Podcast
Questions and Answers
Which of the following scenarios best exemplifies nociplastic pain?
Which of the following scenarios best exemplifies nociplastic pain?
- A patient experiencing sharp, localized pain after a recent ankle sprain.
- A patient with rheumatoid arthritis experiencing joint pain and inflammation.
- A patient diagnosed with fibromyalgia who reports widespread pain and fatigue without clear evidence of tissue damage or inflammation. (correct)
- A patient with diabetic neuropathy reporting burning sensations in their feet.
A patient reports experiencing persistent orofacial pain for over 6 months following a dental procedure. According to the International Classification of Orofacial Pain (ICOP) 2020, how would this pain be primarily classified?
A patient reports experiencing persistent orofacial pain for over 6 months following a dental procedure. According to the International Classification of Orofacial Pain (ICOP) 2020, how would this pain be primarily classified?
- Neuropathic pain, caused by damage to the trigeminal nerve during the procedure.
- Acute nociceptive pain, directly related to the tissue damage from the procedure.
- Chronic orofacial pain, potentially involving changes in the peripheral or central nervous system. (correct)
- Inflammatory pain, due to an ongoing infection at the surgical site.
Why is orofacial pain considered unique compared to other regional pain classifications?
Why is orofacial pain considered unique compared to other regional pain classifications?
- Orofacial pain is primarily psychological, with minimal physiological impact.
- Orofacial pain exclusively involves nociceptive pathways, unlike other pain types.
- The orofacial region lacks vital structures, making pain management simpler.
- The complex anatomy and concentration of vital structures in the head, face, and neck, along with its impact on critical functions, distinguish orofacial pain. (correct)
Which statement best describes the role of the trigeminal nerve in orofacial pain?
Which statement best describes the role of the trigeminal nerve in orofacial pain?
In the context of orofacial pain, what is the primary purpose of acute pain?
In the context of orofacial pain, what is the primary purpose of acute pain?
A patient presents with chronic headaches and is diagnosed with temporomandibular joint disorder (TMD). According to the mechanistic classification of pain, how would the pain associated with TMD be classified?
A patient presents with chronic headaches and is diagnosed with temporomandibular joint disorder (TMD). According to the mechanistic classification of pain, how would the pain associated with TMD be classified?
How does chronic orofacial pain affect a patient's social function and identity?
How does chronic orofacial pain affect a patient's social function and identity?
A researcher is investigating new treatments for neuropathic pain. Which of the following drug classes would be most appropriate to study, based on the characteristics of neuropathic pain?
A researcher is investigating new treatments for neuropathic pain. Which of the following drug classes would be most appropriate to study, based on the characteristics of neuropathic pain?
Which of the following best illustrates the integration of Axis I and Axis II in orofacial pain management?
Which of the following best illustrates the integration of Axis I and Axis II in orofacial pain management?
A patient presents with persistent orofacial pain, reporting significant anxiety and catastrophizing thoughts related to their condition. How would these psychological factors (Axis II) most likely influence their pain experience?
A patient presents with persistent orofacial pain, reporting significant anxiety and catastrophizing thoughts related to their condition. How would these psychological factors (Axis II) most likely influence their pain experience?
A patient reports a recent onset of orofacial pain accompanied by unexplained sensorimotor neuropathy. Which of the following actions is most appropriate given these red flag symptoms?
A patient reports a recent onset of orofacial pain accompanied by unexplained sensorimotor neuropathy. Which of the following actions is most appropriate given these red flag symptoms?
A patient with chronic orofacial pain reports a history of significant life events and early trauma. How might this history influence their current pain condition, according to the biopsychosocial model?
A patient with chronic orofacial pain reports a history of significant life events and early trauma. How might this history influence their current pain condition, according to the biopsychosocial model?
Which of the following best describes the role of Axis II psychological conditions in the context of orofacial pain?
Which of the following best describes the role of Axis II psychological conditions in the context of orofacial pain?
What is the significance of excluding neoplasia in patients presenting with persistent and unexplained orofacial pain?
What is the significance of excluding neoplasia in patients presenting with persistent and unexplained orofacial pain?
A patient presents with symptoms suggestive of sialadenitis. Under which axis of the ICOP 2020 classification system would this condition primarily be categorized?
A patient presents with symptoms suggestive of sialadenitis. Under which axis of the ICOP 2020 classification system would this condition primarily be categorized?
