Podcast
Questions and Answers
Which type of drugs may be used to curb inflammation in the bowel for ulcerative colitis?
Which type of drugs may be used to curb inflammation in the bowel for ulcerative colitis?
- Antibiotics
- Sulfa drugs (correct)
- Corticosteroids (correct)
- Immunosuppressive agents (correct)
What is the main medication used to treat ulcerative colitis?
What is the main medication used to treat ulcerative colitis?
5-aminosalicylic acid
High-fiber diet is recommended for patients with strictures or partial obstruction.
High-fiber diet is recommended for patients with strictures or partial obstruction.
False (B)
___ is recommended to correct fluid and electrolyte losses due to diarrhea.
___ is recommended to correct fluid and electrolyte losses due to diarrhea.
Match the following nutritional complications with their dietary measures:
Match the following nutritional complications with their dietary measures:
What are the typical symptoms experienced by people with Irritable Bowel Syndrome (IBS)?
What are the typical symptoms experienced by people with Irritable Bowel Syndrome (IBS)?
What are the potential causes of Irritable Bowel Syndrome (IBS)?
What are the potential causes of Irritable Bowel Syndrome (IBS)?
Diarrhea is characterized by the passage of frequent, ______ stools.
Diarrhea is characterized by the passage of frequent, ______ stools.
Diarrhea can be classified into osmotic and secretory types.
Diarrhea can be classified into osmotic and secretory types.
What are some potential medical treatments for diarrhea?
What are some potential medical treatments for diarrhea?
What are some potential causes of constipation?
What are some potential causes of constipation?
Flashcards are hidden until you start studying
Study Notes
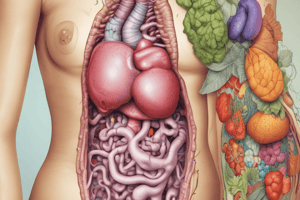
Nutrition Therapy for Lower GIT and Malabsorption Disorders
Disorders of Bowl Function
- Irritable Bowel Syndrome (IBS)
- Characterized by chronic and recurring intestinal symptoms with no specific physical abnormalities
- Symptoms: disturbed defecation, flatulence, abdominal discomfort or pain, sudden change in appearance after a meal, and low-grade intestinal inflammation
- Causes: psychological stress, post-infectious, changes in microflora, idiopathic
- Diagnosis: difficult due to nonspecific symptoms and lack of laboratory tests
- Diarrhea
- Characterized by frequent, watery stools
- Causes: inadequate fluid reabsorption, increased intestinal secretions, osmotic and secretory diarrhea
- Types: osmotic diarrhea (unabsorbed nutrients attract water to the colon), secretory diarrhea (fluid secreted by the intestines exceeds reabsorption)
- Constipation
- Characterized by defecation frequency of fewer than three bowel movements per week
- Symptoms: hard stools, excessive straining during defecation
- Causes: low-fiber diet, low food intake, low fluid intake, low physical activity, medical conditions, neurological conditions, pregnancy, medication side effects
Nutrition Therapy for Disorders of Bowl Function
- Irritable Bowel Syndrome (IBS)
- Dietary adjustments: try and error, peppermint oil, probiotics, psyllium supplementation, gradual increase in fiber intake
- Avoid foods that aggravate symptoms: fried or fatty foods, gas-producing foods, milk
- Diarrhea
- Nutrition care: depends on cause and severity of diarrhea
- Dietary recommendations: low-fat, lactose-free diet, apple pectin or banana flakes to thicken stool consistency
- Avoid foods that exacerbate symptoms: gas-producing foods, caffeine
- Constipation
- Nutrition therapy: gradual increase in fiber intake, adequate fluid intake, adding prunes or prune juice to the diet
- Avoid foods that exacerbate symptoms: low-fiber diet, dairy products, processed foods
Inflammatory Bowel Disease
- Crohn's Disease and Ulcerative Colitis (UC)
- Characterized by chronic inflammatory illnesses with abnormal immune responses to the GI tract
- Causes: autoimmune disease, genetic and environmental factors
- Symptoms: malabsorption, diarrhea, blood in stool, weight loss, fatigue
- Nutrition Therapy for Inflammatory Bowel Disease
- Dietary measures: high-kcalorie, high-protein diet, oral supplements, fat-soluble vitamins and mineral supplements
- Medical treatment: aminosalicylates, corticosteroids, immunomodulators, biologic therapies, surgery
Colostomies and Ileostomies
- Colostomy
- Surgical removal of the rectum and anus
- Stools with high water content
- Nutrition therapy: clear liquids, high-soluble fiber diet, vitamin B12 injections
- Ileostomy
- Surgical removal of the damaged part of the ileum
- Waste material in fluid form
- Nutrition therapy: high-kcalorie, high-protein diet, vitamin B12 injections, extra fluid and electrolyte replacement
Malabsorption Disorders
- Cystic Fibrosis
- Affects the cells that produce mucus, sweat, and digestive juices
- Causes: defective gene
- Complications: lung damage, pancreatic insufficiency, salt losses in sweat
- Nutrition therapy: high-kcalorie, high-protein diet, pancreatic enzyme replacement therapy, liberal use of table salt
- Celiac Disease
- Autoimmune disorder characterized by an abnormal immune response to gluten
- Causes: immune reaction to gluten
- Consequences: damage to intestinal mucosa, malabsorption of nutrients
- Nutrition therapy: gluten-free diet### Malabsorption Disorders
- Lactase deficiency can result from mucosal damage, and milk products may exacerbate gastrointestinal symptoms.
Nutrition Therapy for Celiac Disease
- The treatment for celiac disease involves lifelong adherence to a gluten-free diet.
- Symptoms often improve within several weeks, but mucosal healing can take years.
- If lactase deficiency is suspected, patients should avoid lactose-containing foods until the intestine has recovered.
- A gluten-free diet eliminates foods containing wheat, barley, and rye.
- Patients should be instructed on food preparation methods to prevent cross-contamination from utensils, cutting boards, and toasters.
- Most people with celiac disease can safely consume moderate amounts of oats, but most oats grown in the United States are contaminated with wheat, barley, or rye.
- Some oat manufacturers produce oats in dedicated facilities and test products to ensure they are gluten-free.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.