatment includes: providing support, symptom management, interventions which promote mobility and socialization and the reduction of injuries.
- Key considerations include reducing complications associated with CP, teaching the family how to maintain a clear airway, encouraging ROM exercises, and focusing on patient safety.
Neural Tube Defects
- Neural Tube Defects include Anencephaly, Microcephaly, Encephalocele, Spina Bifida, Type 1: Myelomeningocele, and Type 2: Meningocele.
Anencephaly
- The child is born with an absence of both hemispheres with only the presence of the brainstem and cerebellum.
Microcephaly
- The child is born with an abnormally small brain and head.
- Exposure to the Zika virus is associated with congenital Zika syndrome.
- Microcephaly can lead to a small brain whose skull partially collapses.
Encephalocele
- The child is born with an abnormal sac of fluid that causes the brain and meninges to herniate/protrude through an abnormal defect in the skull.
- Brain tissue may be found within the sac.
Spina Bifida
- Myelomeningocele defines when the child is born with a portion of the vertebral column not closed, leading to a protruding sac containing CSF, meninges, and a portion of the child's spinal cord.
- 80% are located in the lumbosacral areas where it develops last.
- Meningocele defines when a child is born with a defect in the bony spinal column resulting in abnormal protrusion of a CSF-filled sac.
Evaluating Neural Tube Defects
- Evaluation includes: early fetal assessment, ultrasounds during pregnancy, measuring head circumference, assessing neurological deficiencies, and assessing bowel and bladder function.
Neural Tube Defect Interventions
- Key interventions: handle the abnormal sac with care, assess for leaks, rupture, and infection in CNS, keep the sac with NS-soaked gauze, family education, post-op fluid balance, ROM, support lower extremities and intermittent catheterization.
Neural Tube Defect Nursing Consideration
- Consider latex allergy, education on motor limitations, and education on folic acid.
Neurological Injuries
- Common neurological injuries include: drowning and near-drowning, intraventricular hemorrhage (IVH), lead poisoning meningitis, Reye's Syndrome, Spinal Cord Injury (SCI), and Traumatic Brain Injury (TBI).
Drowning and Near Drowning
- Peak periods are in toddler and adolescent periods.
- The evaluation process involves examining the airway, ventilation, ability as well as quality of respirations, HR, BP, ABGs, and LOC.
- Interventions should include CPR, use of ventilators, oxygen support IV fluids, removing wet clothes use of a warm environment and warm blankets.
- Key considerations include providing support for, the patient, the team, the patient's family contacting social worker, and spiritual support if needed.
Intraventricular Hemorrhage (IVH)
- This brain bleed is caused by rupture of the vascular network within the germinal matrix. It impacts premature infants less than 32 weeks with cases developing within four days.
- Reduce Stimuli
- Support head
- Minimize Crying
- 2 person turn
- Avoid discomfort
- Evaluation involves assessing the patient's CT, MRI, labs, H&H, ICP, and fontanels.
- Interventions involve reducing stimuli, minimizing handling, transfusion therapy, and ventriculostomy.
- Keep head midline
- Support head
- Implement 2-person turns.
- Avoid discomfort.
- Minimize crying.
Lead Poisoning
- Irreversibly impairs brain function and can lead to encephalopathy.
- Evaluation involves lab tests at ages 1 & 2, environment assessments, monitoring for PICA behavior, and assessing teething behaviors.
- Interventions and Considerations can include: Checking lead levels, identifying the source, treating the source, monitoring behavior changes.
- Exposure sources may include contaminated soil, contaminated parent clothing, lead-based paints, imported candy, jewelry, pottery, contaminated household dust, lead pipes, imported canned foods, and brass fixtures.
- Metallic Taste in mouth
- Gastrointestinal (GI) upset, including abdominal cramping
- Decreased UOP
- Alteration in thinking
- Parents describing their child has a "personality change."
- Black or Blue discoloration or line along the gums
- Paresthesias or abnormal sensations
- Chelation Therapy can be implemented with lead levels of 45mcg/dL.