Which of the following is NOT typically considered a 'red flag' symptom in the assessment of orofacial pain?
Which of the following is NOT typically considered a 'red flag' symptom in the assessment of orofacial pain?
A patient is diagnosed with a somatoform disorder contributing to their chronic orofacial pain. Which aspect of their condition would be the primary target for psychological intervention?
A patient is diagnosed with a somatoform disorder contributing to their chronic orofacial pain. Which aspect of their condition would be the primary target for psychological intervention?
Following ICOP 2020 guidelines, what is the most critical step after identifying 'red flag' symptoms during an orofacial pain assessment?
Following ICOP 2020 guidelines, what is the most critical step after identifying 'red flag' symptoms during an orofacial pain assessment?
A patient reports a sudden, intense, unilateral facial pain triggered by light touch and localized along the V2 distribution. Which condition is MOST likely?
A patient reports a sudden, intense, unilateral facial pain triggered by light touch and localized along the V2 distribution. Which condition is MOST likely?
A patient presents with constant burning pain in the anterior tongue with no visible lesions. She is a 60-year-old female, post-menopausal, and reports increased stress. Which condition is MOST likely?
A patient presents with constant burning pain in the anterior tongue with no visible lesions. She is a 60-year-old female, post-menopausal, and reports increased stress. Which condition is MOST likely?
A patient reports a headache characterized by unilateral, throbbing pain, accompanied by nausea and sensitivity to light. Which type of orofacial pain is MOST likely?
A patient reports a headache characterized by unilateral, throbbing pain, accompanied by nausea and sensitivity to light. Which type of orofacial pain is MOST likely?
Following a dental implant procedure, a patient experiences persistent burning pain, allodynia, and altered sensation in the affected area. What is the MOST likely cause of this pain?
Following a dental implant procedure, a patient experiences persistent burning pain, allodynia, and altered sensation in the affected area. What is the MOST likely cause of this pain?
An elderly patient presents with persistent pain following a shingles outbreak affecting the ophthalmic branch distribution. Which condition is MOST likely?
An elderly patient presents with persistent pain following a shingles outbreak affecting the ophthalmic branch distribution. Which condition is MOST likely?
A patient describes experiencing 'cold allodynia' after a dental procedure. What specific type of acute orofacial pain is the patient experiencing?
A patient describes experiencing 'cold allodynia' after a dental procedure. What specific type of acute orofacial pain is the patient experiencing?
A dentist suspects a patient's toothache is mimicking trigeminal neuralgia. What clinical presentation would MOST strongly suggest this?
A dentist suspects a patient's toothache is mimicking trigeminal neuralgia. What clinical presentation would MOST strongly suggest this?
A patient presents with chronic facial pain that has lasted over 6 months. The pain is non-responsive to typical treatments and does not follow any specific anatomical boundaries. What is the MOST likely diagnosis?
A patient presents with chronic facial pain that has lasted over 6 months. The pain is non-responsive to typical treatments and does not follow any specific anatomical boundaries. What is the MOST likely diagnosis?
What is the PRIMARY clinical feature differentiating secondary trigeminal neuralgia from idiopathic trigeminal neuralgia?
What is the PRIMARY clinical feature differentiating secondary trigeminal neuralgia from idiopathic trigeminal neuralgia?
A patient who has been diagnosed with neuropathic pain is likely to exhibit which of the following pain characteristics?
A patient who has been diagnosed with neuropathic pain is likely to exhibit which of the following pain characteristics?
Which factor is MOST critical in distinguishing articular pain from myogenous pain in the orofacial region?
Which factor is MOST critical in distinguishing articular pain from myogenous pain in the orofacial region?
Axis I of orofacial pain diagnosis primarily focuses on identifying:
Axis I of orofacial pain diagnosis primarily focuses on identifying:
Why is accurate diagnosis crucial in cases of acute dental pain?
Why is accurate diagnosis crucial in cases of acute dental pain?
Which of the following conditions included in the content is classified as nociplastic pain?
Which of the following conditions included in the content is classified as nociplastic pain?
In managing post-herpetic neuralgia affecting the trigeminal system, what early intervention is MOST critical to improve patient outcomes?
In managing post-herpetic neuralgia affecting the trigeminal system, what early intervention is MOST critical to improve patient outcomes?
