Podcast
Questions and Answers
What condition is characterized by severe atrophy leading to thin slivers of affected gyri?
What condition is characterized by severe atrophy leading to thin slivers of affected gyri?
- Excitotoxicity
- Cortical dysplasia
- Subcortical edema
- Knife-edge atrophy (correct)
Which type of photoreceptor is primarily responsible for night vision?
Which type of photoreceptor is primarily responsible for night vision?
- Cones
- Bipolar cells
- Ganglion cells
- Rods (correct)
Which protein aggregations are characteristic of Pick Disease?
Which protein aggregations are characteristic of Pick Disease?
- Beta-amyloid plaques
- Neurofibrillary tangles
- Lewy bodies
- Pick bodies (correct)
What is typically compromised in individuals with the behavioral variant of Pick Disease?
What is typically compromised in individuals with the behavioral variant of Pick Disease?
What is the main function of cones in the visual system?
What is the main function of cones in the visual system?
What role do the sinuses play in relation to the skull?
What role do the sinuses play in relation to the skull?
Which variant of Primary Progressive Aphasia involves a decline in word meaning comprehension?
Which variant of Primary Progressive Aphasia involves a decline in word meaning comprehension?
Where are cones primarily concentrated in the eye?
Where are cones primarily concentrated in the eye?
What type of light activation is required for rods compared to cones?
What type of light activation is required for rods compared to cones?
What clinical feature may initially lead to a misdiagnosis in Pick Disease?
What clinical feature may initially lead to a misdiagnosis in Pick Disease?
Which sinus empties into the anterior part of the hiatus semilunaris?
Which sinus empties into the anterior part of the hiatus semilunaris?
Which type of cone detects short wavelengths of light?
Which type of cone detects short wavelengths of light?
Which of the following is NOT one of the three main clinical syndromes of Pick Disease?
Which of the following is NOT one of the three main clinical syndromes of Pick Disease?
Which nerve is primarily responsible for the sense of smell?
Which nerve is primarily responsible for the sense of smell?
What provides blood supply to the vestibule of the nose?
What provides blood supply to the vestibule of the nose?
What type of inclusions do residual neurons exhibit in Pick Disease?
What type of inclusions do residual neurons exhibit in Pick Disease?
In terms of visual acuity, how do rods and cones differ?
In terms of visual acuity, how do rods and cones differ?
What does the inferior meatus receive drainage from?
What does the inferior meatus receive drainage from?
In the context of the behavioral variant of Pick Disease, which symptom is commonly observed?
In the context of the behavioral variant of Pick Disease, which symptom is commonly observed?
How do the visual functions of rods and cones compare in terms of color detection?
How do the visual functions of rods and cones compare in terms of color detection?
What is one of the primary functions of the nasal conchae?
What is one of the primary functions of the nasal conchae?
What is the role of the superior meatus in the nasal cavity?
What is the role of the superior meatus in the nasal cavity?
What defines the lower limit of the mouth?
What defines the lower limit of the mouth?
What phenomenon is observed when a dim star disappears when looked at directly?
What phenomenon is observed when a dim star disappears when looked at directly?
How do the nasal conchae contribute to the humidification of inhaled air?
How do the nasal conchae contribute to the humidification of inhaled air?
Which branch of the trigeminal nerve carries sensation from the nasal septum?
Which branch of the trigeminal nerve carries sensation from the nasal septum?
Which artery supplies blood to the roof of the nose?
Which artery supplies blood to the roof of the nose?
Which structure drains into the inferior meatus?
Which structure drains into the inferior meatus?
Which nasal concha has a specific role in enhancing the sense of smell?
Which nasal concha has a specific role in enhancing the sense of smell?
What is the primary function of the ciliated epithelial layer lining the paranasal sinuses?
What is the primary function of the ciliated epithelial layer lining the paranasal sinuses?
Which meatus is specifically critical for sinus drainage and ventilation?