Meningitis
- Meningitis is inflammation of the membranes of the brain or spinal cord.
- Meningitis is an often infectious (bacterial, viral chemical agent).
- If bacterial and Viral meningitis it can spread through droplets.
- Symptoms for bacterial meningitis, which is severe include: rapid on-set, high mortality, sudden infection resulting in DIC, massive hemorrhages, and purple rash or petechial rash.
Meningitis Signs & Symptoms
- Poor feeding habits
- Fever
- Lethargy.
- Bulging fontanels.
- Irritability
- Inconsolable when held
- High Pitched cry
- Opisthotonos.
- Kernig’s sign.
- Brudzinski’s sign.
Meningitis Interventions & Nursing Considerations
- Patent IV
- IV Antibiotics
- Monitor ICP
- Measure Head Circumference
- Provide Antibiotics
- Provide Corticosteroids
- Blood Cultures
- Labs
- Spinal tap
- Anticonvulsants
Reye Syndrome
- Non-specific noninflammatory, encephalopathy involving the liver, spleen, kidney, pancreas, and lymph. Is strongly associated with salicylates- aspiring(ASA).
- Evaluating Reye's Syndrome focuses on frequent vomiting and diarrhea (early stage), rapid breathing (early stage in infancy), Encephalopathy (later stage), Increased ICP (later stage), Metabolic dysfunction (later stage), Hepatic dysfunction (later stage), Renal damage (later stage), Fatty infiltration of the viscera (later stage), Confusion, irrational behavior, and loss of consciousness (later stage).
- Frequent vomiting and diarrhea
- Rapid breathing Metabolic dysfunction
- Fatty infiltration of the viscera.
- Monitor for Hypoxia, Seizures, Hyperthermia, Hypoglycemia, Coagulopathy.
Reye Syndrome Interventions
- Carefully monitor the client as they progress through Reye's syndrome.
- Monitor for changes in neurological status and reporting any changes.
- Continually assess for GI bleeding, pancreatitis, or liver failure.
- Implement seizure precautionsImplement seizure precautions
- Check Glascow Coma Scale
- Manage wounds on the patients liver
- Provide hydration with a source of glucose (IV fluids).
- Assess for increasing ICP.
- Reinforcing patient family teaching about follow-up.
- Provide a quiet environment.
Spinal Cord Injury (SCI)
- Complete SCI refers to a complete loss of sensorimotor and reflex activity below the site of injury.
- Incomplete SCI refers to the preservation of some motor/sensory function below the site of injury.
- Sacral sparing SCI refers to motor and sensory in the anal mucocutaneous border exists.
- Evaluation is performed by neuro exam, followed by CT/MRI scan. In alignment a cervical collar may be placed.
- Stabilization alignment: straight backboard with alignment .
- Spinal cord injury may result in patients needing catheterization due to not being able to eliminate waste.
Traumatic Brain Injury (TBI)
- Primary TBI refers to the impact of trauma/injury where the brain tissue is damaged.
- Secondary TBI when the body responds to initial trauma/injury.
Protecting the head from injury
- Neonate: Head should be supported, head and neck alinement/handle with Care, do not shake the head.
- Infant: Use car seats correctly correct head cushions, prevent falls, no baby wallers on stairs.
- Toddler: Forward-facing- Prevent falling in water- helmet/ prevent Tricycle injuries/ helmet.
- Preschooler: Follow safety rules and follow all safe sporting events must supervised at all times. Use foam padding to prevent falls from structures
- School age: Safety devices and protectives sports equipment. Do not use sharp objects around the head and neck.
- Adolescent: Always follow seat belt, avoid texting while driving. Avoid head injuries when water activities or engaging in sports.
Concussion
- Concussion refers to transient loss of consciousness from shearing/compression of brain's nerve tissue.
- A concussion may present as a mild traumatic brain injury.
- Post-concussion syndrome is when patient may have head aches and memory problems
- Concussions from contact sports must be checked immediately by sports healthcare and teams Families need to be Educated on about their symptoms and the rest needed.