Flashcards
Acute Pain
Acute Pain
Pain lasting less than 3 months, often from an injury.
Nociceptive Pain
Nociceptive Pain
Pain from tissue damage; responds to NSAIDs and opioids.
Inflammatory Pain
Inflammatory Pain
Pain due to tissue inflammation; often short-lived.
Neuropathic Pain
Neuropathic Pain
Signup and view all the flashcards
Nociplastic Pain
Nociplastic Pain
Signup and view all the flashcards
Orofacial Pain
Orofacial Pain
Signup and view all the flashcards
Orofacial Pain: Complex Region
Orofacial Pain: Complex Region
Signup and view all the flashcards
ICOP 2020
ICOP 2020
Signup and view all the flashcards
Visceral Orofacial Pain
Visceral Orofacial Pain
Signup and view all the flashcards
Neural Orofacial Pain
Neural Orofacial Pain
Signup and view all the flashcards
Axis II: Psychological Conditions
Axis II: Psychological Conditions
Signup and view all the flashcards
Anxiety Disorders (Axis II)
Anxiety Disorders (Axis II)
Signup and view all the flashcards
Mood Disorders (Axis II)
Mood Disorders (Axis II)
Signup and view all the flashcards
Somatoform Disorders (Axis II)
Somatoform Disorders (Axis II)
Signup and view all the flashcards
Psychological Factors Affecting Medical Condition (Axis II)
Psychological Factors Affecting Medical Condition (Axis II)
Signup and view all the flashcards
Axis I and II Integration
Axis I and II Integration
Signup and view all the flashcards
Holistic Pain Assessment
Holistic Pain Assessment
Signup and view all the flashcards
Red Flags in Orofacial Pain
Red Flags in Orofacial Pain
Signup and view all the flashcards
Myogenous Pain
Myogenous Pain
Signup and view all the flashcards
Articular Pain
Articular Pain
Signup and view all the flashcards
Neurovascular Pain
Neurovascular Pain
Signup and view all the flashcards
Dental Pain
Dental Pain
Signup and view all the flashcards
Protective Pain
Protective Pain
Signup and view all the flashcards
Burning Mouth Syndrome
Burning Mouth Syndrome
Signup and view all the flashcards
Persistent Idiopathic Facial Pain
Persistent Idiopathic Facial Pain
Signup and view all the flashcards
Trigeminal Neuralgia
Trigeminal Neuralgia
Signup and view all the flashcards
Post-Traumatic Neuropathic Pain
Post-Traumatic Neuropathic Pain
Signup and view all the flashcards
Post-Herpetic Neuralgia
Post-Herpetic Neuralgia
Signup and view all the flashcards
Migraine
Migraine
Signup and view all the flashcards
Cluster Headaches
Cluster Headaches
Signup and view all the flashcards
Study Notes
Key Classifications of Pain
- Pain can be classified temporally, mechanistically, and regionally.
Temporal Classification
- Acute pain lasts for less than 3 months.
- Acute pain can result from injury combined with unresolved tissue healing.
- Arthritis and fibromyalgia are examples of conditions causing acute pain.
Mechanistic Classification
- Nociceptive pain is a healthy feeling pain caused by tissue damage.
- Nociceptive pain responds to NSAIDs and opioids and examples are acute injury and post-surgical pain.
- Inflammatory pain is a healthy pain that is associated with tissue inflammation.
- Inflammatory pain is often short-lived, unless related to chronic conditions, such as rheumatoid arthritis or infections.
- Neuropathic pain results from lesions or diseases affecting the somatosensory nervous system.
- Neuropathic pain responds poorly to traditional painkillers, but may improve with neuroactive drugs.
- Trigeminal neuralgia and diabetic neuropathy are examples of neuropathic pain conditions.
- Nociplastic pain is dysfunctional central pain without clear damage or inflammation.
- Fibromyalgia and irritable bowel syndrome are examples of nociplastic pain conditions.
Regional Classification
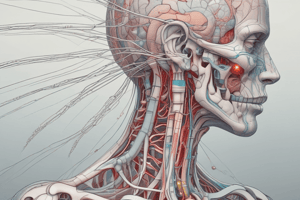
- Orofacial pain is unique due to the complex anatomy of the head, face, and neck.
- Orofacial pain involves the trigeminal nerve, which is responsible for sensory input from the face.
- Acute orofacial pain is a protective reflex that stops us damaging ourselves.
