Podcast
Questions and Answers
Which of the following best describes the role of neuroplasticity in patient recovery?
Which of the following best describes the role of neuroplasticity in patient recovery?
- It is only effective in young patients.
- It involves the brain's ability to reorganize itself by forming new neural connections. (correct)
- It slows down the rehabilitation process.
- It can only occur in the presence of physical interventions.
What does the FIM instrument measure?
What does the FIM instrument measure?
- Cognitive recovery in stroke patients.
- Levels of assistance required for daily living activities. (correct)
- Neurological progress in patients with PD.
- Quality of life after rehabilitation.
During the cognitive stage of motor learning, which characteristic is most evident?
During the cognitive stage of motor learning, which characteristic is most evident?
- Performance without the need for feedback.
- Consistent performance with minimal errors.
- High levels of error and variable performance. (correct)
- Automatic execution of tasks.
In Constraint Induced Movement Therapy (CIMT), what is one key component of the intervention?
In Constraint Induced Movement Therapy (CIMT), what is one key component of the intervention?
Which of the following outcome measures is specifically used to evaluate gait speed?
Which of the following outcome measures is specifically used to evaluate gait speed?
What is a critical feature of the Burke Lateropulsion Scale?
What is a critical feature of the Burke Lateropulsion Scale?
What is one of the principles of LSVT (Lee Silverman Voice Treatment)?
What is one of the principles of LSVT (Lee Silverman Voice Treatment)?
When writing a SMART goal, which component is essential for ensuring clarity and measurability?
When writing a SMART goal, which component is essential for ensuring clarity and measurability?
What is the main purpose of using the CARES Tool in patient assessment?
What is the main purpose of using the CARES Tool in patient assessment?
Which approach involves adapting activities to enhance patient participation despite limitations?
Which approach involves adapting activities to enhance patient participation despite limitations?
In what stage of motor learning do individuals primarily focus on refining their skills and increasing efficiency?
In what stage of motor learning do individuals primarily focus on refining their skills and increasing efficiency?
What is an essential part of the SMART goal framework for healthcare professionals?
What is an essential part of the SMART goal framework for healthcare professionals?
What aspect of neuroplasticity does the LSVT method primarily target during treatment?
What aspect of neuroplasticity does the LSVT method primarily target during treatment?
Which of the following is NOT a characteristic of the Fugl Meyer Assessment for stroke recovery?
Which of the following is NOT a characteristic of the Fugl Meyer Assessment for stroke recovery?
Which exercise intervention is considered beneficial for enhancing postural control in patients with Parkinson's Disease?
Which exercise intervention is considered beneficial for enhancing postural control in patients with Parkinson's Disease?
What is a primary criterion for inclusion in a Constraint Induced Movement Therapy (CIMT) program?
What is a primary criterion for inclusion in a Constraint Induced Movement Therapy (CIMT) program?
Which of the following outcome measures is specifically designed for evaluating clinical gait speed?
Which of the following outcome measures is specifically designed for evaluating clinical gait speed?
Which statement accurately describes the function of the Burke Lateropulsion Scale?
Which statement accurately describes the function of the Burke Lateropulsion Scale?
Which approach focuses on enhancing the patient’s existing abilities while promoting recovery through structured exercises?
Which approach focuses on enhancing the patient’s existing abilities while promoting recovery through structured exercises?
In the context of outcome measures, which tool specifically assesses balance and gait in patients with neurologic conditions?
In the context of outcome measures, which tool specifically assesses balance and gait in patients with neurologic conditions?
Which of the following statements best describes the characteristics of the associative stage of motor learning?
Which of the following statements best describes the characteristics of the associative stage of motor learning?
Which intervention is primarily used to promote postural control in patients with Parkinson's Disease?
Which intervention is primarily used to promote postural control in patients with Parkinson's Disease?
Which features differentiate the Burke Lateropulsion Scale from the Scale for Contraversive Pushing?
Which features differentiate the Burke Lateropulsion Scale from the Scale for Contraversive Pushing?
During the facilitation of neuroplasticity, which characteristic is most crucial in LSVT?
During the facilitation of neuroplasticity, which characteristic is most crucial in LSVT?
In evaluating a patient’s performance during the stages of motor learning, which characteristic is typical of the cognitive phase?
In evaluating a patient’s performance during the stages of motor learning, which characteristic is typical of the cognitive phase?
