Podcast
Questions and Answers
What type of immune response characterizes inflammatory bowel disease?
What type of immune response characterizes inflammatory bowel disease?
- Autoimmune responses to gastrointestinal cells
- Overactive immune responses to gut flora (correct)
- Inadequate immune responses to gut flora
- Allergic responses to dietary substances
Which of the following statements about Crohn disease is true?
Which of the following statements about Crohn disease is true?
- It can involve any area of the gastrointestinal tract. (correct)
- It only involves the mucosal layer of the intestines.
- It exclusively affects the colon.
- It primarily affects the rectum.
At what age does inflammatory bowel disease typically present?
At what age does inflammatory bowel disease typically present?
- During adolescence and early twenties (correct)
- In late adulthood
- During childhood only
- In middle adulthood
Which population is more likely to be affected by inflammatory bowel disease?
Which population is more likely to be affected by inflammatory bowel disease?
What is a possible factor contributing to the pathogenesis of inflammatory bowel disease?
What is a possible factor contributing to the pathogenesis of inflammatory bowel disease?
What is a common clinical feature presented by patients with Crohn's disease?
What is a common clinical feature presented by patients with Crohn's disease?
What can extensive Crohn's disease lead to?
What can extensive Crohn's disease lead to?
Which extraintestinal manifestation is associated with Crohn's disease?
Which extraintestinal manifestation is associated with Crohn's disease?
In which location does ulcerative colitis primarily occur?
In which location does ulcerative colitis primarily occur?
What is a key morphological feature of ulcerative colitis?
What is a key morphological feature of ulcerative colitis?
The tips of the pseudopolyps fuse to form what structure?
The tips of the pseudopolyps fuse to form what structure?
What is a potential complication for patients with long-standing colon involvement in Crohn's disease?
What is a potential complication for patients with long-standing colon involvement in Crohn's disease?
What condition often requires surgical resection in patients with extensive Crohn's disease?
What condition often requires surgical resection in patients with extensive Crohn's disease?
Which type of ulcers are associated with mucosal inflammation in this condition?
Which type of ulcers are associated with mucosal inflammation in this condition?
Which complication is associated with damage to the muscularis propria?
Which complication is associated with damage to the muscularis propria?
What indicates the absence of granulomas in diagnosing Crohn's disease?
What indicates the absence of granulomas in diagnosing Crohn's disease?
What microscopic feature is NOT seen in this condition?
What microscopic feature is NOT seen in this condition?
What is a common presenting symptom in patients with this condition?
What is a common presenting symptom in patients with this condition?
Extra-intestinal manifestations include all of the following EXCEPT:
Extra-intestinal manifestations include all of the following EXCEPT:
What factor increases the risk of colonic adenocarcinoma in this context?
What factor increases the risk of colonic adenocarcinoma in this context?
Which statement regarding the risk of malignancy in IBD is true?
Which statement regarding the risk of malignancy in IBD is true?
What is the consequence of TNF release in a susceptible host regarding mucosal permeability?
What is the consequence of TNF release in a susceptible host regarding mucosal permeability?
Which genetic factor has been linked to Crohn's disease?
Which genetic factor has been linked to Crohn's disease?
In Crohn's disease, helper T cells are primarily polarized to produce which type of cytokines?
In Crohn's disease, helper T cells are primarily polarized to produce which type of cytokines?
What common gastrointestinal locations are primarily affected by Crohn's disease?
What common gastrointestinal locations are primarily affected by Crohn's disease?
What is a characteristic gross feature of Crohn's disease?
What is a characteristic gross feature of Crohn's disease?
Which of the following represents a common microscopic feature seen in Crohn's disease?
Which of the following represents a common microscopic feature seen in Crohn's disease?
What role does microbiota play in managing inflammatory bowel disease (IBD)?
What role does microbiota play in managing inflammatory bowel disease (IBD)?
Which cytokine receptor polymorphisms may play a protective role in Crohn's disease?
Which cytokine receptor polymorphisms may play a protective role in Crohn's disease?
What feature of Crohn's disease may result in a cobblestone appearance in the intestines?