Which meatus is specifically critical for sinus drainage and ventilation?
What type of epithelium primarily lines the nasal cavity?
What type of epithelium primarily lines the nasal cavity?
Which neurodegenerative disease is primarily characterized by the accumulation of amyloid plaques and neurofibrillary tangles in the brain?
Which neurodegenerative disease is primarily characterized by the accumulation of amyloid plaques and neurofibrillary tangles in the brain?
What type of dementia is most commonly associated with motor symptoms such as tremors, rigidity, and bradykinesia?
What type of dementia is most commonly associated with motor symptoms such as tremors, rigidity, and bradykinesia?
What primarily characterizes Alzheimer's disease?
What primarily characterizes Alzheimer's disease?
Which type of dementia results from multiple small strokes or impaired blood flow to the brain, leading to a gradual decline in cognitive function?
Which type of dementia results from multiple small strokes or impaired blood flow to the brain, leading to a gradual decline in cognitive function?
Which age group is most significantly affected by Alzheimer's disease?
Which age group is most significantly affected by Alzheimer's disease?
Which neurodegenerative disease is primarily characterized by visual hallucinations and fluctuating cognition?
Which neurodegenerative disease is primarily characterized by visual hallucinations and fluctuating cognition?
Which of the following is NOT a common pathological feature of Alzheimer's disease?
Which of the following is NOT a common pathological feature of Alzheimer's disease?
Which type of dementia is characterized by personality changes and impaired social behaviors due to degeneration of the frontal lobe?
Which type of dementia is characterized by personality changes and impaired social behaviors due to degeneration of the frontal lobe?
What is the role of reactive astrocytes and microglia in the context of Alzheimer's disease pathology?
What is the role of reactive astrocytes and microglia in the context of Alzheimer's disease pathology?
Which neurodegenerative disease initially manifests with memory loss but later progresses to include significant language difficulties?
Which neurodegenerative disease initially manifests with memory loss but later progresses to include significant language difficulties?
How does the quantity and distribution of senile plaques correlate with clinical disease severity in Alzheimer's?
How does the quantity and distribution of senile plaques correlate with clinical disease severity in Alzheimer's?
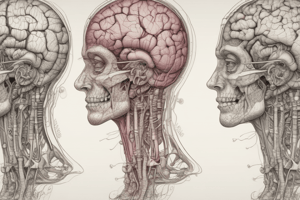
What structural change occurs in the brain's appearance in advanced Alzheimer's disease?
What structural change occurs in the brain's appearance in advanced Alzheimer's disease?
What common feature distinguishes vascular dementia from other types of dementia?
What common feature distinguishes vascular dementia from other types of dementia?
Which of the following best describes neurofibrillary tangles in Alzheimer's disease?
Which of the following best describes neurofibrillary tangles in Alzheimer's disease?
Which type of dementia can often be mistaken for Alzheimer's disease due to shared early symptoms, yet has different underlying causes?
Which type of dementia can often be mistaken for Alzheimer's disease due to shared early symptoms, yet has different underlying causes?
Which proteins are primarily involved in the neurodegenerative process of Alzheimer's disease?
Which proteins are primarily involved in the neurodegenerative process of Alzheimer's disease?
Flashcards
Sinuses
Sinuses
Openings in the skull that connect to the nasal cavity, serving as resonant chambers and reducing skull weight.
Frontal sinus drainage
Frontal sinus drainage
The frontal sinus drains into the anterior part of the hiatus semilunaris through the infundibulum.
Maxillary and ethmoidal sinus drainage
Maxillary and ethmoidal sinus drainage
The maxillary sinus, anterior and middle ethmoidal sinuses drain into the hiatus semilunaris.