- Increased sensitivity from swelling helps remind us to protect the region from unnecessary movement and further trauma, thereby helping maximise healing capacity.
- Chronic orofacial pain is largely due to subtle changes in the peripheral and central nervous system, meaning pain-sensing nerves (nociceptors) process normal and painful information differently.
- Headaches, temporomandibular joint disorders (TMDs), and dental pain are examples of orofacial pain conditions.
Orofacial Pain: Unique Characteristics
- The orofacial region contains vital structures, including the eyes, mouth, ears, nose, and brain.
- Functions such as breathing, eating, speaking, sleeping, and communication all occur in the orofacial region.
- Damage to the orofacial region can lead to severe psychological and physiological consequences.
- Loss of social function and identity can occur as a result of orofacial pain.
- Chronic orofacial pain can be debilitating, causing emotional distress and social isolation.
International Classification of Orofacial Pain (ICOP) 2020
- ICOP 2020 provides a structured classification for both acute and chronic orofacial pain.
- Seven pain categories exist within ICOP 2020.
- Nociceptive pain includes pulpitis, gingival pain, and mucosal pain.
- Myogenous pain is muscle-based pain, such as temporalis and masseter involvement.
- Articular pain is joint pain, such as TMJ disorders.
- Neuropathic pain includes trigeminal neuralgia and post-traumatic neuropathy.
- Neurovascular pain includes headache-related facial pain, such as migraines and cluster headaches.
- Nociplastic pain is chronic, non-specific pain, such as burning mouth syndrome.
- Psychological aspects highlights the impact of psychosocial factors.
Acute Orofacial Pain
- Dental pain is the most common type of acute orofacial pain.
- Dental pain progresses through reversible pulpitis to irreversible pulpitis and abscess formation.
- Misdiagnosis of dental pain can lead to unnecessary treatments.
- Protective pain alerts the brain to potential harm.
- Cold allodynia and mechanical allodynia from cracked teeth or exposed dentine are examples of protective pain.
Chronic Orofacial Pain
- Burning Mouth Syndrome (BMS) has a spontaneous onset in women >50 years.
- Symptons of BMS: Burning pain in the tongue, lips, or mucosa with no visible cause.
- BMS is often linked to psychological factors and systemic issues, e.g., menopause or diabetes.
- Persistent Idiopathic Facial Pain (PIFP) is chronic pain that lasts for >6 months.
- PIFP is non-responsive to treatments and is not confined to anatomical boundaries.
- PIFP is often associated with psychosocial stressors.
- PIFP is constant and lasts greater than 6 months.
- PIFP is "pain all the time resistant to interventions usually greater than 3 years."
Neuropathic Pain in Orofacial Region
- Trigeminal Neuralgia involves sudden, unilateral pain in the distribution of the trigeminal nerve (V2/V3 regions).
- Trigeminal Neuralgia triggers: Brushing teeth, shaving, talking, or eating.
- Trigeminal Neuralgia pain lasts for seconds, and can have periods of being pain free.
- Associated Trigeminal Neuralgia factors: trigger areas and weight loss.
- Trigeminal Neuralgia is managed with Carbamazepine or surgical options for refractory cases.
- Secondary TN is caused by multiple sclerosis, stroke, vasculitis etc.
- Idiopathic TN is not secondary and has No NVC.
- Post-Traumatic Neuropathic Pain (PTNP) is caused by dental procedures like third molar surgery, implants, or endodontics.
- Burning pain, allodynia (pain from normally non-painful stimuli, like light touch), and altered sensation are features of PTNP.
- Prompt intervention for nerve injuries is required to improve PTNP outcomes.
- Post-Herpetic Neuralgia is persistent pain after herpes zoster infection (shingles).
- Post-Herpetic Neuralgia is common in elderly or immunocompromised patients.
- In trigeminal system Post-Herpetic Neuralgia is most commonly V1 and V2.
- Early treatment for Post-Herpetic Neuralgia involves high-dose antifungals: acyclovir and prednisone.
Features of Neuropathic Pain
- Multiple injuries or episodes of infection and pain.
- Non-responsive to anti-inflammatory pain killers (NSAIDs and Paracetamol).
- Pain is better in the mornings but worsens during the day.
- Pain does not disturb sleep.
- Pain presentation consists of constant burning, elicited neuralgic, or a combination of the two.