What is the purpose of incorporating SMART goals in the therapy plan?
What is the purpose of incorporating SMART goals in the therapy plan?
Which of the following outcome measures is best suited for assessing functional mobility over an extended distance?
Which of the following outcome measures is best suited for assessing functional mobility over an extended distance?
Which intervention is appropriate for managing symptoms of freezing and festination in Parkinson's Disease?
Which intervention is appropriate for managing symptoms of freezing and festination in Parkinson's Disease?
Flashcards are hidden until you start studying
Study Notes
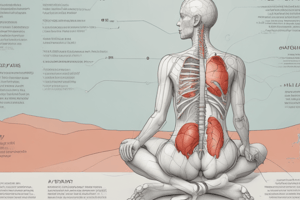
Introduction to Clinical Reasoning
- ICF Framework: This framework outlines the components of a patient's health and disability, including body functions, activities, and participation.
- Neuroplasticity: The brain's ability to adapt and change in response to experiences, injuries, or training.
- Characteristics Ideal For Recovery: Neuroplasticity is enhanced by:
- Intensity of training
- Repetition of tasks
- Specificity of training to targeted tasks
- Timing of interventions after injury or illness
- Motivation and engagement
- Treatment Frameworks:
- Restorative: Aiming at restoring lost function through strengthening, stretching, and retraining.
- Augmented: Using assistive devices or technology to support and enhance function.
- Compensatory: Adapting to limitations by teaching new strategies or skills for managing tasks.
- Stages of Motor Learning:
- Cognitive Stage: Learning new movements and understanding the task.
- Associative Stage: Refining the movement and becoming more consistent.
- Autonomous Stage: Performing the movement automatically and efficiently.
- Roles and Responsibilities:
- Physical Therapists: Design and implement treatment plans, provide skilled interventions.
- Physical Therapist Assistants (PTAs): Assist with treatments under the supervision of a PT.
- Aides: Provide support with activities of daily living (ADLs) and tasks under the guidance of a PT or PTA.
Goal Writing and Outcome Measures
- Components of FIM: (Functional Independence Measure) Measures an individual's ability to perform ADLs.
- Levels of Assistance:
- Total Assistance: Requires 100% help from another person to perform the task.
- Maximum Assistance: Requires 75% help from another person to perform the task.
- Moderate Assistance: Requires 50% help from another person to perform the task.
- Minimal Assistance: Requires 25% help from another person to perform the task.
- Supervision: Needs verbal cues or supervision to perform the task.
- Modified Independence: Requires an assistive device or extra time.
- Complete Independence: Performs the task without any assistance.
- Levels of Assistance:
- CARES Tool: (Comprehensive Assessment of Repetitive Evaluation Systems) A standardized tool that assesses an individual's cognitive abilities across a range of domains.
- Outcome Measures (OMs):
- Purpose: Quantify patient progress, measure effectiveness of intervention, and guide treatment.
- Example OMs: Berg Balance Scale, Timed Up and Go (TUG), Dynamic Gait Index (DGI), Functional Gait Assessment (FGA), 10 Meter Walk, 6-Minute Walk, 5 Times Sit to Stand, Fugl-Meyer Assessment, Performance-Oriented Mobility Assessment (PASS), Tinetti Balance Scale, Romberg Test, Functional Reach.
- Cut-Off Scores and Implications: Each OM has a standardized scoring range with established cut-off scores that indicate level of function or impairment.
- Goal Writing:
- SMART Goals: Specific, Measurable, Achievable, Relevant, Time-bound.
- Neuro-Functional Goal: Focuses on improving functional abilities related to a neurological condition.
- SOAP Notes:
- Subjective: Patient reported symptoms and concerns.
- Objective: Measurable findings from assessments.
- Assessment: Analysis of the patient's condition and progress.
- Plan: Outline of the future treatment plan.
Interventions & Outcome Measures for Parkinson's Disease (PD)
- EDGE Recommended OMs for PD: Scales that align with the ICF model and assess specific areas of function affected by PD.
- Hoehn & Yahr (H&Y) Stages:
- Stage 1: Unilateral tremor; minimal or no disability.
- Stage 2: Bilateral disease; minimal disability.
- Stage 3: Bilateral disease; significant disability; postural instability.
- Stage 4: Severe disability; unable to stand or walk without assistance.
- Stage 5: Wheelchair-bound or bedridden.
