Podcast
Questions and Answers
What is the primary cause of periodontitis?
What is the primary cause of periodontitis?
- Fungal infection
- Nutritional deficiency
- Viral infection
- Bacterial infection (correct)
Which bacterium is most strongly associated with periodontitis?
Which bacterium is most strongly associated with periodontitis?
- Lactobacillus casei
- Porphyromonas gingivalis (correct)
- Streptococcus mutans
- Escherichia coli
What contributes to the complexity and resilience of the periodontal biofilm?
What contributes to the complexity and resilience of the periodontal biofilm?
- Nutrient availability
- Polymicrobial interactions (correct)
- Host immune factors
- Environmental conditions
What role do pro-inflammatory cytokines play in periodontitis?
What role do pro-inflammatory cytokines play in periodontitis?
Which of the following is considered a preventative measure against periodontitis?
Which of the following is considered a preventative measure against periodontitis?
What therapeutic approach involves disrupting the biofilm in periodontitis treatment?
What therapeutic approach involves disrupting the biofilm in periodontitis treatment?
Which of the following bacteria is notably involved in localized aggressive periodontitis?
Which of the following bacteria is notably involved in localized aggressive periodontitis?
What technique can be used for the microbial analysis during periodontitis diagnosis?
What technique can be used for the microbial analysis during periodontitis diagnosis?
Flashcards
Periodontitis Definition
Periodontitis Definition
A chronic inflammatory disease affecting tooth-supporting tissues, caused by pathogenic microorganisms.
Oral Biofilm
Oral Biofilm
Dental plaque that acts as a breeding ground for bacteria.
Porphyromonas gingivalis
Porphyromonas gingivalis
A gram-negative anaerobic bacterium strongly associated with periodontitis.
Tannerella forsythia
Tannerella forsythia
Signup and view all the flashcards
Treponema denticola
Treponema denticola
Signup and view all the flashcards
Aggregatibacter actinomycetemcomitans
Aggregatibacter actinomycetemcomitans
Signup and view all the flashcards
Clinical Manifestations
Clinical Manifestations
Signup and view all the flashcards
Scaling and Root Planing
Scaling and Root Planing
Signup and view all the flashcards
Study Notes
Microbiology in Periodontitis
-
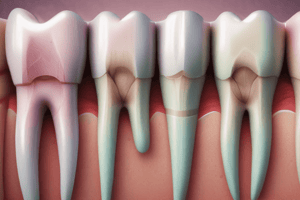
Definition: Periodontitis is a chronic inflammatory disease affecting the tissues supporting the teeth, caused by pathogenic microorganisms.
-
Etiology:
- Bacterial Infection: Primarily caused by a complex interplay of various microorganisms, chiefly bacteria.
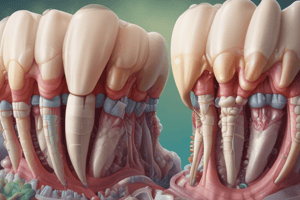
- Oral Biofilm: Formation of a dental biofilm (plaque) as a precursor to periodontal disease.
-
Key Pathogenic Bacteria:
- Porphyromonas gingivalis: Gram-negative, anaerobic; strongly associated with periodontitis.
- Tannerella forsythia: Contributes to the inflammatory response and periodontal tissue destruction.
- Treponema denticola: Spirochete involved in the advanced stages of periodontitis.
- Aggregatibacter actinomycetemcomitans: Notable in localized aggressive periodontitis.
-
Microbial Synergy:
- Pathogenic bacteria often work synergistically to enhance virulence and tissue destruction.
- Polymicrobial interaction leads to increased biofilm complexity and resilience.
-
Immune Response:
- Host immune response to microorganisms results in inflammation.
- Pro-inflammatory cytokines (e.g., IL-1, TNF-α) and enzymes (e.g., matrix metalloproteinases) produced during immune responses contribute to tissue breakdown.
-
Clinical Manifestations:
- Clinical features include gum inflammation (gingivitis), pocket depth increase, attachment loss, and bone resorption.
-
Diagnosis:
- Clinical examination, radiographic analysis, and microbial analysis (e.g., PCR, culture).
- Salivary diagnostics for pathogen detection can be useful.
-
Therapeutic Approaches:
- Mechanical Therapy: Scaling and root planing to disrupt biofilm.
- Antimicrobial Agents: Local or systemic antibiotics targeting specific pathogens.
- Host Modulation: Therapies aimed at altering host response (e.g., overactive inflammatory response).
-
Prevention:
- Good oral hygiene practices to minimize plaque accumulation.
- Regular dental check-ups for early detection and intervention.
-
Research Trends:
- Exploration of the microbiome's role in periodontitis beyond traditional pathogens.
- Development of novel diagnostics and therapeutic strategies targeting microbial communities.
Understanding the microbial dynamics and their interactions in periodontitis is crucial for effective prevention and treatment strategies.
Periodontitis
- A chronic inflammatory disease that affects the tissues supporting the teeth, caused by pathogenic microorganisms
- Primarily caused by a complex interplay of various microorganisms, chiefly bacteria
- Formation of a dental biofilm (plaque) is a precursor to periodontal disease
- Key pathogenic bacteria include:
- Porphyromonas gingivalis: Gram-negative, anaerobic; strongly associated with periodontitis
- Tannerella forsythia: Contributes to the inflammatory response and periodontal tissue destruction
- Treponema denticola: Spirochete involved in the advanced stages of periodontitis
- Aggregatibacter actinomycetemcomitans: Notable in localized aggressive periodontitis
- Pathogenic bacteria work synergistically to enhance virulence and tissue destruction
- Polymicrobial interaction leads to increased biofilm complexity and resilience
- Host immune response to microorganisms results in inflammation
- Pro-inflammatory cytokines (e.g., IL-1, TNF-α) and enzymes (e.g., matrix metalloproteinases) produced during immune responses contribute to tissue breakdown
- Clinical features include gum inflammation (gingivitis), pocket depth increase, attachment loss, and bone resorption
- Diagnosis involves clinical examination, radiographic analysis, and microbial analysis (e.g., PCR, culture)
- Salivary diagnostics for pathogen detection can be helpful
- Therapeutic approaches include:
- Mechanical Therapy: Scaling and root planing to disrupt biofilm
- Antimicrobial Agents: Local and systemic antibiotics targeting specific pathogens
- Host Modulation: Therapies aimed at altering the host response (e.g., overactive inflammatory response)
- Prevention strategies include:
- Good oral hygiene practices to minimize plaque accumulation
- Regular dental check-ups for early detection and intervention
- Research trends focus on:
- Exploration of the microbiome's role in periodontitis beyond traditional pathogens
- Development of novel diagnostics and therapeutic strategies targeting microbial communities
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.