Podcast
Questions and Answers
Which bone is the longest in the human body?
Which bone is the longest in the human body?
- Femur (correct)
- Tibia
- Fibula
- Patella
DVT always presents with severe, debilitating pain.
DVT always presents with severe, debilitating pain.
False (B)
What is the most common and reliable test for confirming DVT?
What is the most common and reliable test for confirming DVT?
Doppler Ultrasound
The kneecap, also known as the __________, protects the knee joint.
The kneecap, also known as the __________, protects the knee joint.
Which of the following is NOT a risk factor for DVT?
Which of the following is NOT a risk factor for DVT?
The D-dimer test is highly specific for DVT.
The D-dimer test is highly specific for DVT.
What is the main goal of anticoagulation therapy in DVT?
What is the main goal of anticoagulation therapy in DVT?
__________ is a life-threatening complication of DVT where the clot travels to the lungs.
__________ is a life-threatening complication of DVT where the clot travels to the lungs.
Patients on Warfarin must avoid excessive consumption of?
Patients on Warfarin must avoid excessive consumption of?
Heparin requires routine monitoring with a blood test, while low-molecular-weight heparin (LMWH) does not.
Heparin requires routine monitoring with a blood test, while low-molecular-weight heparin (LMWH) does not.
Flashcards
Femur
Femur
The thigh bone, the longest bone in the body.
Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT)
A blood clot (thrombus) formation in a deep vein, typically in the legs.
DVT Risk Factors
DVT Risk Factors
Prolonged immobility, medical conditions, surgical procedures, hormonal factors, age, and family history.
DVT Symptoms
DVT Symptoms
Signup and view all the flashcards
Diagnosing DVT
Diagnosing DVT
Signup and view all the flashcards
Anticoagulation Therapy
Anticoagulation Therapy
Signup and view all the flashcards
Pulmonary Embolism (PE)
Pulmonary Embolism (PE)
Signup and view all the flashcards
Clotting Cascade
Clotting Cascade
Signup and view all the flashcards
Heparin Mechanism
Heparin Mechanism
Signup and view all the flashcards
Warfarin (Coumadin)
Warfarin (Coumadin)
Signup and view all the flashcards
Study Notes
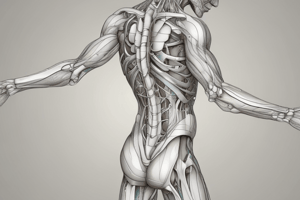
Musculoskeletal Anatomy of the Lower Limb
-
The lower limb allows movement and stability, consisting of bones, muscles, and joints
-
Bones of the Lower Limb:
- Femur: The thigh bone, it is the longest bone
- Tibia: Larger and stronger shin bone
- Fibula: Smaller lower leg bone that provides support
- Patella: The kneecap, protects the knee joint
- Tarsals, Metatarsals, Phalanges: Foot bones that facilitate movement
-
Muscles of the Lower Limb:
- Quadriceps: Located in the front of the thigh, responsible for knee extension
- Hamstrings: Located at the back of the thigh, responsible for knee flexion and hip extension
- Calf muscles: Gastrocnemius and soleus muscles facilitate plantarflexion
- Gluteal muscles: Responsible for hip extension and abduction
-
Joints of the Lower Limb:
- Hip joint: A ball-and-socket joint allowing wide motion
- Knee joint: A hinge joint allowing flexion and extension
- Ankle joint: Includes the tibia, fibula, and talus and enables dorsiflexion and plantarflexion
Deep Vein Thrombosis (DVT)
-
DVT is a blood clot (thrombus) that forms in a deep vein, typically in the legs
-
DVT can cause swelling, pain, and redness
-
A complication of DVT is pulmonary embolism if the clot dislodges and travels to the lungs
-
Risk Factors for DVT:
- Prolonged immobility (long flights, bed rest, sedentary work)
- Medical conditions (heart disease, cancer, obesity, inflammatory disorders)
- Surgical procedures (hips, legs, abdomen)
- Hormonal factors (birth control pills, hormone replacement therapy, pregnancy)
- Age (risk increases with age, particularly over 60)
- Family history: Genetic conditions affecting blood clotting, like factor V Leiden mutation
-
DVT Symptoms:
- Pain or swelling in one leg, calf area
- Redness or warmth in the affected area
- Tenderness when pressing on the leg
- Increased pain with standing or walking
-
DVT Diagnosis:
- Clinical examination: Pain upon dorsiflexion (Homan's sign) may suggest DVT, but it is not specific
