Podcast
Questions and Answers
What can accumulate at the synapses during hepatic failure?
What can accumulate at the synapses during hepatic failure?
- Phenylethanolamine (correct)
- Adenosine
- Serotonin
- Dopamine
Which of the following is a consequence of cerebral ammonia intoxication?
Which of the following is a consequence of cerebral ammonia intoxication?
- Improved nerve cell membrane action
- Impairment of energy metabolism (correct)
- Increased ATP production
- Enhanced neurotransmitter release
What does NH3 produce in the body that affects neurotransmission?
What does NH3 produce in the body that affects neurotransmission?
- Cortisol
- Urea (correct)
- Acetylcholine
- Serotonin
What is a consequence of the Na+-K+ pump inhibition in nerve cells?
What is a consequence of the Na+-K+ pump inhibition in nerve cells?
What effect does decreased neurotransmitter levels have during systemic shunt formation?
What effect does decreased neurotransmitter levels have during systemic shunt formation?
What is a consequence of liver dysfunction regarding neurotransmitter levels?
What is a consequence of liver dysfunction regarding neurotransmitter levels?
Which amino acids fall under the category of branched chain amino acids (BCAA)?
Which amino acids fall under the category of branched chain amino acids (BCAA)?
What is the normal ratio of BCAA to aromatic amino acids (AAA)?
What is the normal ratio of BCAA to aromatic amino acids (AAA)?
Which enzyme is responsible for converting phenylalanine to tyrosine?
Which enzyme is responsible for converting phenylalanine to tyrosine?
Which neurotransmitter is a product of tyrosine after undergoing hydroxylation?
Which neurotransmitter is a product of tyrosine after undergoing hydroxylation?
High levels of which compound in the blood may indicate severe liver damage?
High levels of which compound in the blood may indicate severe liver damage?
Which of the following compounds is most closely related to sympathomimetic functions?
Which of the following compounds is most closely related to sympathomimetic functions?
What does β-hydroxylase primarily convert?
What does β-hydroxylase primarily convert?
What is an effect of octopamine on the cardiovascular system?
What is an effect of octopamine on the cardiovascular system?
Which neurotransmitter is associated with regulating consciousness and excited impulses?
Which neurotransmitter is associated with regulating consciousness and excited impulses?
What role does the urea cycle play in the body?
What role does the urea cycle play in the body?
What is one major contributor to hyperpolarization in neurons?
What is one major contributor to hyperpolarization in neurons?
Which of the following is NOT a precipitating factor of hepatic encephalopathy (HE)?
Which of the following is NOT a precipitating factor of hepatic encephalopathy (HE)?
Which treatment option is used to reduce plasma ammonia levels in HE?
Which treatment option is used to reduce plasma ammonia levels in HE?
Which amino acid imbalance contributes to hepatic encephalopathy?
Which amino acid imbalance contributes to hepatic encephalopathy?
What is a result of elevated ammonia levels in the body?
What is a result of elevated ammonia levels in the body?
Which of the following metabolites is associated with a foul odor in certain medical conditions?
Which of the following metabolites is associated with a foul odor in certain medical conditions?
What is one of the potential treatments for advanced liver failure?
What is one of the potential treatments for advanced liver failure?
What is a primary consequence of hepatic insufficiency?
What is a primary consequence of hepatic insufficiency?
Which condition is characterized by the disturbance of the central nervous system due to severe liver disease?
Which condition is characterized by the disturbance of the central nervous system due to severe liver disease?
What is one common cause of hyperammonemia in liver dysfunction?
What is one common cause of hyperammonemia in liver dysfunction?
Which grade represents the most serious stage of hepatic encephalopathy?
Which grade represents the most serious stage of hepatic encephalopathy?
What is a clinical feature of hepatorenal syndrome (HRS)?
What is a clinical feature of hepatorenal syndrome (HRS)?
Which of the following is a contributing factor to acute liver failure?
Which of the following is a contributing factor to acute liver failure?
Which hypothesis relates to the pathogenesis of hepatic encephalopathy regarding neurotransmitter levels?
Which hypothesis relates to the pathogenesis of hepatic encephalopathy regarding neurotransmitter levels?
What role does the liver play in digestion?
What role does the liver play in digestion?
What mechanism is primarily involved in the urea cycle in relation to ammonia clearance?
What mechanism is primarily involved in the urea cycle in relation to ammonia clearance?
Which type of hepatic insufficiency is most often associated with morphological changes in liver cells?
Which type of hepatic insufficiency is most often associated with morphological changes in liver cells?
Flashcards
Cerebral Ammonia Intoxication
Cerebral Ammonia Intoxication
A condition where the liver cannot properly filter ammonia from the blood, leading to a buildup of ammonia in the brain.
Impairment of Energy Metabolism in Cerebral Ammonia Intoxication
Impairment of Energy Metabolism in Cerebral Ammonia Intoxication
A key symptom of cerebral ammonia intoxication, caused by a disruption in the energy production process within brain cells.
Neurotransmitter Alteration in Cerebral Ammonia Intoxication
Neurotransmitter Alteration in Cerebral Ammonia Intoxication
The disruption of chemical messengers in the brain due to cerebral ammonia intoxication, influencing communication between brain cells.
