Podcast
Questions and Answers
What is the effect of decreased sodium chloride concentration on the afferent arterioles?
What is the effect of decreased sodium chloride concentration on the afferent arterioles?
- Decreases resistance to blood flow (correct)
- Decreases glomerular capillary hydrostatic pressure
- Increases resistance to blood flow
- Causes constriction of the arterioles
Which muscle is primarily responsible for bladder contraction during micturition?
Which muscle is primarily responsible for bladder contraction during micturition?
- Internal urethral sphincter
- External urethral sphincter
- Pelvic floor muscles
- Detrusor muscle (correct)
What triggers the micturition reflex to initiate urination?
What triggers the micturition reflex to initiate urination?
- Contraction of the external urethral sphincter
- Increased sodium concentration in the blood
- Stretch receptors in the bladder wall (correct)
- Release of renin from juxtaglomerular cells
During which phase does the internal urethral sphincter remain tense?
During which phase does the internal urethral sphincter remain tense?
What must occur for urination to successfully take place?
What must occur for urination to successfully take place?
What structures are involved in the filtration process of a nephron?
What structures are involved in the filtration process of a nephron?
Which segment of the Loop of Henle primarily consists of simple squamous cells?
Which segment of the Loop of Henle primarily consists of simple squamous cells?
What is the primary function of the distal convoluted tubule (DCT)?
What is the primary function of the distal convoluted tubule (DCT)?
What is the role of juxtaglomerular cells within the juxtaglomerular apparatus?
What is the role of juxtaglomerular cells within the juxtaglomerular apparatus?
Which process involves the movement of substances from renal tubules back into blood plasma?
Which process involves the movement of substances from renal tubules back into blood plasma?
What is the primary function of the kidneys?
What is the primary function of the kidneys?
Which part of the nephron is responsible for the initial filtration of blood?
Which part of the nephron is responsible for the initial filtration of blood?
What does GFR stand for in the context of kidney function?
What does GFR stand for in the context of kidney function?
Which of the following components is part of the renal tubule?
Which of the following components is part of the renal tubule?
What role does the hormone erythropoietin play in the body?
What role does the hormone erythropoietin play in the body?
Which factor is NOT a function of the kidneys?
Which factor is NOT a function of the kidneys?
What is the primary role of the proximal convoluted tubule (PCT)?
What is the primary role of the proximal convoluted tubule (PCT)?
What anatomical feature encloses the glomerulus?
What anatomical feature encloses the glomerulus?
Flashcards
Kidney Function
Kidney Function
The kidney plays a crucial role in maintaining bodily homeostasis by filtering waste products, regulating electrolytes and fluid balance, controlling blood pressure, and contributing to red blood cell production.
Urine Formation Steps
Urine Formation Steps
Urine formation involves three main steps: glomerular filtration, tubular reabsorption, and tubular secretion. Glomerular filtration separates waste products from blood, tubular reabsorption returns useful substances back to the blood, and tubular secretion adds additional waste products to the filtrate.
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
GFR measures the rate at which blood is filtered by the kidneys. It indicates the overall health of the kidneys and their ability to filter waste products.
Glomerular Filtration
Glomerular Filtration
Signup and view all the flashcards
Tubular Reabsorption
Tubular Reabsorption
Signup and view all the flashcards
Tubular Secretion
Tubular Secretion
Signup and view all the flashcards
Factors Affecting Urine Output
Factors Affecting Urine Output
Signup and view all the flashcards
Nephron Structure
Nephron Structure
Signup and view all the flashcards
Loop of Henle
Loop of Henle
Signup and view all the flashcards
Juxtaglomerular Apparatus
Juxtaglomerular Apparatus
Signup and view all the flashcards
Macula Densa Signal
Macula Densa Signal
Signup and view all the flashcards
Afferent Arteriole Vasodilation
Afferent Arteriole Vasodilation
Signup and view all the flashcards
Renin Release
Renin Release
Signup and view all the flashcards
Micturition
Micturition
Signup and view all the flashcards
Detrusor Muscle
Detrusor Muscle
Signup and view all the flashcards
Study Notes
Renal System Overview
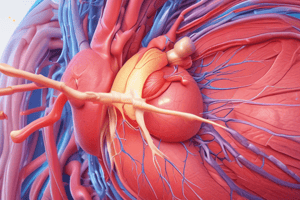
- The kidney is a reddish-brown, bean-shaped organ, approximately 12 centimeters long, enclosed in a tough fibrous capsule.
- Kidneys are located on either side of the vertebral column, behind the peritoneum, against the deep muscles of the back.
- Kidneys perform crucial functions including excretion of waste products and foreign chemicals; regulation of water and electrolyte balances; regulation of body fluid and electrolyte concentrations (Na+, Ca2+, K+, etc.); regulation of arterial blood pressure via the renin-angiotensin system; regulation of acid balance; secretion, metabolism, and excretion of hormones; hemopoietin function (regulation of red blood cell production via erythropoietin); and aiding in vitamin D production.
Kidney Structure
- The kidney has distinct regions:
- Renal cortex
- Renal medulla
- Renal pyramids
- Renal pelvis
- Renal capsule
- Ureter
Nephron
- The nephron is the structural and functional unit of the kidney.
- Each nephron has two components:
- Vascular component
- Tubular component
- Cortical nephrons (80-85%) are more superficial and have a shorter loop of Henle.
- Juxtamedullary nephrons (15-20%) are located closer to the medulla and possess a longer loop of Henle, essential for concentrating urine.
Renal Corpuscle
- The renal corpuscle, the initial filtering unit, is composed of:
- Glomerulus: A network of capillaries
- Bowman's capsule: A cup-shaped structure that encloses the glomerulus
Renal Tubule
- The renal tubule, extending from Bowman's capsule, processes the filtrate:
- Proximal convoluted tubule (PCT): Reabsorbs water and solutes, secretes substances.
- Loop of Henle: A hairpin loop with ascending and descending limbs; crucial for water reabsorption and urine concentration.
- Distal convoluted tubule (DCT): Primarily involved in secretion.
- Collecting ducts: Receive filtrate from DCTs, empty into minor calyces.
Capillary Beds
- Each nephron includes two capillary beds:
- Glomerulus - filters blood
- Peritubular capillaries - reabsorb and secrete substances
Urine Formation
- Urine formation involves three processes:
- Glomerular filtration: Substances move from glomerular capillaries into renal tubules.
- Tubular reabsorption: Useful substances are reabsorbed into the blood.
- Tubular secretion: Additional wastes move from the blood to the filtrate.
Juxta-Glomerular Apparatus
- The juxtaglomerular apparatus (JGA) is a specialized region near the glomerulus in the kidney, regulating glomerular filtration rate (GFR) via:
- Macula densa cells
- Extra glomerular mesengial cells
- Juxtaglomerular cells: Secrete renin.
Micturition
- Micturition is the process of emptying the urinary bladder.
- It is controlled by autonomic and somatic nervous systems.
- The internal urethral sphincter remains tense during storage phase.
- Relaxation of the sphincters and contraction of detrusor muscle cause urination.
- Micturition is initiated by stretch receptors in the bladder wall.
Learning Resources
- Essential textbook for anatomy and physiology is recommended (Marieb En, Human Anatomy and Physiology, 9th Ed.)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.