- Ultrasound: Common and reliable test to confirm DVT by detecting clots and monitoring blood flow
- D-dimer test: Detects clotting activity. Elevated levels suggest increased clotting, but it is nonspecific
- D-dimer cutoffs are age-adjusted, especially for older patients in Australia
- CT or MRI: Are used in complex cases or when other conditions are suspected
-
DVT Management:
- Anticoagulation therapy: Mainstay treatment to prevent clot extension and reduce embolism risk
- Heparin/enoxaparin: Given initially for rapid anticoagulant effects
- Warfarin: Long-term management to maintain therapeutic INR levels
- Compression stockings: Reduce swelling and prevent post-thrombotic syndrome
- Lifestyle modifications: Weight management, smoking cessation, and increasing physical activity
- Anticoagulation therapy: Mainstay treatment to prevent clot extension and reduce embolism risk
-
DVT Pathogenesis
- Signs and Symptoms:
- Swelling and redness in the affected leg
- Pain, especially with dorsiflexion (positive Homan's sign)
- Warmth over the clot area
- Tenderness and discoloration
- Signs and Symptoms:
-
DVT Pathogenesis - Virchow's Triad:
- Stasis of blood flow: Immobility can cause this
- Endothelial injury: This is worsened by smoking and alcohol
- Hypercoagulability: Obesity and hypertension contribute to increased clotting risk
-
DVT Complications include:
- Pulmonary Embolism (PE): Life-threatening if clot travels to lungs
- Chronic Venous Insufficiency: Long-term vein damage
- Post-thrombotic Syndrome: Persistent leg swelling and pain
-
Large DVTs put patients at risk for PE
Coagulation Cascade
-
The coagulation cascade is a series of biochemical reactions leading to blood clot formation to stop bleeding
-
It has three interconnected pathways:
- Intrinsic Pathway: Triggered by internal damage to blood vessels
- Extrinsic Pathway: Triggered by external trauma
- Common Pathway: Where both pathways converge to form a stable clot
-
The pathways consist of clotting factors that activate each other, ultimately forming a fibrin clot
Intrinsic Pathway (Contact Activation Pathway)
-
Triggered by damage to blood vessel itself (exposed collagen/abnormal endothelium)
-
Takes longer (minutes) for a controlled response
-
Lab test: Activated Partial Thromboplastin Time (aPTT) monitors heparin therapy
-
Intrinsic Pathway Step-by-Step Breakdown:
- Factor XII (Hageman Factor) is activated by contact with collagen or a damaged surface
- Factor XIIa converts Factor XI into Factor XIa
- Factor XIa activates Factor IX into Factor IXa (requires calcium)
- Factor IXa combines with Factor VIIIa and activates Factor X
- Begins the common pathway
-
Key Points: Hemophilia A (Factor VIII deficiency) and Hemophilia B (Factor IX deficiency) affect this pathway
Extrinsic Pathway (Tissue Factor Pathway)
-
Triggered by tissue damage, external trauma, cuts, or surgery
-
Faster than the intrinsic pathway (seconds instead of minutes)
-
Lab test: Prothrombin Time (PT) and INR monitors warfarin therapy
-
Extrinsic Pathway Step-by-Step Breakdown:
- Damaged tissue releases Tissue Factor (TF) (Factor III) into the bloodstream
- Tissue Factor (TF) binds to Factor VII forming a complex
- TF-VIIa complex directly activates Factor X, initiating the common pathway
-
Extrinsic Pathway Key Points: Essential for rapid clot formation in response to trauma
Common Pathway (Final Clot Formation)
-
Triggered when Factor X is activated by either the intrinsic or extrinsic pathway
-
Results in fibrin clot formation
-
Common Pathway - Step-by-Step Breakdown:
- Factor Xa combines with Factor Va and calcium to convert Prothrombin (Factor II) into Thrombin (Factor IIa)
- Thrombin Plays a Critical Role:
- Converts Fibrinogen (Factor I) into Fibrin (Factor Ia): It is the structural component of a clot
- Activates Factor XIII to stabilize fibrin clot by cross-linking fibrin strands
- A stable fibrin mesh forms, trapping platelets and red blood cells and completing clot formation
-
Common Pathway Key Points: It is the final clot formation stage and is regulated by multiple anticoagulant mechanisms
Anticoagulants