Posterior ethmoidal sinus drainage
Posterior ethmoidal sinus drainage
Signup and view all the flashcards
Sphenoid sinus drainage
Sphenoid sinus drainage
Signup and view all the flashcards
Tears drainage
Tears drainage
Signup and view all the flashcards
Olfactory nerves
Olfactory nerves
Signup and view all the flashcards
General sensation of nasal cavity
General sensation of nasal cavity
Signup and view all the flashcards
What is the main characteristic of Alzheimer's disease?
What is the main characteristic of Alzheimer's disease?
Signup and view all the flashcards
What distinguishes Lewy body dementia?
What distinguishes Lewy body dementia?
Signup and view all the flashcards
What is the primary cause of vascular dementia?
What is the primary cause of vascular dementia?
Signup and view all the flashcards
What is Parkinson's dementia associated with?
What is Parkinson's dementia associated with?
Signup and view all the flashcards
What is the primary area of the brain affected by frontotemporal dementia?
What is the primary area of the brain affected by frontotemporal dementia?
Signup and view all the flashcards
What are nasal conchae?
What are nasal conchae?
Signup and view all the flashcards
What are the meatuses in the nasal cavity?
What are the meatuses in the nasal cavity?
Signup and view all the flashcards
What is the Superior Meatus?
What is the Superior Meatus?
Signup and view all the flashcards
What is the Middle Meatus?
What is the Middle Meatus?
Signup and view all the flashcards
What is the Inferior Meatus?
What is the Inferior Meatus?
Signup and view all the flashcards
What is the mucous membrane in the nasal cavity?
What is the mucous membrane in the nasal cavity?
Signup and view all the flashcards
What are the paranasal sinuses?
What are the paranasal sinuses?
Signup and view all the flashcards
What is the function of the ciliary action in the paranasal sinuses?
What is the function of the ciliary action in the paranasal sinuses?
Signup and view all the flashcards
Alzheimer's Disease (AD)
Alzheimer's Disease (AD)
Signup and view all the flashcards
Senile Plaques
Senile Plaques
Signup and view all the flashcards
Neurofibrillary Tangles
Neurofibrillary Tangles
Signup and view all the flashcards
Proteostasis
Proteostasis
Signup and view all the flashcards
Proteostasis Disruption
Proteostasis Disruption
Signup and view all the flashcards
Neurodegenerative Diseases
Neurodegenerative Diseases
Signup and view all the flashcards
Cortical Atrophy
Cortical Atrophy
Signup and view all the flashcards
Dementia
Dementia
Signup and view all the flashcards
Visual Acuity
Visual Acuity
Signup and view all the flashcards
Rods
Rods
Signup and view all the flashcards
Cones
Cones
Signup and view all the flashcards
Convergence
Convergence
Signup and view all the flashcards
Fovea
Fovea
Signup and view all the flashcards
Blind Spot
Blind Spot
Signup and view all the flashcards
S, M, and L Cones
S, M, and L Cones
Signup and view all the flashcards
Colour Perception
Colour Perception
Signup and view all the flashcards
Knife-edge Atrophy
Knife-edge Atrophy
Signup and view all the flashcards
Pick Disease
Pick Disease
Signup and view all the flashcards
Pick Bodies
Pick Bodies
Signup and view all the flashcards
Behavioral Variant Pick Disease
Behavioral Variant Pick Disease
Signup and view all the flashcards
Semantic Variant Primary Progressive Aphasia
Semantic Variant Primary Progressive Aphasia
Signup and view all the flashcards
Nonfluent/Agrammatic Variant Primary Progressive Aphasia
Nonfluent/Agrammatic Variant Primary Progressive Aphasia
Signup and view all the flashcards
Motor Neuron Disease
Motor Neuron Disease
Signup and view all the flashcards
Astrogliosis
Astrogliosis
Signup and view all the flashcards
Study Notes
General Information
- HEENT 3 is a subject covering the general anatomy of the mouth and sinuses, along with the neurology of the olfactory and gustatory pathways.
- The material is part of a BMS 200 course, likely within a Naturopathic Medicine program.
