Podcast
Questions and Answers
What is the most common bacterium responsible for bone infections?
What is the most common bacterium responsible for bone infections?
- S. aureus (correct)
- Salmonella
- Pseudomonas
- E. coli
Which condition might lead to an infection by Salmonellae in the bones?
Which condition might lead to an infection by Salmonellae in the bones?
- Myositis
- Gout
- Sickle-cell anemia (correct)
- Rheumatoid arthritis
What is the term for edema of a joint caused by increased synovial fluid?
What is the term for edema of a joint caused by increased synovial fluid?
- Effusion (correct)
- Infiltration
- Influx
- Sequestration
Which of the following can make bone more susceptible to infection?
Which of the following can make bone more susceptible to infection?
What is the primary function of synovial fluid in joints?
What is the primary function of synovial fluid in joints?
Which category of osteomyelitis is characterized by a long-standing bone infection?
Which category of osteomyelitis is characterized by a long-standing bone infection?
Which stage of Lyme Disease is characterized by severe joint pain and swelling of large joints, central nervous system involvement, and polyradiculopathy symptoms?
Which stage of Lyme Disease is characterized by severe joint pain and swelling of large joints, central nervous system involvement, and polyradiculopathy symptoms?
What is the most common cause of osteomyelitis in individuals with diabetes mellitus and peripheral vascular disease?
What is the most common cause of osteomyelitis in individuals with diabetes mellitus and peripheral vascular disease?
Which test is commonly used in the diagnosis of Lyme Disease despite showing false negatives?
Which test is commonly used in the diagnosis of Lyme Disease despite showing false negatives?
How long is the oral therapy typically recommended to follow the IV antibiotic therapy in the treatment of osteomyelitis?
How long is the oral therapy typically recommended to follow the IV antibiotic therapy in the treatment of osteomyelitis?
In Lyme Disease, what condition may be reported post-treatment and could be due to a prolonged immune response?
In Lyme Disease, what condition may be reported post-treatment and could be due to a prolonged immune response?
What is the most common stage of Lyme Disease presentation characterized by fever, myalgias, and erythema migrans?
What is the most common stage of Lyme Disease presentation characterized by fever, myalgias, and erythema migrans?
Which joint is typically affected in gout?
Which joint is typically affected in gout?
What is a characteristic symptom of gout?
What is a characteristic symptom of gout?
What dietary factor is a risk factor for gout?
What dietary factor is a risk factor for gout?
How can chronic gout be distinguished from osteoarthritis (OA) and rheumatoid arthritis (RA)?
How can chronic gout be distinguished from osteoarthritis (OA) and rheumatoid arthritis (RA)?
Which diagnostic test is considered the gold standard for confirming gout?
Which diagnostic test is considered the gold standard for confirming gout?
In psoriatic arthritis (PsA), what precedes joint disease?
In psoriatic arthritis (PsA), what precedes joint disease?
What is a common symptom of psoriatic arthritis (PsA) affecting the eyes?
What is a common symptom of psoriatic arthritis (PsA) affecting the eyes?
What type of drugs are specifically mentioned as a treatment for PsA?
What type of drugs are specifically mentioned as a treatment for PsA?
Flashcards
Musculoskeletal Disorders
Musculoskeletal Disorders
Inflammation of muscles, bones, and joints.
Gout
Gout
Inflammatory disorder triggered by hyperuricemia, affecting specific joints, often the big toe.
Rheumatoid Arthritis
Rheumatoid Arthritis
A common inflammatory disorder of the musculoskeletal system.
