Podcast
Questions and Answers
What is one primary objective of studying upper gastrointestinal tract disorders in this module?
What is one primary objective of studying upper gastrointestinal tract disorders in this module?
- To understand psychological factors associated with eating disorders
- To analyze the surgical interventions for GI disorders
- To learn about the pharmacological treatments for upper GI diseases
- To identify and manage nutritional consequences of various upper GI disorders (correct)
Which condition is included in the discussion of upper gastrointestinal tract disorders?
Which condition is included in the discussion of upper gastrointestinal tract disorders?
- Diverticulitis
- Cholecystitis
- Colorectal cancer
- Peptic ulcers (correct)
What is the significance of understanding dysphagia in relation to nutritional management?
What is the significance of understanding dysphagia in relation to nutritional management?
- It describes how swallowing mechanisms affect nutritional intake. (correct)
- It helps to identify how to increase caloric intake.
- It indicates the need for medical imaging studies.
- It evaluates the effectiveness of medications for GI disorders.
What is a common symptom of gastroparesis?
What is a common symptom of gastroparesis?
Which of the following best describes the nutrition care process (NCP) in the context of upper gastrointestinal disorders?
Which of the following best describes the nutrition care process (NCP) in the context of upper gastrointestinal disorders?
What are the nutritional consequences of esophagitis?
What are the nutritional consequences of esophagitis?
Which of the following terms refers to the condition of food passing too quickly from the stomach to the small intestine?
Which of the following terms refers to the condition of food passing too quickly from the stomach to the small intestine?
Which symptom is NOT typically associated with dyspepsia?
Which symptom is NOT typically associated with dyspepsia?
What is the primary goal of nutrition intervention for individuals with dysphagia?
What is the primary goal of nutrition intervention for individuals with dysphagia?
How should nutritional needs be calculated for patients requiring nutrition intervention?
How should nutritional needs be calculated for patients requiring nutrition intervention?
Which of the following lab works is primarily conducted by a physician during a nutrition assessment?
Which of the following lab works is primarily conducted by a physician during a nutrition assessment?
What is a recommended practice when a patient cannot tolerate a regular diet?
What is a recommended practice when a patient cannot tolerate a regular diet?
What is the role of a Speech and Language Therapist in the context of dysphagia?
What is the role of a Speech and Language Therapist in the context of dysphagia?
What support can be provided to ensure independence in eating for patients with dysphagia?
What support can be provided to ensure independence in eating for patients with dysphagia?
Which of the following reflects a warning sign of swallowing problems?
Which of the following reflects a warning sign of swallowing problems?
What is the purpose of the International Dysphagia Diet Standardisation Initiative (IDDSI) guidelines?
What is the purpose of the International Dysphagia Diet Standardisation Initiative (IDDSI) guidelines?
What is a primary advantage of using Percutaneous Endoscopic Gastrostomy (PEG) over Nasogastric Tube Feeding (NGT)?
What is a primary advantage of using Percutaneous Endoscopic Gastrostomy (PEG) over Nasogastric Tube Feeding (NGT)?
Which nutrient deficiencies should be monitored if whole grains, fruits, and vegetables are not consumed?
Which nutrient deficiencies should be monitored if whole grains, fruits, and vegetables are not consumed?
Which of the following is considered a high-risk food that could cause choking in patients with dysphagia?
Which of the following is considered a high-risk food that could cause choking in patients with dysphagia?
What should be ensured to enhance eating for individuals with dysphagia?
What should be ensured to enhance eating for individuals with dysphagia?
What is a recommended practice for maintaining nutrition monitoring and evaluation?
What is a recommended practice for maintaining nutrition monitoring and evaluation?
Which of the following practices is recommended for improving meal palatability?
Which of the following practices is recommended for improving meal palatability?
What role do food thickeners play in the nutrition of patients with swallowing difficulties?
What role do food thickeners play in the nutrition of patients with swallowing difficulties?
Which dietary change is suggested for improving the control of swallowing?
Which dietary change is suggested for improving the control of swallowing?
What is a bezoar primarily composed of?
What is a bezoar primarily composed of?
Which type of bezoar is composed of vegetable fibers?
Which type of bezoar is composed of vegetable fibers?
What is a common dietary recommendation for a patient with a bezoar?