- LSVT (Lee Silverman Voice Treatment): Focuses on increasing vocal intensity through high-intensity, repetitive speech exercises to improve speech, language, and swallowing.
- Addressing Freezing & Festination:
- Freezing: A sudden inability to move.
- Festination: Increasing speed of walking.
- High-Intensity Training: Improves cardiovascular fitness and muscle strength with exercises that are challenging but achievable for the person with PD.
CVA Intervention Planning and Constraint Induced Movement Therapy (CIMT)
- Outcome Measures to Predict Motor Recovery Post Stroke: Fugl-Meyer Assessment and the Chedocke Arm and Hand Activity Inventory.
- CIMT: A therapy that restricts the use of the less-affected limb to promote the use of the weak limb.
- Transfer Package Recommendations: Specific guidelines for patients with stroke who are eligible for CIMT.
- Inclusion Criteria for CIMT: Criteria that determine if a patient is a good candidate for CIMT.
- Shaping vs. Functional Exercises: Shaping exercises focus on specific movements, while functional exercises train for daily activities.
- Mirror Therapy: A technique that uses visual feedback from a mirror to trick the brain into thinking the unaffected limb is moving the affected limb.
- Functional Electrical Stimulation (FES): Uses electrical currents to stimulate muscles and improve movement.
- Treadmill Training: Improves walking and balance.
Contraversive Pushing
- Contraversive Pushing: A tendency to push away from the affected side after stroke.
- Burke Lateropulsion Scale: Measures lateral displacement during gait.
- Scale for Contraversive Pushing: Measures the severity of contraversive pushing.
Intro to Clinical Reasoning; Augmented Interventions:
- ICF Framework:
- Body Functions and Structures: physiological functions of body systems and anatomical parts
- Activities: execution of tasks or actions by an individual
- Participation: involvement in life situations
- Environmental Factors: physical, social, and attitudinal environment
- Personal Factors: individual's unique background, experiences, gender, etc.
- Neuroplasticity:
- Principles: the brain's ability to reorganize and change its structure and function in response to experiences
- Terms:
- Synaptic Plasticity: changes in synaptic strength and connections
- Neurogenesis: growth of new neurons
- Axonal Sprouting: new branches grow from existing neurons
- Cortical Remapping: reassignment of brain areas to new functions
- Application of Neuroplasticity for Recovery:
- Characteristics Ideal for Recovery:
- Intensity: high frequency and repetition of activity
- Specificity: exercises match the desired function
- Time: sufficient duration for neuroplastic changes to occur
- Challenge: exercises push the individual beyond their comfort zone
- Repetition: repeated practice promotes skill acquisition
- Variability: introducing new exercises or challenges keeps the brain engaged
- Characteristics Ideal for Recovery:
- Treatment Frameworks:
- Restorative: Aim to regain lost function
- Augmented: Enhance existing abilities through techniques like constraint-induced movement therapy (CIMT)
- Compensatory: Adapt to limitations by using assistive devices or alternative strategies
- Stages of Motor Learning:
- Cognitive Stage: understanding the skill and making errors
- Associative Stage: refining the skill and reducing errors
- Autonomous Stage: performing the skill automatically and without conscious effort
- Roles and Responsibilities of Healthcare Professionals:
- Physical Therapist (PT): develops and implements individualized treatment plans, evaluates functional limitations and impairments
- Physical Therapist Assistant (PTA): carries out treatment plans under the supervision of the PT
- Physical Therapy Aide: assists with patient care, including setup and cleanup, but does not provide direct interventions
Goal Writing and Outcome Measures:
- FIM (Functional Independence Measure):
- Components:
- Self-Care: eating, grooming, bathing, dressing, toileting
- Sphincter Control: bowel and bladder management
- Mobility: bed mobility, transfers, walking
- Communication: understanding, expressing
- Social Cognition: memory, attention, problem-solving
- Levels of Assistance:
- Complete Dependence (7): patient unable to perform
- Maximal Assistance (6): patient performs 25% or less
- Moderate Assistance (5): patient performs 25-50%
- Minimal Assistance (4): patient performs 50-75%
- Supervision (3): patient requires verbal cues or supervision
- Modified Independence (2): patient performs task with assistive device or extra time
- Complete Independence (1): patient performs task without assistance
