Podcast
Questions and Answers
The incidence of TTP is estimated to be between 2 and 10 cases per million people.
The incidence of TTP is estimated to be between 2 and 10 cases per million people.
True (A)
TTP is more common in men than women.
TTP is more common in men than women.
False (B)
Genetic cases of TTP are most commonly observed in adults.
Genetic cases of TTP are most commonly observed in adults.
False (B)
An inhibitory IgG autoantibody is a potential cause of the acquired form of TTP.
An inhibitory IgG autoantibody is a potential cause of the acquired form of TTP.
TTP is characterized by the presence of a pentad of clinical signs and symptoms including anemia and fever.
TTP is characterized by the presence of a pentad of clinical signs and symptoms including anemia and fever.
Flashcards
What is Thrombotic Thrombocytopenic Purpura (TTP)?
What is Thrombotic Thrombocytopenic Purpura (TTP)?
A rare condition affecting blood clotting, with an estimated incidence of 2-10 cases per million people. It's more common in women (about 2/3 of cases).
What is the main cause of the acquired form of TTP?
What is the main cause of the acquired form of TTP?
Inhibitory IgG autoantibody, stimulated by factors like infection, autoimmune diseases, certain drugs, organ transplants, or cardiac surgery.
What is von Willebrand factor (VWF)?
What is von Willebrand factor (VWF)?
A protein that helps platelets stick together and forms blood clots.
What is ADAMTS-13?
What is ADAMTS-13?
Signup and view all the flashcards
What are the five key features of TTP?
What are the five key features of TTP?
Signup and view all the flashcards
Study Notes
Course Information
- Course Title: Clinical Laboratory Sciences, M.Sc. program
- Course Name: Blood Homeostasis and Coagulation
- Course Code: MCLS7211
- Semester: First Semester, 2024/2025
- Lecturer: Dr. Ola Karmi
- Email: [email protected]
Lecture 8: Thrombotic Thrombocytopenic Purpura (TTP) & Hemolytic Uremic Syndrome (HUS)
- TTP: A rare disease with an estimated incidence of 2-10 cases per million in all racial groups.
- Higher frequency in women. Two-thirds of cases are in women.
- Infants & Young Children: Cases with a genetic basis are rare, occurring in 1 in 1 million or less, representing a small portion of TTP (less than 5%).
- High mortality: Mortality rate is high, ranging from 10-20%.
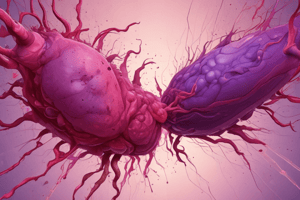
Pathophysiology of TTP
- VWF Secretion: Von Willebrand Factor (VWF) is secreted by endothelial cells initially as ultra-large multimers.
- ADAMTS13 Cleavage: The enzyme ADAMTS13 cleaves VWF, specifically a Tyr-Met bond in the A2 domain of VWF, reducing the size of VWF multimers.
- Ultra-Large Multimers & Platelet Aggregation: Failure of cleavage allows ultra-large VWF multimers to persist in plasma and on endothelial cells, causing the aggregation of platelets, mostly under high shear forces.
Pathology and Pathogenesis of TTP
- Widespread Platelet Thrombi: Widespread formation of platelet thrombi occurs in the microcirculation accompanied by limited endothelial damage and fibrin formation. Abundant VWF is present.
- Microthrombi: Microthrombi are found throughout various organs but are not always grossly detectable.
- Endothelial Cell Activation: Endothelial cells are activated by an unknown triggering event, leading to the secretion of large amounts of ultra-large VWF.
- Intravascular Platelet Aggregation: This large VWF leads to massive intravascular platelet aggregation under high shear stress, causing ischemic organ damage, consumptive thrombocytopenia, and schistocytic anemia.
Pathology and Pathogenesis of TTP (continued)
- Defective VWF Processing: TTP arises due to the defective processing of highly thrombogenic ultra-large VWF molecules secreted in excess by endothelial cells.
- Congenital or Immune Dysfunction: The deficiency or dysfunction of ADAMTS-13, which is a key regulator, can be either congenital or immune-mediated.
Conditions and Diseases Associated with TTP
- Pregnancy and post-partum
- Infections (particularly HIV)
- Drugs (quinine, quinidine, ticlopidine, clopidogrel, cyclosporine, interferon-alpha, statins)
- Chemotherapy (mitomycin, cisplatin, gemcitabine)
- Allogeneic bone marrow transplantation
- Connective tissue disorders (lupus erythematosus, scleroderma)
- Cardiac surgery
Known and Unknown Players Involved in TTP
- ADAMTS13 Deficiency: Severe deficiency of ADAMTS13 is the primary known cause. Acquired cases can involve autoantibodies, and inherited ones are due to gene mutations.
- Predisposing Factors: Female gender, Black ethnicity, HLA-DRB1*11, and obesity are predisposing factors for acquired TTP.
- Precipitating Factors: Conditions increasing plasma VWF levels (inflammation, infections, pregnancy) also play a role.
- Protein Candidates & Cellular Candidates: Potential (unknown) proteins or cells may play a part in TTP pathogenesis (e.g., platelets and endothelial cells).
Congenital vs. Acquired TTP
- Familial TTP: This form is caused by mutations in the ADAMTS-13 gene. Multiple mutations have been reported (more than 50).