- Anticoagulants prevent blood clots from forming or growing larger by interfering with different parts of the coagulation cascade
- Types of Anticoagulants:
- Heparins (Unfractionated Heparin & Low-Molecular-Weight Heparin)
- Vitamin K Antagonists (Warfarin)
- Direct Oral Anticoagulants (DOACs)
- Direct Thrombin Inhibitors (Dabigatran)
- Direct Factor Xa Inhibitors (Rivaroxaban, Apixaban, Edoxaban)
Heparins
-
Mechanism: Enhance the activity of antithrombin III (ATIII), a natural anticoagulant that inhibits Factor Xa and Thrombin (Factor IIa)
-
Heparin Forms:
- Unfractionated Heparin (UFH): Works quickly, used in hospitals for acute conditions, like DVT and PE
- Low-Molecular-Weight Heparin (LMWH): Has a more predictable effect, used for long-term anticoagulation, like enoxaparin and dalteparin
-
Heparin Monitoring: UFH is monitored with aPTT, LMWH doesn’t require monitoring
Warfarin (Vitamin K Antagonist)
-
Mechanism: Inhibits the enzyme Vitamin K Epoxide Reductase (VKOR), which is needed to activate Vitamin K-dependent clotting factors (II, VII, IX, and X)
-
Warfarin takes days to work, so patients often start on heparin while waiting for warfarin to take effect
-
Warfarin Monitoring: Requires regular INR (International Normalized Ratio)
-
Warfarin Key Points: Patients on warfarin should avoid excessive vitamin K-rich foods
Direct Oral Anticoagulants (DOACs)
-
More predictable than warfarin and doesn’t require routine monitoring
-
Lower risk of bleeding compared to warfarin
-
DOACs are now commonly used for DVT in Australia
-
Direct Thrombin (Factor IIa) Inhibitor
- Dabigatran (Pradaxa)
- Mechanism: Directly inhibits thrombin (Factor IIa), preventing the conversion of fibrinogen to fibrin
- Use: Stroke prevention in atrial fibrillation, DVT, and PE
-
Direct Factor Xa Inhibitors
- Examples: Rivaroxaban, Apixaban, Edoxaban
- Mechanism: Directly inhibit Factor Xa, preventing thrombin activation and fibrin clot formation
- Use: Preventing stroke, DVT, and pulmonary embolism
-
DOACs Key Points: Increasingly preferred over warfarin due to high safety profile and ease of use
Comparison of Anticoagulants
- Please see the table generated in the document for a quick comparison.
Conclusion
-
The coagulation cascade is a complex process with intrinsic, extrinsic, and common pathways that form fibrin clots
-
Anticoagulants target different parts of this cascade
-
Warfarin requires INR monitoring, DOACs provide a more convenient alternative
-
Understanding which anticoagulant to use and how to monitor them is essential in treating conditions like DVT, PE, and stroke prevention
Coagulation Cascade Summary
-
Intrinsic Pathway: Activated by blood vessel damage. Involves Factor XII --> Factor X
-
Extrinsic Pathway: Activated by tissue injury and release of tissue factor. Factor VII --> Factor X
-
Common Pathway: Converges on Factor X, which converts prothrombin to thrombin, then fibrinogen to fibrin forming a clot
-
Anticoagulants Target Specific Points:
- Warfarin: Inhibits Vitamin K-dependent clotting factors (II, VII, IX, X)
- Heparin/Enoxaparin: Inhibit Factor Xa and thrombin by potentiating antithrombin III
-
Warfarin requires monitoring of INR and enoxaparin is used for rapid anticoagulation
Anticoagulant Indications
- Prevention of further clot formation and reduce the risk of complications like pulmonary embolism
- Anticoagulants are started to reduce the risk of clot extension and embolization in patients with established DVT
Common Anticoagulants
-
Low molecular weight heparin (LMWH):
- Example Enoxaparin (Clexane)
- Administered subcutaneously and provides immediate anticoagulation
- Typically, this is used before oral therapy
-
Warfarin
- Oral anticoagulant to maintain anticoagulation long-term
- Warfarin requires regular monitoring of the International Normalized Ratio (INR) to ensure it stays within the therapeutic range (2.0-3.0 for DVT)
- bridging therapy with LMWH is required due to slow onset until the INR is therapeutic
-
Direct Oral Anticoagulants (DOACs):
- Examples include Apixaban, rivaroxaban, dabigatran
- Fewer dietary restrictions and do not require regular INR monitoring compared to warfarin
- Used for long-term treatment of DVT
-
INR should be maintained between 2.0 and 3.0 for DVT.
