Podcast
Questions and Answers
What is the purpose of metabolism in living cells?
What is the purpose of metabolism in living cells?
- To facilitate only the absorption of electrolytes.
- To generate energy without chemical reactions.
- To acquire and utilize free energy for cellular functions. (correct)
- To only break down large molecules without creating any.
Which of the following best describes catabolism?
Which of the following best describes catabolism?
- The conversion of energy from sunlight into chemical energy.
- The process of energy storage within cells.
- The breakdown of large molecules into smaller ones. (correct)
- The buildup of complex molecules from simpler ones.
What is the role of anabolism in metabolism?
What is the role of anabolism in metabolism?
- It facilitates the digestive process exclusively.
- It breaks down molecules to release energy.
- It is solely responsible for energy regulation.
- It combines small molecules to form larger ones, consuming energy. (correct)
What are metabolites in the context of metabolism?
What are metabolites in the context of metabolism?
Which pathway is referred to as amphibolism?
Which pathway is referred to as amphibolism?
What is produced during the citric acid cycle (CAC) that is essential for the electron transport chain?
What is produced during the citric acid cycle (CAC) that is essential for the electron transport chain?
What is the end result of catabolism?
What is the end result of catabolism?
During which process are macromolecules converted into small units?
During which process are macromolecules converted into small units?
What enzyme in saliva initiates the digestion of carbohydrates?
What enzyme in saliva initiates the digestion of carbohydrates?
Which part of the digestive system does not contribute to carbohydrate digestion?
Which part of the digestive system does not contribute to carbohydrate digestion?
How is energy captured during the degradation of foodstuffs?
How is energy captured during the degradation of foodstuffs?
Which enzyme is responsible for hydrolyzing lactate into glucose and galactose?
Which enzyme is responsible for hydrolyzing lactate into glucose and galactose?
What role does GluT 2 play in glucose metabolism?
What role does GluT 2 play in glucose metabolism?
Which of the following enzymes in the intestinal juice hydrolyzes terminal α-1→4 glycosidic linkages?
Which of the following enzymes in the intestinal juice hydrolyzes terminal α-1→4 glycosidic linkages?
What type of metabolism is characterized by the entry of reducing equivalents into the electron transport chain?
What type of metabolism is characterized by the entry of reducing equivalents into the electron transport chain?
What are carbohydrates primarily broken down into during digestion?
What are carbohydrates primarily broken down into during digestion?
Which hormone is primarily responsible for lowering blood glucose levels?
Which hormone is primarily responsible for lowering blood glucose levels?
What is the predominant glucocorticoid in humans that raises blood glucose levels?
What is the predominant glucocorticoid in humans that raises blood glucose levels?
Which hormone secreted by the anterior pituitary gland opposes the action of insulin?
Which hormone secreted by the anterior pituitary gland opposes the action of insulin?
What effect do catecholamines have on blood glucose levels?
What effect do catecholamines have on blood glucose levels?
Which condition is NOT a cause of hyperglycemia?
Which condition is NOT a cause of hyperglycemia?
What is a common cause of hypoglycemia related to insulin administration?
What is a common cause of hypoglycemia related to insulin administration?
Which metabolic process does glucagon enhance in the liver during hypoglycemia?
Which metabolic process does glucagon enhance in the liver during hypoglycemia?
What is the normal fasting blood glucose range in mg%?
What is the normal fasting blood glucose range in mg%?
What is the renal threshold for glucose excretion in normal individuals?
What is the renal threshold for glucose excretion in normal individuals?
Which condition describes the presence of sugar in urine?
Which condition describes the presence of sugar in urine?
Which type of diabetes is characterized by absolute insulin deficiency?
Which type of diabetes is characterized by absolute insulin deficiency?
What is the primary cause of Type II Diabetes Mellitus?
What is the primary cause of Type II Diabetes Mellitus?
Under normal dietary conditions, what sugar is primarily present in blood plasma?
Under normal dietary conditions, what sugar is primarily present in blood plasma?
Which of the following describes melituria?
Which of the following describes melituria?
When does glycosuria typically occur?
When does glycosuria typically occur?
Which condition is a secondary cause of diabetes?
Which condition is a secondary cause of diabetes?
What type of glucose transporter is GluT 4 and where is it found?
What type of glucose transporter is GluT 4 and where is it found?
Which monosaccharide has the maximum absorption rate in the intestine?
Which monosaccharide has the maximum absorption rate in the intestine?
How is glucose absorbed using GluT 1 transporter?
How is glucose absorbed using GluT 1 transporter?
What is the main function of GluT 5?
What is the main function of GluT 5?
What mechanism is involved in the absorption of both glucose and galactose?