What is a common dietary recommendation for a patient with a bezoar?
Which of the following is known to contribute to bezoar formation?
Which of the following is known to contribute to bezoar formation?
What type of bezoar is typically made up of hair and food particles?
What type of bezoar is typically made up of hair and food particles?
Which beverage should be limited or avoided by someone suffering from dyspepsia or bezoars?
Which beverage should be limited or avoided by someone suffering from dyspepsia or bezoars?
In treating dyspepsia, what does using a food and symptoms diary help achieve?
In treating dyspepsia, what does using a food and symptoms diary help achieve?
Which of the following is NOT a type of bezoar?
Which of the following is NOT a type of bezoar?
Which gastrointestinal condition is associated with mechanical dysfunction?
Which gastrointestinal condition is associated with mechanical dysfunction?
What is a common result of pancreatic insufficiency?
What is a common result of pancreatic insufficiency?
Which of the following conditions can cause a fear of eating?
Which of the following conditions can cause a fear of eating?
What defines malabsorption in the context of digestive diseases?
What defines malabsorption in the context of digestive diseases?
Which condition is characterized by disaccharidase deficiencies?
Which condition is characterized by disaccharidase deficiencies?
Which of these conditions is NOT classified under malabsorption issues?
Which of these conditions is NOT classified under malabsorption issues?
Cholelithiasis affects which part of the digestive system?
Cholelithiasis affects which part of the digestive system?
Which of the following can be a consequence of irritable bowel syndrome?
Which of the following can be a consequence of irritable bowel syndrome?
Flashcards are hidden until you start studying
Study Notes
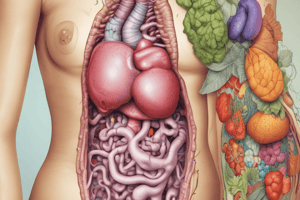
Overview of Medical Nutrition Therapy
- Focuses on digestive and absorptive processes in the GI tract.
- Includes common disorders: GERD, gastric peptic ulcers, dysphagia, and gastroparesis.
- Emphasizes nutritional management and care processes for these conditions.
Learning Objectives
- Understand the digestive processes and normal vs. dysphagic swallowing.
- Recognize causes and symptoms of conditions like esophagitis, gastritis, and dumping syndrome.
- Apply nutrition care process (NCP) steps for managing upper GI tract diseases.
Gastrointestinal Tract Disorders
- Malabsorption Disorders: Celiac disease, Crohn’s disease, pancreatic insufficiency, ulcerative colitis.
- Mechanical Dysfunction: Achalasia, bowel obstructions, esophageal stricture, and tracheoesophageal fistula.
- Fear of Eating Conditions: Dysphagia, bloating, and irritable bowel syndrome, potentially leading to nutritional deficits.
Nutrition Diagnosis and Intervention for Dysphagia
- Assess nutrition based on swallowing problems, weight changes, and diet history.
- Individualized goals: correct deficits, prevent choking, maintain weight, and support eating independence.
- Nutritional needs: 30-35 kcal/kg body weight, 1-1.5g protein/kg for preventing body mass loss.
Food Modifications and Texture Guidelines
- Follow IDDSI guidelines for food and liquid consistency.
- Modified diet may include different textures to accommodate swallowing difficulties.
- Recommended use of enteral nutrition for severe cases, preferring PEG feeding.
Monitoring and Evaluation
- Regularly assess food intake, weight, and oral hygiene.
- Suggestions for suitable food preparation to enhance swallowing safety.
Bezoar Formation
- Bezoars are solid masses of indigestible material causing digestive tract blockages.
- Common types of bezoars:
- Phytobezoars (vegetable fibers)
- Trichobezoars (hair)
- Pharmacobezoars (undissolved medications)
- Lactobezoars (milk proteins)
Nutritional Management of Dyspepsia and Bezoars
- Utilize food diaries to identify food triggers related to symptoms.
- Recommend a soft, low-fat diet, avoiding caffeine and alcohol.
- In cases of obstruction or bezoars, liquid diets may be necessary until resolution.
Overall Importance
- Understanding and addressing upper gastrointestinal disorders is essential for effective nutritional therapy and patient care.
- Tailoring dietary recommendations enhances patient outcomes and quality of life.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.