-
Monitoring is essential to ensure appropriate blood clotting.
-
Regular testing is critical, especially when therapy first starts
Adverse Effects
- Bleeding risks are the most serious anticoagulation complication
- Warfarin has numerous drug interactions (e.g., with antibiotics, antifungals, and some foods)
- A rare side effect of LMWH is skin necrosis or heparin-induced thrombocytopenia (HIT)
Patient education
- Injection techniques: Educate patients on how to self-inject subcutaneously if using LMWH
- Warfarin considerations: Inform to avoid foods high in vitamin K to not interfere with warfarin's effectiveness
Pharmacokinetics
- Pharmacokinetics refers to how a drug moves through the body via four key processes:
- Absorption: How the drug enters the bloodstream
- Distribution: How the drug spreads throughout the body
- Metabolism: How the drug is broken down
- Excretion: How the drug is removed from the body
- How long a drug stays active and how effective it is is impacted by each of these processes
Absorption
-
Is the process by which a drug moves from the site of administration to the bloodstream
-
Routes of Drug Administration:
- Oral (PO): Absorbed mainly in the small intestine with slower onset due to digestion/first-pass metabolism
- Intravenous (IV): Immediate effect as it directly enters the bloodstream
- Intramuscular (IM): Absorbed through muscle tissue into the bloodstream
- Subcutaneous (SC): Slower absorption compared to IM but useful for drugs like insulin
- Transdermal: Absorbed through skin for prolonged effect
- Sublingual/Buccal: Absorbed directly into bloodstream by bypassing first-pass metabolism
- Inhalation: Rapid absorption due to lungs large surface area
-
Factors Affecting Absorption:
- Drug solubility: Lipid-soluble drugs cross cell membranes easier
- pH and ionization: Weak acids are better absorbed in the stomach and weak bases are better absorbed in intestines
- Gastric emptying time: Food can slow drug absorption
- First-pass metabolism: Reduces bioavailability when drugs get absorbed by the GI tract
Distribution
-
Is the drug moves from the bloodstream to tissues and organs
-
Factors Affecting Distribution:
- Blood Flow: More drug compared as highly perfused organs (brain, liver, kidneys) receive
- Plasma Protein Binding:
- Drugs can bind to albumin in the blood and prevent them from entering tissues
- Active and can exert only the free drug
- There are strong interactions that protein-bound drugs have with other protein-bound drugs
- Volume of Distribution (Vd):
- Low Vd (stays in the plasma) doesn’t let drugs distribute widely. Example: heparin
- High Vd (distributes into tissues) when lipophilic drugs are in fat/muscle
- Drugs that are small and lipid-soluble can Blood-Brain Barrier (BBB) - cross into the brain
Metabolism (Biotransformation)
-
Is process where the body breaks down drugs into metabolites in the liver
-
Phase I (Modification) - Cytochrome P450 Enzymes:
- CYP oxidize, reduce, or hydrolyze the drug to make it more water-soluble
- An example is codeine being metabolized by CYP2D6 into morphine (active form)
- Drug interactions can affect drug metabolism when some drugs induce or inhibit CYP enzymes
- Inducers increase metabolism and decrease drug levels
- Inhibitors decrease metabolism and increase drug levels
-
Phase II (Conjugation): The drug undergoes conjugation to make it more water-soluble
-
An example is paracetamol undergoing glucuronidation in Phase II
Excretion
-
The process of eliminating drugs and their metabolites typically with the kidneys/urine
-
But also via bile, feces, sweat, saliva, and breath
-
Main Routes of Excretion Kidney function:
- Glomerular Filtration: Only unbound drugs are filtered
- Tubular Secretion: Transports drugs into urine
- Reabsorption: bloodstream to prolong their effect
-
Biliary Excretion: Some may undergo enterohepatic recirculation
-
Volatile drugs (e.g., anesthetics) are exhaled through the lungs
-
Factors Affecting Excretion:
- Kidney function: Reduced renal clearance in kidney disease can lead to drug accumulation