Anatomy - Nose and Sinuses
- Upper nasal cavity boundary: the cribriform plate of the ethmoid bone.
- Lower boundary: the hard palate.
- Choanae: openings leading to the nasopharynx.
Anatomy - Nose and Sinuses (Ethmoid Bone)
- The cribriform plate is a horizontal, perforated bone structure forming part of the ethmoid bone. It separates nasal cavity from cranial cavity and supports the olfactory bulb.
- Perforations in the cribriform plate allow olfactory nerves (CN I) to pass through, facilitating smell.
- Any injury can cause CSF leakage leading to cerebrospinal fluid (CSF) leak or rhinorrhea.
Anatomy - Nose and Sinuses (Hard Palate)
- The hard palate forms the floor of the nasal cavity.
- Composed of: the palatine processes of the maxilla (anteriorly) and the horizontal plates of the palatine bones (posteriorly).
- It separates the nasal cavity from the oral cavity.
- The hard palate is important for chewing, speech, and swallowing.
Anatomy - Nose and Sinuses (Choanae)
- Choanae are funnel-shaped openings located at the posterior aspect of the nasal cavity.
- They connect the nasal cavity to the nasopharynx.
- Choanae (singular: choana) function as a passageway for airflow from the nasal cavity.
Anatomy - Nose and Sinuses (Meatuses)
- Meatuses are narrow air passages located between the nasal conchae and the lateral walls of the nasal cavity.
- Superior meatus: drains posterior ethmoidal air cells, facilitating airflow to the olfactory region.
- Middle meatus: houses middle ethmoidal air cells, and transmits drainage from frontal sinus, maxillary sinus, and anterior ethmoidal air cells.
- Inferior meatus: houses the nasolacrimal duct, which drains tears from the lacrimal sac into the nasal cavity.
Anatomy - Nose and Sinuses (Nasal Conchae)
- The three nasal conchae (Superior, Middle, Inferior) are curved, bony projections on the lateral walls of the nasal cavity.
- Covered in highly vascularized mucosa, playing a role in conditioning inhaled air.
- Functions:
- Amplify Surface Area - increasing the nasal mucosa's area optimizes the air-conditioning process.
- Induce Air Turbulence - promotes contact with the mucosa as air swirls across the conchae.
- Humidification - the mucosa warms and moistens incoming air to match body temperature, maintaining respiratory tract function.
- Filtration - particles and pathogens in inhaled air are trapped in the mucosal lining to protect the lower respiratory tract.
- Olfactory Role - the superior concha directs air towards the olfactory region, enhancing smell.
Anatomy - Oral Cavity (General)
- The upper boundary of the mouth is formed by the palate, with the mylohyoid muscle defining its lower limit.
- Cheeks are bordered by the buccinator muscles.
- The posterior boundary is marked by the palatoglossal arches.
- The mouth encompasses the vestibule, an area situated between the teeth and the cheeks.
Anatomy - Palate
- The hard palate is formed from the fusion of the palatal process of the maxilla and the horizontal process of the palatine bone.
- Muscles of the soft palate: Tensor Veli Palatini, Levator Veli Palatini, Palatoglossus, Palatopharyngeus, and Musculus Uvulae.
Anatomy - Tongue
- Foliate, fungiform, filiform, and vallate papillae cover the surface of the front two-thirds of the tongue.
- Lingual tonsils, clusters of lymphoid tissue, are found in the posterior third of the tongue.
Anatomy - Oral Cavity (Muscles)
- The tongue is a highly flexible muscular organ for speaking, eating, and swallowing.
- It's controlled by intrinsic muscles (longitudinal, vertical, transverse) that alter its shape, plus extrinsic muscles that facilitate movement.
- Muscles: Genioglossus (extend and lower), Hyoglossus (lower and pull back rear), Styloglossus (lift and retract), and Palatoglossus (associated with palate).