- Pain worsens with stress, tiredness, and illness.
Neurovascular Pain
- Migraine presents as unilateral, throbbing pain often associated with aura, nausea, and photophobia.
- Cluster headaches present as severe, episodic pain around the eye or temple.
- Cluster headaches are more common in males and often misdiagnosed as toothache.
- Tension-Type Headaches present as bilateral, dull pain with possible links to medication overuse.
Pain Mechanisms in Dentistry
- Toothache mimics neuralgia when involving dentine or pulp exposure.
- TMJ Disorders include myogenous and arthralgia-related pain.
- TMJ Disorders may mimic migraines or cluster headaches.
Psychological and Psychosocial Factors
Axis I: Physical Conditions
- Axis I focuses on physical conditions responsible for initiating nociceptive impulses.
- These conditions are classified based on the specific orofacial structures involved in generating pain.
- Cutaneous and Mucogingival Pains originate from the skin and gingival (gum) tissues.
- Gingivitis, localized infections, and trauma to gingival tissues are examples of Cutaneous and Mucogingival Pains.
- Mucosal Pains of the Pharynx, Nose, and Paranasal Sinuses are linked to mucosal tissues in the upper respiratory tract.
- Sinusitis, pharyngitis, and nasal infections are examples of Mucosal Pains of the Pharynx, Nose, and Paranasal Sinuses.
- Pains of Dental Origin are caused by dental structures.
- Pulpitis, periapical abscess, and cracked tooth syndrome are examples of Pains of Dental Origin.
- Pains of the Musculoskeletal Structures of the Mouth and Face involve muscles, joints, and related tissues.
- Temporomandibular joint disorders (TMD) and myofascial pain are examples of Pains of the Musculoskeletal Structures of the Mouth and Face.
- Pains of the Visceral Structures of the Mouth and Face arise from deeper structures such as salivary glands.
- Sialadenitis (salivary gland inflammation) and oropharyngeal infections are examples of Pains of the Visceral Structures of the Mouth and Face.
- Pains of the Neural Structures of the Mouth and Face are linked to nerve damage or dysfunction in the orofacial region.
- Trigeminal neuralgia and post-traumatic neuropathy are examples of Pains of the Neural Structures of the Mouth and Face.
Axis II: Psychological Conditions
- Axis II addresses psychological conditions that either directly produce or significantly influence the pain experience.
- These conditions impact how patients perceive, respond to, and manage pain.
- Anxiety Disorders involve excessive worry and fear that can amplify pain perception.
- Generalized anxiety disorder and panic disorder are examples of Anxiety Disorders..
- Mood Disorders involve emotional disturbances that can exacerbate pain sensitivity.
- Depression and bipolar disorder are Mood Disorders.
- Somatoform Disorders are psychological conditions presenting as physical symptoms with no identifiable medical cause.
- Somatization disorder and conversion disorder are Somatoform Disorders.
- Other Psychological Factors Affecting a Medical Condition are mental health issues that influence the onset, severity, or progression of physical pain.
- Post-traumatic stress disorder (PTSD) and health-related anxiety are examples of Other Psychological Factors Affecting a Medical Condition.
- Effective pain management requires addressing both physical (Axis I) and psychological (Axis II) components.
- For example, treating dental pain (Axis I) may require concurrent anxiety management (Axis II) for optimal patient outcomes.
- A comprehensive evaluation should include both physical examination and psychosocial history to ensure all contributing factors are identified and managed.
- Treatment must target the underlying physical pathology while considering the psychological state to enhance recovery and prevent chronic pain conditions.
- Anxiety, depression, and catastrophizing influence pain perception and chronicity.
- Significant life events and early trauma can predispose individuals to chronic pain.
- A holistic assessment of the patient is crucial.
- Ensure neoplasia is excluded in persistent, unexplained pain.
Red Flags in Orofacial Pain
- Recent onset or rapid progression.
- Unexplained sensorimotor neuropathy.
- Persistent painless ulcers or lymphadenopathy.
- Unresponsiveness to conventional treatments.
- Associated systemic symptoms such as weight loss, night fevers, or anemia.
Conclusion
- Pain is a complex experience involving physiological and psychological factors.
- Accurate diagnosis requires a thorough history and structured assessment.
- ICOP 2020 provides a foundation for consistent classification and management of orofacial pain.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.