Inhibition of Nerve Cell Membrane Action in Cerebral Ammonia Intoxication
Inhibition of Nerve Cell Membrane Action in Cerebral Ammonia Intoxication
Signup and view all the flashcards
Hepatic Failure in Ammonia Toxicity
Hepatic Failure in Ammonia Toxicity
Signup and view all the flashcards
Hepatic Encephalopathy
Hepatic Encephalopathy
Signup and view all the flashcards
Hepatic Insufficiency
Hepatic Insufficiency
Signup and view all the flashcards
Hepatorenal Syndrome (HRS)
Hepatorenal Syndrome (HRS)
Signup and view all the flashcards
Ornithine Cycle
Ornithine Cycle
Signup and view all the flashcards
Hyperammonemia
Hyperammonemia
Signup and view all the flashcards
Ammonia Intoxication
Ammonia Intoxication
Signup and view all the flashcards
Protein Catabolism
Protein Catabolism
Signup and view all the flashcards
Protein Degradation
Protein Degradation
Signup and view all the flashcards
Urea Cycle Enzymes
Urea Cycle Enzymes
Signup and view all the flashcards
Arginine
Arginine
Signup and view all the flashcards
Noradrenaline
Noradrenaline
Signup and view all the flashcards
Dopamine
Dopamine
Signup and view all the flashcards
Octopamine
Octopamine
Signup and view all the flashcards
β-hydroxylase
β-hydroxylase
Signup and view all the flashcards
Monoamine oxidase (MAO)
Monoamine oxidase (MAO)
Signup and view all the flashcards
Neurotransmitter hypothesis of hepatic encephalopathy
Neurotransmitter hypothesis of hepatic encephalopathy
Signup and view all the flashcards
Plasma amino acid hypothesis of hepatic encephalopathy
Plasma amino acid hypothesis of hepatic encephalopathy
Signup and view all the flashcards
Gamma-aminobutyric acid (GABA)
Gamma-aminobutyric acid (GABA)
Signup and view all the flashcards
Branched-chain amino acids (BCAA)
Branched-chain amino acids (BCAA)
Signup and view all the flashcards
Urea Cycle
Urea Cycle
Signup and view all the flashcards
GABA (Gamma-aminobutyric acid)
GABA (Gamma-aminobutyric acid)
Signup and view all the flashcards
Hepatic Encephalopathy (HE)
Hepatic Encephalopathy (HE)
Signup and view all the flashcards
Gastrointestinal bleeding
Gastrointestinal bleeding
Signup and view all the flashcards
Electrolyte and acid-base disorders
Electrolyte and acid-base disorders
Signup and view all the flashcards
Infections
Infections
Signup and view all the flashcards
Treatment of HE
Treatment of HE
Signup and view all the flashcards
Study Notes
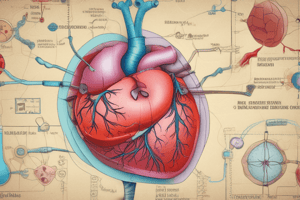
Hepatic Insufficiency
- Hepatic insufficiency is a condition where the liver's ability to function properly is impaired.
- This can result in liver cirrhosis and liver failure.
- Liver failure leads to a buildup of toxins in the blood.
- Conditions like liver cirrhosis can lead to portal hypertension.
Hepatic Encephalopathy
- Hepatic encephalopathy (HE) is a neurological complication associated with advanced liver disease.
- It's caused by toxins building up in the blood due to impaired liver function.
- Symptoms of HE can range from mild confusion to coma.
- GABA and GABA-A levels are elevated in the blood when the liver isn't functioning properly.
Liver Cirrhosis
- Cirrhosis is marked by the replacement of healthy liver tissue with scar tissue, hindering liver function.
- Causes include prolonged alcohol abuse, hepatitis B or C, and non-alcoholic fatty liver disease.
- Portal hypertension results in backup of blood flow through the liver, leading to varices, potentially leading to bleeding, esophageal bleeding, and malnutrition.
- The liver plays a critical role in blood circulation.
Liver Function
- The liver processes toxins and waste products from the blood.
- It produces bile, important for nutrient digestion.
- It plays a key role in metabolism.
Hepatic Failure
- Liver failure occurs when the liver is severely damaged and can no longer perform its essential functions.
- This can lead to toxic build-up in the blood.
- Symptoms vary and can be life-threatening.
Neurological Symptoms of Liver Failure
- Confusion and impaired mental status.
- Altered levels of consciousness ranging from subtle changes to coma.
Gastrointestinal Bleeding Related to Liver Issues
- Enlarged veins or varices in the esophagus, potentially leading to bleeding.
- This is often a consequence of portal hypertension.
- Proper management of bleeding is crucial.
Pathological Processes of Hepatic Insufficiency
- Toxins accumulating in the blood are a crucial aspect of liver failure.
- The liver's inability to process and filter toxic substances can lead to serious complications.
- This damage impacts liver function and blood circulation.
Brain Damage in Hepatic Insufficiency
- Accumulation of toxins in the blood from impaired liver function can directly affect the brain.
- This can cause neurological symptoms.
- GABA and GABA-A levels become elevated in the blood, impacting brain activity.
Other Relevant Information
- Various diagnostic tests are used to assess the condition of the liver and identify underlying causes of the issues.
- Treatment strategies are tailored to the specific cause and severity of the liver condition and target the underlying cause directly.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.