Contusion
- Contusion is localized brain tissue injuries and Traumatice brain injuries often occur during trauma and are caused by damaged vasculature and and or Tissue.
Evaluating TBI
- Assess airway, vitals for effective breathing, heart problems, and shock
- Monitor vitals, neurological checks, signs of shock, poor perfusion, increased Intracranial pressure (ICP).
- Check the status of Cushing's triad, blood patterns, and assess cranial nerves
- Monitor LOC ,Assess GCS, and preform neurological examinations.
TBI Interventions
- Provide airway maintenance, low stimulation, and increase HOB
- Steroids, ventilator as needed, HOB/ reduce ICP, check transducer, hyperosmolar saline
TBI Nursing Considerations
- Monitor for subtle changes in clinical care airway, possible npo status, preventing aspiration, perform Turning on the patients.
Other Neurological Disorders
- Other neurological disorders include: brain tumors, migraines, cognitive impairment, hydrocephalus, increased Intracranial pressure, and seizure disorders.
Brain Tumors
- Brain tumors indicate malignancy, the most common solid malignancy during childhood with a frequency second to leukemia.
- Tumors are graded according classification and location.
- Brain tumors are graded either low (localized) or high or invasive.
- Brain tumors are common under children 7 that have medulloblastoma.
Brain Tumors (Evaluation Interventions, & Nursing Consideration
- Increased intracranial pressure
- Provide Increased intercranial space
- Radiation
- Provide consideration and radiation care
- Suport of surgery
- Maintain intercranial space.
- Educate the family support and preparation
Migraine Headaches
- Types of migraine headaches may be categorized as: chronic daily headaches, cluster headaches, tension headaches or psychogenic headaches.
- Migraine Evaluation involves assessments for Health history, family history, Risk factors, Physical, exam signs of infection, and a head CT.
- Treatment of any infections or complications must occur. Hospitalization occurs. Vision may be check for sign's of strain
- Counciling and Neurology follow ups can be helpful
- Take a holistic approach with the patient
Cognitive Impairment (CI)
- Cognitive Impairment refers to limitations in intellectual functioning and adaptive behaviors.
- Evaluation includes: a focus on developmental status.
- Nursing considerations - focus on accomplishments with recognition. And local area support for organizations.
Hydrocephalus
- Hydrocephalus occurs when the brain has too much CSF in the brain.
- Non Communicating;
- Obstructing
- Communicating to impaired-Impared absorption of CSF often.
Hydrocephalus Evaluation & Interventions
- Frequently check head and palpate.
- Childs with high pitched cry are irratiblitaly will have acute vomiting, monitor.
- Vp shunt
- Educate of the changes of assess and ICP for the body.
Increased Intracranial Pressure (IICP)
- May be cuased by Cerebral edema, abscesses, meningitis, tumors, h20 intoxication/Hydrocephalus,
- The body might start herinating . Deterioration of brain/ stem apnea and death. History must includes/ trauma/ blleding disoders/exrensive vears-over-dehydration of a child with DKA.
- Evaluating IICP may cause problems during Sunset years, Posturing/macewena’s sign/diplopian/seizures/pupiels
- Maintain Peyton, Oxygen, and intubate
- Treat seizure with lights
- Rapid and Maintain iv. Give diuretics/ corticosteroids
Seizure Disorder
- This disruption of communication among neroun that results in abrnomal discharge of eletricals activity within the brain. During the brain will start firing electricity that is expected. This expected patterns will resuot and lead to stimual and cause the seizure
- 40 % off cuoldhood seizure is partial cause of most neontal and infant remains unknown do not conititue the most CNS inry Evaluation:
- Always ask their background when seizure started.
- And how it came about-look for signs of auras loss of consciousness
Interventions
- Maintain save enviroment- utilitize seizure -Do not-restris body part- airaway will need to be a patent to prevent the administration of precribed medication and electrolytes.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.