Anatomy - Oral Cavity (Arteries)
- Lingual artery, a branch of the external carotid artery, supplies the tongue.
Anatomy - Eye (General)
- The eye comprises the cornea, iris, lens, and retina.
- Each part plays a critical role in vision.
- Visual information transmits via complex interactions of retinal components to visual centers of the brain.
Eye Physiology & Histology 1
- General structure and function of the human eye.
- Outcomes: describe eye anatomy (cornea, iris, lens, retina), major components of vision & interaction, and photoreceptor cells (rods and cones) for light transduction.
The Eye - Getting Familiar
- Diagram of the eye, showing major structures (sclera, choroid, retina, fovea centralis, central artery, central vein, optic nerve, conjunctiva, ciliary body, posterior/anterior chambers, cornea, pupil, lens, iris, vitreous chamber).
What Does the Eye Do (Light-Focusing Functions)?
- Light focusing functions in the eye include: (1) changes in lens shape to adjust focus (accommodation) based on object distance, and (2) pupil size changes that support focusing.
What Does the Eye Do (Transparency)?
- Transparency is achieved with a highly organized structure in the lens and cornea to maximize transparency.
- Light signals get transduced into electrical signals.
- Protective structures (robust sclera, fat in the orbit, and eyelids) safeguard the eye from physical, chemical, and infectious damage.
- Eyelids, eyelashes, and tear production aid the eye's health.
The Eye - Focusing
- The eye's focusing is accomplished via the Extraocular Muscles (EOMs); and the ciliary body and ciliary muscles.
The Eye - Transparency
- Transparency is maintained by the cornea and lens' highly organized structure.
- Light gets transduced and sent to the brain in 2D maps.
- The eye is protected from damage from outside by robust sclera and orbit fat.
- Lacrimal secretions and eyelids/eyelashes aid eye health.
Eye Structure - Anatomy and Histology
- The eye is made up of three layers:
- Fibrous tunic (sclera & cornea): Provides shape, protection; cornea for refraction.
- Vascular tunic (choroid, ciliary body & iris): Supplies nutrients; melanin absorbs stray light.
- Neurosensory layer: retina, processes visual information
Fibrous Layer Basics
- Sclera: opaque, dense irregular connective tissue, strong, outer layer, site for extrinsic eye muscle attachment.
- Cornea: transparent, avascular, composed of 5 layers; external stratified squamous epithelium, stroma (organized collagen bundles), endothelium (basement membrane).
Cornea Histology Facts
- Bowman's membrane: strong barrier to infection.
- Corneal stroma: ~99% of the cornea's thickness, made of uniform collagen fibers for transparency.
- Corneal endothelium: helps maintain cornea's transparency and appropriate hydration via fluid transfer from the anterior chamber.
- Limbus: region where cornea meets sclera, source of stem cells.
Vascular Tunic Basics
- Choroid: vascularized connective tissue with melanocytes; absorbs light to avoid scattering, posterior two-thirds of the eye.
- Ciliary body: includes ciliary muscles, processes, and zonule; controls lens shape and accommodation.
Simplified Function – Ciliary Muscles and Zonular Ligaments
- Accommodation (process of the eye focusing on objects) results from the changing shape of the lens.
- Ciliary muscles and zonular ligaments play critical role in lens shape changes, adjusting focus for near or far objects.
Production of Aqueous Humor
- Aqueous humor circulates from the posterior chamber to the anterior chamber.
- Ciliary processes secrete aqueous humor.
- This fluid maintains the anterior segment and facilitates proper refraction.
Production of Aqueous Humor (Scleral Venous Sinus)
- The scleral venous sinus is found at the junction of the cornea and sclera.
- It's a complex filter (trabecular meshwork), mostly fibroblasts and ECM.
- The iris can "flop over" the scleral venous sinus - blocking fluid drainage.
- The angle between the iris and lens impacts fluid drainage.