What mechanism is involved in the absorption of both glucose and galactose?
Which glucose transporter is involved in the uniport system for glucose absorption into the bloodstream?
Which glucose transporter is involved in the uniport system for glucose absorption into the bloodstream?
What characterizes the absorption process of fructose compared to glucose?
What characterizes the absorption process of fructose compared to glucose?
What role does insulin play in glucose absorption?
What role does insulin play in glucose absorption?
Study Notes
Overview of Carbohydrate Metabolism
- Metabolism encompasses all chemical reactions within living cells, acquiring and utilizing free energy.
- Metabolism is categorized as intermediary, involving enzyme-catalyzed reactions that transform metabolites.
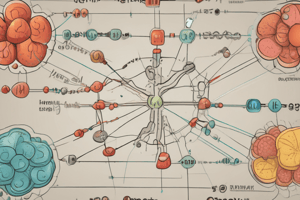
- Metabolic pathways can be classified into catabolic, anabolic, and amphibolic paths.
Metabolic Pathways
- Catabolism: Breakdown of large molecules into smaller ones, releasing energy.
- Anabolism: Formation of large molecules from smaller ones, consuming energy.
- Amphibolism: Involves both breakdown and synthesis processes, acting as a crossroad between catabolic and anabolic pathways.
Stages of Metabolism
- Primary Metabolism: Digestion in the gastrointestinal tract (GIT) reduces macromolecules to smaller units (e.g., proteins to amino acids).
- Secondary Metabolism: Absorption and catabolism occur, with the citric acid cycle generating reducing equivalents like NADH and FADH2.
- Tertiary Metabolism: Reduced equivalents enter the electron transport chain for energy release, referred to as cellular respiration.
Digestion of Carbohydrates
- Carbohydrates include polysaccharides (starch, glycogen) and disaccharides (sucrose, lactose) converting to monosaccharides (glucose, galactose, fructose) via hydrolysis.
- Mouth: Salivary amylase begins carbohydrate digestion.
- Stomach: Limited carbohydrate activity; no carbohydrate-splitting enzymes.
- Duodenum: Pancreatic amylase continues breakdown of polysaccharides.
- Small Intestine: Several enzymes (amylase, lactase, maltase, etc.) liberate free glucose and other monosaccharides.
Transport of Glucose
- GluT 1: Present in numerous tissues, facilitates glucose uptake into most cells.
- GluT 2: Found in intestinal cells and liver, acts as glucose sensor but has low affinity for glucose.
- GluT 3: High-affinity glucose transporter in neurons and brain cells.
- GluT 4: Insulin-mediated transporter in skeletal muscle and adipose tissue.
- GluT 5: Mainly transports fructose in the small intestine.
Absorption Mechanisms
- Only monosaccharides are absorbed; absorption rates: galactose (max), glucose (moderate), fructose (min).
- Passive Diffusion: Dependent on concentration gradients.
- Facilitated Diffusion: Rapid glucose and galactose absorption via sodium-dependent glucose transporter (S GluT-1).
Hormonal Regulation of Carbohydrate Metabolism
- Insulin: Reduces blood glucose levels, promoting uptake in tissues.
- Cortisol: Increases blood glucose levels through gluconeogenesis.
- Growth Hormone and ACTH: Elevate blood glucose, acting against insulin.
- Catecholamines (Epinephrine, Norepinephrine): Stimulate glycogenolysis, increasing blood glucose.
- Glucagon: Released during hypoglycemia, promotes glycogenolysis and gluconeogenesis in the liver.
Blood Sugar Levels
- Normal Fasting Glucose: 60 to 100 mg/dL.
- Hyperglycemia: Elevated blood glucose, causes include diabetes and stress.
- Hypoglycemia: Low blood glucose, causes include insulin overdose and severe exercise.
Glycosuria
- Glucose is typically absent in urine; its presence indicates renal threshold exceeded (170-180 mg/dL).
- Glycosuria occurs when blood glucose exceeds reabsorptive capacity of renal tubules.
Diabetes Mellitus (DM)
- DM is characterized by chronic high blood glucose due to insulin deficiency or insensitivity.
- Types of DM:
- Type I (Juvenile-Onset): Insulin-dependent.
- Type II (Maturity-Onset): Non-insulin dependent, often associated with obesity.
- Causes: Hereditary factors, autoimmune responses (Type I), obesity, and dietary influences.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your understanding of carbohydrate metabolism as taught in MED 302. This quiz covers the normal responses during fed and fasting states, as well as the effects of exercise and diabetes on carbohydrate metabolism. Prepare to assess your knowledge on these critical aspects of medical biochemistry.