What feature of Crohn's disease may result in a cobblestone appearance in the intestines?
Which feature is NOT associated with ulcerative colitis (UC)?
Which feature is NOT associated with ulcerative colitis (UC)?
Flashcards are hidden until you start studying
Study Notes
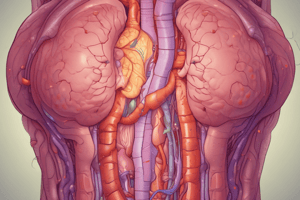
Inflammatory Bowel Disease (IBD)
- IBD is a chronic condition characterized by inappropriate immune responses to normal gut flora.
- It includes two main disorders:
- Ulcerative colitis (UC), which is confined to the colon and rectum, affecting mucosa and submucosa.
- Crohn disease (CD), known for regional enteritis that can impact any part of the gastrointestinal tract, exhibiting transmural involvement.
Epidemiology
- Predominantly observed in developed countries, consistent with the hygiene hypothesis.
- Presents in adolescence and early twenties.
Pathogenesis
-
IBD is idiopathic, resulting from:
- Host interaction defects with gastrointestinal flora.
- Intestinal epithelial barrier dysfunction.
- Aberrant mucosal immune responses leading to increased permeability.
-
Transepithelial microbial flux triggers immune responses, creating a self-amplifying cycle resulting in IBD.
-
Genetic factors include higher disease risk in affected families and a 50% concordance in monozygotic twins for CD.
Genetics and Immune Responses
- NOD2 polymorphisms linked to CD; regulates immune response to luminal microbes.
- Other genes like ATG16L1 and IRGM are involved in microbial recognition.
- CD is associated with polarized TH1 responses, while UC shows TH2 responses.
- IL-23 receptor polymorphisms may provide protection in CD, whereas IL-10 gene polymorphisms are linked to UC.
Epithelial Defects and Microbiota
- Barrier dysfunction due to tight junction defects and transporter gene alterations.
- Microbiota composition influences immune responses; altering gut flora can aid in managing IBD.
Crohn Disease Morphology
- Can appear in any gastrointestinal tract area; most common in the ileum, ileocecal valve, and cecum.
- Typically presents with skip lesions and granular serosa, thickened rubbery bowel wall, and stricture formation.
Gross Features of CD
- Aphthous ulcers and cobblestone appearance due to interspersed mucosa elevation.
- Fistula tracts and granulomas may develop, with granulomas possible in mesenteric lymph nodes.
Clinical Features of CD
- Intermittent attacks include diarrhea, fever, and abdominal pain, with asymptomatic periods lasting weeks or months.
- Extensive CD can lead to malnutrition, iron deficiency, B12 deficiency, and protein-losing enteropathy.
- Surgical resection often needed for complications like fibrotic strictures or fistulas, with recurrence seen in 40% at anastomoses.
- Extraintestinal manifestations may include uveitis, sacroiliitis, and an increased risk of colonic cancer.
Ulcerative Colitis Morphology
- UC affects the colon in a continuous manner from the rectum upward; skip lesions are absent.
- Involves mucosal inflammation with potential backwash ileitis.
Gross Features of UC
- Characterized by reddened, granular mucosa with inflammatory pseudopolyps and extensive ulcers.
- Mucosal damage can lead to toxic megacolon and perforation.
Microscopic Features of UC
- Mucosal inflammation primarily affects the mucosa and submucosa; features include crypt abscesses and glandular distortion.
- Granulomas, skipped lesions, and fissures not present.
Clinical Features of UC
- Patients experience intermittent bloody mucoid diarrhea and abdominal pain with relapses common.
- Extraintestinal manifestations include joint pain, uveitis, and skin lesions; increased risk of colon cancer persists.
Indeterminate Colitis
- 10% of IBD patients cannot be definitively classified between UC and CD.
Colitis Associated Neoplasia
- Risk of malignancy rises 8 to 10 years after onset of IBD, greater in extensive disease.
- Patients require regular surveillance with biopsies for early detection of neoplasia.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.