Iris - Basics
- The iris is located in the anterior most part of the vascular layer and covers the lens.
- The iris has two major muscles that govern pupil size: dilator pupillae (sympathetic NS) and sphincter pupillae (parasympathetic NS).
Vitreous Body Basics
- The vitreous body is a clear, gel-like tissue located in the posterior cavity.
- This structure is primarily 99% water with collagen fibrils and hyaluronate; hyalocytes build the ECM.
- It connects to the retina at the inner limiting membrane.
Retina - The Basics
- Embryologically derived from the diencephalon and histologically resembles the CNS.
- Nine layers have specialized functions.
- The retina's regions display differences in rod/cone makeup for optimized vision.
- Layers include retinal blood vessels, pigment epithelial layer, and photoreceptor cells (rods & cones).
Layers of the Retina
- Layers of the retina, including nerve fiber layer, ganglion cell layer, inner plexiform layer, inner nuclear layer, outer plexiform layer, outer nuclear layer, outer limiting membrane, and photoreceptor layer to pigment epithelium layer.
Differences Across the Retina
- Fovea centralis is primarily cone-driven for high visual acuity.
- Retina contains a majority of rods for optimal night vision in peripheral areas.
- The optic disc is where the optic nerve exits the retina, lacking photoreceptors. The optic disc is also known as the blind spot, which is why you can't perceive any image in this area of the retina.
The Lens
- The lens is a transparent, ectodermally-derived tissue with highly specialized epithelial cells called lens fibers, whose elasticity decreases with age.
- Lens cells are vital for refractive properties of the eye.
- The lens has an epithelium region with simple cuboidal cells.
The Lens - Structural Basics
- The lens structure has three components: lens capsule.
- lens epithelium
- differentiating fibers (DLF), mature lens fibres (MLF)
- Abnormal lens function can cause loss of elasticity (presbyopia), or the formation of the opacities like cataracts.
Accommodation
- Accommodation is the process of changing the shape of the lens to focus light on the retina. This mainly involves adjustment between distant and near objects.
- Lens convexity (rounding) is increased for near vision under parasympathetic control. The oculomotor nerve fires and ciliary muscle contracts, relaxing the zonular ligaments.
- Distant vision: The ciliary muscle is relaxed, and the suspensory ligament is tight, resulting in a flattened lens.
Accommodation
- Constriction of the pupil, or miosis, is driven by parasympathetic control and mediated by the oculomotor nerve. - Bright light leads to pupillary constriction.
- Dilation of the pupil, or mydriasis, is driven under sympathetic nervous system control. Dim light leads to pupillary dilation.
More on the Lens (Myopia/Hyperopia)
- Myopia (nearsightedness): distant images focus in front of the retina, requiring a concave lens.
- Hyperopia (farsightedness): distant images focus behind the retina, requiring a convex lens.
Visual Acuity
- Visual acuity is measured using an eye chart (such as the Snellen chart).
- Normal vision is 20/20, meaning the patient can read the chart from 20 feet, at a distance that a normal person can read at 20 feet.
Vision Correction - Diopters
- The strength of a corrective lens is measured in diopters.
- Diopters are inversely related to the focal length of the lens.
- Higher diopter means stronger bending of light.
Vision Correction
- Convex lenses (+): for myopia (or nearsightedness) - focusing the light from objects at a distance onto the retina.
- Concave lenses (-): for hyperopia (or farsightedness) - focusing the light from nearby objects onto the retina.
Depth Perception
- Depth perception involves the brain combining disparate images from two eyes that are offset.
- Both eyes see an overlapping view, but slightly different images, leading to retinal disparity.
- The brain determines depth based on these differences.
Retinal Cells: Rods and Cones (Structure)
- Rods and cones are photoreceptor cells.
- Both contain photopigments within saccules/disks that transform photons into electrical signals (transduction).
- Both have outer and inner segments, nuclei, and synaptic terminals.