- Urine pH: Acidic urine promotes excretion of weak bases and alkaline urine promotes excretion of weak acids
Pharmacokinetics Summary (see table in original document)
Clinical Importance of Pharmacokinetics
-
Dosing Adjustments: Patients with kidney or liver disease may need lower doses due to impaired metabolism/excretion
-
Drug Interactions:
- CYP450 inhibitors increase drug levels, risk of toxicity
- CYP450 inducers decrease drug levels, risk of therapeutic failure
-
Therapeutic Drug Monitoring (TDM): Drugs with a narrow therapeutic index require carful monitoring of blood levels
-
Optimizing Drug Therapy:
- Knowing half-life helps determine dosing frequency
- Steady-state concentration is reached after 4-5 half-lives in chronic dosing
Drug Action Principles
-
Drugs exert effects by interacting with biological targets, typically proteins (e.g., enzymes, receptors, ion channels)
-
Receptor Binding: Drugs bind to receptors, which can activate (agonists - opioids) or inhibit receptor function (antagonists - beta-blockers)
-
Enzyme Inhibition or Activation: Drugs interact with enzymes by inhibiting (ACE inhibitors) or enhancing their activity
-
Ion Channel Modulation: Drugs affect ion channels (calcium channel blockers)
-
Transporter Modulation: Drugs can inhibit proteins that move molecules across cell membranes
-
Dose-Response Relationship: is critical for Efficacy and Potency
-
Compliance: Is essential with correct dosage, follow-up care and patient education
CYP450 Enzymes
-
The group of enzymes responsible for biotransformation of drugs
-
The CYP450 pathway is responsible for:
- Drug-Drug Interactions: some substrates compete in the same active site
- Drug-Food Interactions: alter metabolism of drug as certain foods affect pathway
- Genetic Variations: Polymorphisms cause a variation in drug pharmacokinetics
-
CYP450 Enzymes (Common)/ Their Role
- CYP3A4: statins, benzodiazepines and chemotherapeutic agents
- CYP2D6: antidepressants, antipsychotics, beta-blockers
- CYP1A2: caffeine, some antipsychotic drugs, and theophylline
Drug Kinetics
- Zero-Order Kinetics: the rate of drug metabolism is constant and independent of the drug concentration (ethanol)
- First-Order Kinetics: rate of drug metabolism is directly proportional to the drug concentration (paracetamol and aspirin)
- Michaelis-Menten Kinetics: Rate of metabolism is Zero order at high concentrations and vice versa (phenytoin)
Load Dose vs Steady State
- Loading Dose is a higher dose of a drug given to to achieve therapeutic levels quickly
- Steady State the rate of drug administration equals the rate of elimination reached after several half-lives
PreTest Probability vs Sensitivity vs Specificity
- Pre-Test Probability: Likelihood a patient has a condition before diagnostic testing. (Wells score)
- Sensitivity: Ability of a test to be true-positive to identify if patients have a certain disease (D-dimer test)
- Specificity: Ability of a test to be true-negative to identify if patients do not have a certain disease
D-dimer test
- elevated levels suggest active clot formation or breakdown
- normal (low) D-dimer makes PE or DVT unlikely
- Elevated D-dimer levels can be seen in other conditions (e.g, liver trauma and etc.)
Warfarin (Coumarin Anticoagulants)
- It may start beside heparin or a LMWH
- The Mechanism of Action is inhibit Vitamin K-dependent
- Indications: DVT prevention and treatment as monitoring is every so often done to determine level -Frequent : The INR must be check if Warfarin and Enoxaparin are taken simultaneously
- Adverse Effects: Bleeding and Interactions
- Patient Counselling: Regular testing needed and intake consistent Vitamin K in vegetables and fruits
Enoxaparin LMWH
- The Mechanism of Action is prevent clot forming
- Administration: subcutaneous for DVT, PE as bridges between medication
- Advantages: predictable
- Adverse Effects and monitoring
Please note
The use and indication of each medication in this summary should be cross reference and compared to local clinical guides to determine current standard of practice
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.