- Acquired TTP: Stimulated by infections, autoimmune/connective tissue disorders, specific drugs, stem cell transplantations, or cardiac surgery. IgG autoantibodies are a key mechanism.
Clinical Presentation
- Previous Pentad: Previously, TTP was diagnosed by the presence of five symptoms: fever, microangiopathic hemolytic anemia, thrombocytopenia, neurological deficits, and renal insufficiency.
- Modern Diagnostic Approach: Now, a diagnosis of TTP can be based on the presence of thrombocytopenia and microangiopathic hemolytic anemia alone, along with blood work (blood smear, LDH).
Clinical & Lab Features
- Thrombocytopenia: Low platelet count (usually less than 20 x 109/L) in the acute phase.
- Microangiopathic Hemolytic Anemia: Hemolytic anemia with schistocytes (fragmented red blood cells), lowered Hematocrit (Hct) (<20%), increased indirect bilirubin, low or undetectable haptoglobin, and high LDH (>1000 U/L)
- Neurological Abnormalities: Neurological issues such as focal signs, coma, stroke, and seizures are common
- Renal Failure: Renal failure, hematuria, and proteinuria often occur. Serum creatinine elevation usually is mild.
- Fever: Fever may sometimes but not always be present.
Diagnosis
- ADAMTS13 Activity: Measuring ADAMTS13 activity is crucial. Less than 10% activity highly suggests TTP.
- Anti-ADAMTS13 Antibodies: Presence of antibodies against ADAMTS13 can help to determine if a TTP case is acquired.
- ADAMTS13 Antigen: Assessment of ADAMTS13 antigen levels to determine the presence of functional ADAMTS13.
Management/Treatment
- Plasma Exchange: Frequent plasma exchange is critical to correct thrombocytopenia, while continuing until platelets are above 150,000/µL and LDH is normal.
- Steroids (Adjunctive): Prednisone (1-2 mg/kg per day) can support the treatments.
- Other Therapies: Additional therapies like rituximab may be used for those who don't respond to plasma exchange (e.g., refractory cases, recurrent cases). Considereculizumab in some cases as well.
- Blood Transfusion: Blood transfusion may be considered.
- Platelet Transfusion: Blood platelet transfusions are contraindicated in patients with TTP.
Hemolytic Uremic Syndrome (HUS)
- Definition: HUS is a heterogeneous group of diseases resulting in thrombotic microangiopathy. A common pathology that is accompanied by microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.
- Causes: Shiga toxin-producing Escherichia coli is a common cause. Variants include complement mediated HUS, and other factors and causes.
Diarrhea-related HUS
- Prodomal Symptoms: Bloody diarrhea is a common precursor, occurring 2-14 days prior to the syndrome onset.
- Lab Findings: Serum creatinine and urea may be more elevated than observed in TTP.
- Neurological Symptoms: Neurological symptoms are uncommon, but more emphasis is placed on the renal failure, which is often more severe than in TTP.
Etiology of HUS
- Bacterial infections: Infections by E. coli 0157:H7 or Shigella dysenteriae bacteria can produce exotoxins.
- Endotoxin binding to receptors: Verotoxins bind to specific receptors in glomerular capillary endothelial cells.
- Pathogenesis: This toxin-receptor complex disrupts endothelial cells causing extensive endothelial swelling and massive thrombus formation.
Pathology & Pathogenesis HUS
- Endothelial Cell Damage: Massive injury to endothelial cells (EC) occurs.
- Reduced Deposition of VWF: Less VWF deposition in thrombi compared to TTP.
- VWF Removal: Released VWF binds to platelets, effectively removing it from the circulation.
- ADAMTS13: Levels of ADAMTS-13 are typically normal in this form of HUS.
Natural History HUS
- Self-Limited: Usually self-limiting with no early or late relapses, unlike the tendency in TTP.
- Renal Failure: Renal failure is a prominent feature of HUS, often severe and potentially leading to residual renal failure requiring dialysis or transplantation treatment..
- Mortality: Mortality rates can be elevated in HUS when compared with TTP, but rates vary depending on the etiology.
Lab Findings (HUS)
- Hemolysis Evidence: Decreased Hb and Hct, reticulocytosis, Schistocytes, Leukocytosis (with shift to the left).
- Intravascular Hemolysis Findings: Increased serum bilirubin, decreased haptoglobin, Hb-emia and Hb-uria
- Microangiopathic Findings: Thrombocytopenia, normal to slightly elevated FDPs. PT and APTT are normally normal or only slightly abnormal.
Treatment HUS
- Supportive Therapy: Close observation, electrolytes management, blood transfusions, and addressing fluid imbalances are crucial.
- Plasma Exchange: Usually not recommended in typical HUS except when ADAMTS-13 is deficient, which usually is the cause of atypical HUS.
- Antibiotics: Controversial, as their role and effectiveness vary greatly.
- Vaccination: Vaccination may help to limit the risk of toxins that are induced by infection, which can lead to HUS.
Comparison TTP vs HUS
| Feature | TTP | HUS |
|---|---|---|
| Age of Onset | Adults (20-50) | Children (<5) |
| Hemolytic Anemia | Fragmented RBCs | Fragmented RBCs |
| Renal Dysfunction | Often present but variable | Acute renal failure is prominent |
| Thrombocytopenia | Severe | Severe |
| CNS involvement | Severe CNS syndrome is common | Mild CNS syndrome |
| Fever | Often present | Often present |
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.