- Not Applicable (0): task not performed or not applicable to patient
- Components:
- CARES Tool:
- Components: measures patient's emotional well-being and social support
- Outcome Measures (OMs):
- Components:
- Objectivity: reliable and quantifiable
- Validity: measures what it is intended to measure
- Reliability: consistent results over time
- Responsiveness: sensitive to change
- Application within a POC:
- Baseline: establish starting point for improvement
- Progress: monitor progress over time
- Discharge: evaluate overall improvement and determine home needs
- Components:
- Progression of Outcome Measures:
- Functional: measures daily tasks, such as walking or dressing
- Clinical: measures specific impairments, such as balance or strength
- Outcome Measure Cutoff Scores and Implications:
- Berg Balance Scale (BBS)
- Cutoff Score: < 45 indicates increased risk of falls
- ** Implications:** predict functional limitations and fall risk
- Timed Up & Go (TUG)
- Cutoff Score: > 14 seconds indicates a decline in mobility and increased risk of falls
- Implications: predict falls risk and functional limitations
- Dynamic Gait Index (DGI) & Functional Gait Assessment (FGA)
- Cutoff Score: < 19 indicates increased fall risk
- Implications: identify gait impairments and predict falls risk
- 10 Meter Walk Test:
- Cutoff Score: > 15 seconds indicates lower mobility
- Implications: assess walking speed and endurance
- Tinetti Balance and Gait Scale
- Cutoff Score: < 19 indicates risk of falls
- Implications: measure fall risk and predict future falls
- Performance-Oriented Mobility Assessment (POMA)
- Cutoff Score: < 19 indicates risk of falls
- Implications: predict fall risk and functional limitations
- Functional Reach Test
- Cutoff Score: < 10 inches indicates impaired balance and higher risk of falls
- Implications: predict falls risk and assess functional balance
- Berg Balance Scale (BBS)
- Goal Writing:
- SMART Goals:
- Specific: clear description
- Measurable: quantifiable or observable
- Achievable: realistic and attainable
- Relevant: align with the individual's needs and priorities
- Time-bound: target date or timeframe
- SMART Goals:
- SOAP Note Components:
- Subjective (S): patient's report of symptoms and experiences
- Objective (O): measurable findings, such as ROM, strength, and balance scores
- Assessment (A): interpretation of subjective and objective findings
- Plan (P): treatment plan, including interventions and goals
Interventions & Outcome Measures For Parkinson's Disease (PD)
- Edge Recommended OMs for PD:
- Unified Parkinson's Disease Rating Scale (UPDRS)
- Hoehn and Yahr (H&Y) Staging Scale
- Montreal Cognitive Assessment (MoCA)
- Mini-Mental State Examination (MMSE)
- Timed Up and Go (TUG)
- Functional Reach Test (FRT)
- Berg Balance Scale (BBS)
- Hoehn and Yahr (H&Y) Stages:
- Stage 1: unilateral involvement, minimal or no functional impairment
- Stage 2: bilateral involvement, no balance impairment
- Stage 3: bilateral involvement, mild to moderate balance impairment
- Stage 4: severe disability, requires assistance with ADLs
- Stage 5: confined to wheelchair or bed, requires maximal assistance
- Exercise for Postural Control:
- Balance Exercises:
- Practice shifting weight, standing on one leg, and reaching
- Proprioceptive Exercises:
- Use balance boards or uneven surfaces to challenge stability
- Strengthening Exercises:
- Focus on core muscles to improve stability
- Balance Exercises:
- LSVT - Facilitation of Neuroplasticity:
- Principles:
- High-Intensity Training: large amplitude movements to improve voice, speech, and movement
- Repetition and Intensity: repeated practice to promote neural changes
- Internal Focus: focus on generating force and movement
- Auditory Feedback: use of metronomes or vocal cues
- Principles:
- Addressing Freezing and Festination:
- Strategies:
- Cueing: visual, auditory, or tactile cues
- Task-Specific Training: practice maneuvers to overcome freezing
- Visual Cues: focus on a specific point or target
- Auditory Cues: use of music or metronomes
- Tactile Cues: gentle touch or pressure
- Festination: use of a weighted cart as a visual and tactile cue
- Strategies:
- High-Intensity Training (HIT):
- Effects:
- Increased muscle mass and strength
- Improved cardiovascular fitness
- Enhanced motor control
- Dosage:
- 3-5 sessions per week
- 60-75% of maximum heart rate
- 30-60 minutes per session
- Effects:
CVA Intervention Planning, CIMT (Constraint Induced Movement Therapy), Mirror Therapy and FES:
- Outcome Measures to Predict UE/LE Motor Recovery Post Stroke:
- Fugl-Meyer Assessment:
- Measures motor function, balance, and coordination
- Chedoke Arm and Hand Activity Inventory:
- Measures upper limb function, including grasp and manipulation
- Fugl-Meyer Assessment:
- Interventions to Facilitate Motor Recovery:
- CIMT:
- Elements:
- Constraint of the unaffected limb
- Intensive practice of the affected limb
- Shaping of movements to promote functional use
- Transfer Package Recommendations:
- Follow-up with OT and SLP to address cognitive and communication deficits
- Inclusion Criteria:
- Minimal voluntary movement in the affected limb
- Sufficient cognitive function to participate in training
- Elements:
- Shaping vs. Functional Exercises:
- Shaping: breaking down movements into smaller steps
- Functional: practice tasks that are relevant to daily life
- Mirror Therapy:
- Evidence:
- Reduced phantom limb pain
- Improved motor function
- Enhanced motor recovery
- Evidence:
- Functional Electrical Stimulation (FES):
- Evidence:
- Improved muscle strength and function
- Enhanced motor recovery
- Evidence:
- Treadmill Training:
- Benefits:
- Improved gait, balance, and cardiovascular fitness
- Types of Exercise:
- Body-weight supported
- Overground walking
- Partial weight bearing
- Evidence:
- Promotes motor recovery and improves functional mobility
- Benefits:
- CIMT:
Contraversive Pushing
- Burke Lateropulsion Scale:
- Features:
- Measures the severity of lateropulsion (pushing away from the less affected side)
- Assesses postural control, balance, and functional mobility
- Features:
- Scale for Contraversive Pushing:
- Features:
- Measures the severity of pushing behavior
- Assesses the presence and intensity of pushing
- Can be used to monitor progress over time and guide interventions
- Features:
- Use:
- Both scales help assess the presence and severity of pushing behavior in individuals with stroke, providing valuable information for treatment planning and monitoring progress.
Introduction to Clinical Reasoning
- ICF framework: Focus on identifying and analyzing the health condition, body functions and structures, activities, and participation of the patient within their environment.
Neuroplasticity
- Principles of Neuroplasticity: The brain's ability to change and adapt throughout life in response to experiences, learning, and injury. It is essential for motor recovery.
- Ideal Characteristics for Recovery: Factors that enhance neuroplasticity include:
- Intensity & Repetition: High-intensity exercises and repetitive practice.
- Specificity: Exercises that mimic desired movements and tasks.
- Timing: Starting rehabilitation as soon as possible after injury.
- Motivation: Patient engagement and commitment to therapy.
- Variability: Introducing new challenges and variations to exercises.
Treatment Frameworks
- Restorative: Aimed at restoring lost function. Examples include strengthening exercises, balance training, and range of motion exercises.
- Augmented: Utilizing assistive devices and techniques to enhance abilities. Examples include using adaptive equipment, technology, and assistive devices.
- Compensatory: Finding alternative ways to perform tasks when full recovery is not possible. Examples include retraining the non-affected side, using assistive devices, and adapting the environment.
Stages of Motor Learning
- Cognitive: The patient focuses on understanding the task and requires conscious effort and feedback. This stage emphasizes learning.
- Associative: The patient refines the movement and develops more efficient strategies with less conscious effort. Focus on practicing to improve consistency and automaticity.
- Autonomous: The movement is automatic and requires minimal conscious effort. This stage represents the goal of motor learning, aiming to free up attention for other tasks.
Roles and Responsibilities of Healthcare Professionals
- Physical Therapists (PTs): Design and implement individualized treatment plans based on patient needs and goals, assess and evaluate patient's progress, and provide education and instruction.
- Physical Therapist Assistants (PTAs): Implement treatment plans under the supervision of a PT. They assist with exercises, modalities, and other interventions.
- Aides: Provide support and assistance to patients. They may help with transfers, ambulation, and basic exercises.
Goal Writing and Outcome Measures
-
FIM (Functional Independence Measure): Assesses a patient's functional independence in 18 areas of daily living activities. It utilizes levels of assistance:
- Total Assistance: Patient requires 100% help from another person.
- Maximal Assistance: The patient requires at least 75% help from another person.
- Moderate Assistance: The patient requires at least 50% help from another person.
- Minimal Assistance: The patient requires at least 25% help from another person.
