Podcast
Questions and Answers
What is the estimated incidence of Thrombotic Thrombocytopenic Purpura (TTP)?
What is the estimated incidence of Thrombotic Thrombocytopenic Purpura (TTP)?
- 2-10 cases per million (correct)
- 100 cases per million
- 1 in 1 million
- 50 cases per million
Which gender is more likely to be diagnosed with TTP?
Which gender is more likely to be diagnosed with TTP?
- Equally likely
- Female (correct)
- Male
- There is no gender difference
What is the typical occurrence of genetically-based TTP cases?
What is the typical occurrence of genetically-based TTP cases?
- Middle-aged individuals
- Infants and young children (correct)
- Adults
- Teenagers
What is the proposed mechanism of TTP development?
What is the proposed mechanism of TTP development?
What role does ADAMTS-13 play in the pathogenesis of TTP?
What role does ADAMTS-13 play in the pathogenesis of TTP?
What is a common characteristic of TTP that typically presents in the acute phase?
What is a common characteristic of TTP that typically presents in the acute phase?
Flashcards
Thrombotic thrombocytopenic purpura (TTP)
Thrombotic thrombocytopenic purpura (TTP)
A rare disorder characterized by abnormally small blood clots forming in small blood vessels, leading to a decrease in platelets and red blood cells.
Acquired TTP
Acquired TTP
A type of TTP that develops due to an autoimmune response. The body produces antibodies that attack a protein involved in breaking down von Willebrand factor (VWF).
von Willebrand factor (VWF)
von Willebrand factor (VWF)
A protein that helps platelets stick together and clotting factors to form blood clots.
ADAMTS-13
ADAMTS-13
Signup and view all the flashcards
Clinical features of TTP
Clinical features of TTP
Signup and view all the flashcards
Haemolytic uraemic syndrome (HUS)
Haemolytic uraemic syndrome (HUS)
Signup and view all the flashcards
Study Notes
Clinical Laboratory Sciences, M.Sc. Program
- Course: MCLS7211
- Topic: Blood Homeostasis and Coagulation
- Semester: 1, 2024/2025
- Lecturer: Dr. Ola Karmi
Thrombotic Thrombocytopenic Purpura (TTP) & Haemolytic Uremic Syndrome (HUS)
-
TTP is a rare disease with estimated incidence of 2-10 cases per million in all racial groups
-
Women are more frequently affected (2/3 of cases)
-
Genetic cases in infants and young children are extremely rare (<5%)
-
High mortality rate: 10-20%
-
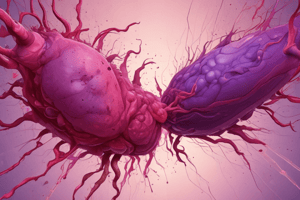
Pathophysiology: von Willebrand Factor (vWF) is secreted from endothelial cells as ultra-large multimers.
-
ADAMTS13 cleaves vWF, preventing large multimer aggregation and platelet aggregation.
-
Lack of ADAMTS13 activity leads to the buildup of ultra-large vWF, causing platelet aggregation, thrombi, and microvascular damage.
-
Pathology and Pathogenesis:
-
Widespread plat thrombi form in the microcirculation with abundant vWF.
-
Microthrombi occur in multiple organs, but large detectable thrombi are rare.
-
Endothelial cells secrete a lot of ultra-large vWF, directly aggregating platelets, especially in high shear conditions
-
This results in massive intravascular platelet aggregation, leading to ischemic organ damage, consumptive thrombocytopenia, and schistocyte anemia.
-
Pathology & Pathogenesis:
-
TTP is caused by defective ultra-large vWF processing, in excess by endothelial cells.
-
The failure of proper clearance leads to the persistence of large vWF multimers and platelet activation, triggering TTP.
-
Genetic or immune-mediated deficiency of ADAMTS13 is a key factor.
-
Conditions associated with TTP:
-
Pregnancy and post-partum
-
Infections (particularly HIV)
-
Drugs (e.g., quinine, quinidine, ticlopidine, clopidogrel, ciclosporine, interferons, statins)
-
Chemotherapy (e.g., mitomycin, cisplatin, gemcitabine)
-
Allogeneic bone marrow transplantation
-
Connective tissue disorders (e.g., lupus erythematosus, scleroderma)
-
Cardiac surgery
-
Causing factors and Predisposing/Precipitating Factors:
-
Severe ADAMTS13 deficiency, either acquired (autoantibodies) orinherited (gene mutations)
-
Female gender, Black ethnicity, HLA-DRB1*11, obesity
-
Conditions increasing vWF levels: inflammation, infections, and pregnancy
Congenital vs. Acquired TTP
- Familial TTP: due to mutations in the ADAMTS-13 gene (>50 reported mutations).