Osteomyelitis
Osteomyelitis
Signup and view all the flashcards
Bone Infection Risk Factors
Bone Infection Risk Factors
Signup and view all the flashcards
Bone Structure Infection Path
Bone Structure Infection Path
Signup and view all the flashcards
Psoriatic Arthritis (PsA)
Psoriatic Arthritis (PsA)
Signup and view all the flashcards
PsA Symptoms
PsA Symptoms
Signup and view all the flashcards
Lyme Disease
Lyme Disease
Signup and view all the flashcards
Lyme Disease Early Localized
Lyme Disease Early Localized
Signup and view all the flashcards
Lyme Disease Early Disseminated
Lyme Disease Early Disseminated
Signup and view all the flashcards
Lyme Disease Late Disseminated
Lyme Disease Late Disseminated
Signup and view all the flashcards
Gout Risk Factors
Gout Risk Factors
Signup and view all the flashcards
Gout Podagra
Gout Podagra
Signup and view all the flashcards
PsA Diagnosis
PsA Diagnosis
Signup and view all the flashcards
PsA Treatment
PsA Treatment
Signup and view all the flashcards
Hyperuricemia
Hyperuricemia
Signup and view all the flashcards
Bone Resistance to Infection
Bone Resistance to Infection
Signup and view all the flashcards
Bone Infection Cause
Bone Infection Cause
Signup and view all the flashcards
Study Notes
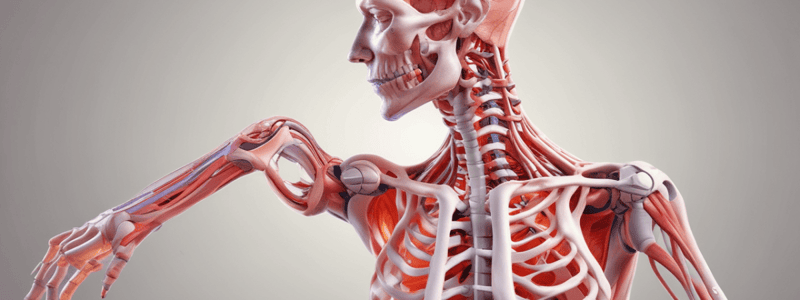
Musculoskeletal Disorders
- Inflammation of muscle, bone, and joints (Rheumatology)
- Gout and Rheumatoid Arthritis are common inflammatory disorders of the musculoskeletal system
Bone Structure and Infection
- Bone is normally resistant to infection
- Infection occurs due to break in bone or through the bloodstream
- Bacteria invade the cortex via Haversian and Volkmann canals
- Risk factors for bone infections include immunosuppression, comorbid diseases (e.g., diabetes mellitus), and nutritional deficiency
- Prosthetic material can also increase the risk of infection
Osteomyelitis
- Infection of bone, usually due to bacterial infection (Staphylococcus aureus)
- Three categories: hematogenous, contiguous, and chronic
- Presentation: recent infections, chills, fever, malaise, localized tenderness, erythema, edema, and reduced ROM in affected area
Gout
- Hyperuricemia triggers inflammation
- Affects specific joints (e.g., first metatarsal)
- Podagra: acute inflammation of the metatarsophalangeal joint of the great toe
- Primary and secondary forms
- Uric acid crystals may be deposited in subcutaneous tissue (“tophi”)
- Patient presents with redness, warmth, swelling of the joint, and discomfort onset during night or early morning
Risk Factors for Gout
- Diet high in meat (purines: uric acid)
- High alcohol consumption
- Obesity and yo-yo dieting
- Family history
- Chemotherapy resulting in cellular destruction
- Medications
Psoriatic Arthritis (PsA)
- Chronic, autoimmune inflammatory disease
- Psoriatic skin disease precedes joint disease
- Immunoglobulins deposition in epidermis
- Patterns: distal interphalangeal (DIP) predominant, arthritis mutilans, symmetric arthritis, asymmetric arthritis, and spondylitis
Symptoms of PsA
- Pain
- Swelling
- Erythema of affected joints
- Generalized fatigue
- Redness
- Eye pain
- Plaque psoriasis of the skin
- Psoriatic nail changes (pitting, ridging, and onycholysis)
Diagnosis of PsA
- Lab tests only somewhat helpful
- Need to differentiate from other arthritis forms
- Skin and nail changes are important for diagnosis
- In later stages, x-rays may show characteristic changes
Treatment of PsA
- Methotrexate
- NSAID’s
- Disease-modifying antirheumatic drugs (DMARD’s)
- Specifically TNF inhibitors
Lyme Disease
- Bacterial disease: Borrelia burgdorferi
- Transmitted by ticks (Ixodes scapularis)
- Incubation period: 7 to 14 days
- Fewer than 50% of individuals recall tick bite
- Disease manifestation due to infection and immune response
Stages of Lyme Disease
- Early localized (3–30 days post-bite): fever, myalgias, erythema migrans
- Early disseminated (3 to 12 weeks post-bite): vague, generalized symptoms, lymphocytic meningitis, cranial neuritis, carditis, and ocular involvement
- Late disseminated (months to years after bite): severe joint pain and swelling of large joints, central nervous system involvement, polyradiculopathy symptoms
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.