- Rods contain rhodopsin (very sensitive).
Rods and Cones (Comparison)
- Rods: poor visual acuity, very sensitive to dim light, no colour vision.
- Cones: good visual acuity, less sensitive to dim light, colour vision (different cones detect different wavelengths of light).
- Cones are concentrated in the fovea, while rods are more abundant in the periphery, explaining why we can see dim peripheral light more easily than central.
Signal Transduction - Rods
- Light activates rhodopsin, triggering a signal cascade.
- This reduces sodium channel opening, decreasing glutamate release.
- This hyperpolarisation is vital for activating bipolar cells and initiating the visual signal.
Signal Transduction (Rods) (Detail)
- Light activates rhodopsin
- Rhodopsin activates transducin.
- Transducin activates PDE (phosphodiesterase)
- PDE converts cGMP to GMP
- Sodium channels close
- Reduced glutamate release
- Hyperpolarisation of the rod.
Signal Transduction (Rods) (Detail)
- The hyperpolarization results from a decrease in a G-protein-dependent signal in the dark.
- In the light, rhodopsin activates transducin, leading to closure of sodium channels in the outer segment. This reduces glutamate release from the rod, and activates the ON-center bipolar cells.
Color Vision
- Cones are responsible for color vision
- Three main types of cones—S, M, and L—with different sensitivity to wavelengths of light (blue, green, and red).
- Combinations of cone activation generate all colors.
Color Blindness
- Anomalies in cones cause color vision deficiencies.
- This can result in various color-mixing problems and different forms of color blindness.
Eye Parts (for review)
- Diagram showing structures of the eye to refresh memory of their roles (sclera, choroid, conjunctiva, cornea, pupil, lens, iris, retina, optic nerve, ciliary body, anterior/posterior chambers, vitreous chamber).
Dementia
- Is a syndrome, encompassing decline in cognitive function.
- Leads to difficulties executing daily activities.
- Commonly affected cognitive function is memory.
- Often associated with cellular inclusions and accumulations of extracellular proteins.
- May involve several regions of the brain.
Dementia (Risk Factors)
- Lower education levels link to increased dementia risk.
- Cognitive capacity is frequently linked to educational attainment and associated with a plateau after puberty;
- Individuals in higher-demand, challenging occupations appear less susceptible to dementia.
Dementia (Pathophysiology)
- Degenerative dementia types can be impacted by the location and extent of lesions.
- Memory impairment: occurs with widespread disease in specific cerebral areas (cerebral cortex, diencephalon, medial temporal lobes).
- Language function impairment: associated specifically with disease in the dominant hemisphere.
- Lesions in posterior regions related to reading and calculation capabilities.
Dementia (Pick's Disease, Pathology)
- Characterized by the accumulation of Tau proteins without amyloid plaques.
- Cortical atrophy (most prominently in frontotemporal regions).
- Neurofibrillary tangles occur (tau filaments within cytoplasm).
- Includes Pick bodies (round cytoplasmic inclusions).
Dementia (Vascular, Pathology)
- Caused by multiple strokes.
- Pathophysiology linked to infarctions within the brain stem, thalamus, basal ganglia, and cerebrum.
- Damage also often appears in cortical (sensory/motor) and association areas.
- Results in cumulative impact of strokes leading to cognitive impairment.
- Symptoms can range from mild to severe dependence.
Dementia (TBI, Pathology)
- Direct mechanical disruption from TBI can lead to extensive deep brain degeneration.
- Potential mechanisms include axons shearing and diffuse axonal injury.
Dementia (Gut Microbiome)
- Mounting evidence suggests a significant, though still unclear, relationship between gut microbiota and dementia development.
- Pathways may include Aβ, tau phosphorylation, neuroinflammation, neurotransmitter dysfunction, and oxidative stress.
General Notes
- The provided outlines are for a student's study of a variety of specific, medical topics.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.