- Acquired TTP: results from inhibitory IgG autoantibodies stimulated by infections, autoimmune/connective tissue diseases, certain drugs, or procedures (e.g., stem cell transplantation or cardiac surgery).
Proposed pathogenesis of TTP
- Healthy vascular endothelium (diagram in the document).
- TTP vascular endothelium (diagram in the document).
- Severe ADAMTS13 deficiency along with other factors like hormonal changes, stress, infections, drugs "second hit."
Interaction between vWF and ADAMTS-13 in plasma
- Showing the normal vWF and ADAMTS13 interplay in the circulation.
Clinical & Lab Features
- TTP often presents with a pentad: thrombocytopenia, microangiopathic hemolytic anemia, neurological abnormalities, renal failure, and fever; sometimes a single sign can be seen.
- Thrombocytopenia, low hematocrit(<20%), schistocytes, elevated lactate dehydrogenase (LDH), low or non-detectable haptoglobin, negative direct Coombs' test,
Natural History
- Variants of TTP, acute sporadic (early relapsing), idiopathic, antibody mediated, chronic recurrent, inherited antibody mediated.
Diagnosis
- Clinical presentation: Previously defined by the pentad, now presence of thrombocytopenia and microangiopathic hemolytic anemia are sufficient to suggest TTP.
- ADAMTS13 activity, Anti-ADAMTS13 antibodies, ADAMTS13 Antigen.
- Complete deficiency of ADAMTS-13 is a key finding leading to TTP and atypical HUS.
Emerging Biomarkers
- Laboratory tests for suspected TTP include a CBC, platelet count, blood smears, coagulation studies, BUN, creatinine, and serum bilirubin and lactate dehydrogenase
Differential Diagnosis
- TTP vs. aHUS(atypical haemolytic uremic syndrome): harder to differentiate, as some symptoms overlap. Usually, patients with aHUS present with more acute and severe renal failure.
- TTP vs. DIC (disseminated intravascular coagulation): DIC is distinguishable by marked elevations in FDPs (fibrin degradation products) and D-dimer, along with hypofibrinogenemia and prolonged PT (prothrombin time) and APTT (activated partial thromboplastin time).
Treatment
- Plasma therapy (plasma exchange) is the cornerstone of current management.
- Steroids.
- Rituximab (for patients with inadequate response to plasma exchange).
- Additional immunomodulators.
- Red blood cell transfusions are needed where necessary.
Haemolytic Uraemic Syndrome (HUS)
- HUS is a heterogeneous group of diseases resulting in thrombotic microangiopathy (TMA).
- TMA is characterized by non-immune microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.
- Common causes include Shiga toxin-producing Escherichia coli (STEC) HUS.
Etiology
- Bacterial infections like E. coli 0157:H7 and Shigella dysenteriae produce exotoxins called verotoxins.
Pathology & Pathogenesis
- Severe endothelial cell injury and decreased vWF deposition,
- vWF is released in excess and binds to platelets
- In HUS, ADAMTS13 activity is normal
Natural History
- Majority of D+HUS cases are self limiting with far less tendency for relapse, compared to TTP.
- Renal failure is often associated with acute D+ HUS.
Lab findings
- Evidence of hemolysis (decreased Hb/Hct, reticulocytosis, schistocytes, leukocytosis)
- Intravascular hemolysis (Hb-emia, Hb-uria, decreased haptoglobin, increased serum bilirubin)
- Thrombotic microangiopathy (thrombocytopenia, normal or slightly elevated FDPs (fibrin degradation products), normal or slightly abnormal PT & APTT)
Diagnosis- suspected TMA
- Clinical findings of TMA (platlet count, serum creatinine)
- Assess ADAMTS13 activity and ADAMTS13 autoantibodies
- Depending on the results, rule out other causes like sepsis, malignancy, DIC.
- Consider other diagnoses like aHUS.
Diarrhea-related HUS
- Characterized by bloody diarrhea preceding the syndrome, oligouria, jaundice, petechial hemorrhage, anemia with schistocytosis.
- Serum creatinine and urea are more abnormal than in TTP.
- Neurological signs are uncommon.
Flowchart for Treatment
- Flowchart for management of adult-onset acquired TTP
Comparison of characteristics associated with HUS & TTP
- TTP vs. HUS
- Age, Symptoms, Renal failure, Treatment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.