- Supervision: The patient requires verbal cues or another person to be within arm's reach for supervision.
- Modified Independence: Patient can perform the task independently but may require adaptive equipment or take an extended time.
- Independent: Patient can complete the task by themselves without any assistance.
-
CARES Tool: Evaluates a patient’s risk of falls.
-
Outcome Measures (OMs): Standardized assessments used to quantify a patient's functional abilities and measure progress. Examples are the Berg Balance Scale, TUG (Timed Up & Go), DGI (Dynamic Gait Index), FGA (Functional Gait Assessment), 10-Meter Walk Test, 6-Minute Walk Test, 5-Times Sit-To-Stand Test, Fugl-Meyer Assessment, PASS (Postural Assessment Scale for Stroke), Tinetti Balance and Gait Assessment, Romberg Test, and Functional Reach Test.
-
SMART Goals: Specific, Measurable, Achievable, Relevant, and Time-bound. They guide treatment and provide a framework for measuring progress.
-
SOAP Note:
- Subjective: Patient's own reported symptoms and concerns.
- Objective: Measurable data from assessments and observations.
- Assessment: Interpretation of the subjective and objective information, including diagnosis and prognosis.
- Plan: Treatment plan, including interventions, goals, and frequency.
Interventions and Outcome Measures for Parkinson's Disease (PD)
-
EDGE Recommended OMs: Standardized assessments for PD include the UPDRS (Unified Parkinson's Disease Rating Scale), Hoehn and Yahr (H&Y) Staging Scale, and MDS-UPDRS (Movement Disorder Society - Unified Parkinson's Disease Rating Scale).
-
Hoehn and Yahr (H&Y) Stages:
- Stage 1: Unilateral involvement, minimal or no functional impairment.
- Stage 2: Bilateral involvement, minimal or no functional impairment.
- Stage 3: Bilateral involvement, balance impairment, mild to moderate functional impairment.
- Stage 4: Severe disability, requiring assistance with daily activities.
- Stage 5: Bedridden or wheelchair-bound, completely dependent for all activities.
-
LSVT (Lee Silverman Voice Treatment): A high-intensity speech therapy program that utilizes loud voice exercises and feedback to improve voice amplitude, articulation, and speech intelligibility in people with Parkinson's Disease.
-
LSVT principles: Focus on increasing vocal intensity, improving speech clarity, and enhancing speech intelligibility through loud vocal exercises, self-monitoring, and task specific training.
-
Freezing & Festination: Can be addressed through strategies like:
- External Cues: Visual cues, auditory cues, and tactile cues.
- Mental Imagery: Visualizing forward movement.
- Stepping over Obstacles: Stepping over imaginary or real obstacles.
- Walking with a Wider Base of Support: Increasing stability and proprioception.
- Cueing: Using a metronome, music, or other rhythm-based prompts..
- Treadmill Training: Use of treadmill with varying speeds and resistance levels.
-
High-Intensity Training: The use of high-intensity exercise protocols to improve strength, endurance, and functional capacity, impacting motor function and quality of life. Benefits include:
- Improved Strength and Endurance: Enhancement of muscle strength and endurance.
- Increased Functional Capacity: Improved ability to perform daily activities.
- Improved Motor Function: Enhancement of coordination, balance, and gait.
CVA (Cerebrovascular Accident, Stroke) Interventions and Outcome Measures
-
Outcome Measures: Evaluate physical function, sensory function, and motor recovery in patients with Stroke. Some key outcome measures include:
- Fugl-Meyer Assessment: Evaluates motor function, sensory function, and balance.
- Chedocke Arm and Hand Activity Inventory: Assesses upper extremity activity and dexterity.
- National Institutes of Health Stroke Scale (NIHSS): Measures stroke severity.
- Wolf Motor Function Test (WMFT): Evaluates motor function in the upper extremities.
-
Interventions to Facilitate Motor Recovery:
- CIMT (Constraint-Induced Movement Therapy): A therapy approach that restricts the use of the less affected limb to force use of the affected limb. It promotes neuroplasticity.
- Mirror Therapy: An intervention that uses a mirror to create a visual illusion, stimulating the brain and improving motor recovery.
CIMT (Constraint-Induced Movement Therapy)
-
Elements of CIMT:
- Intensive Therapy: Multiple hours of therapy per day.
- Constraint: Restricting the use of the non-affected limb.
- Massed Practice: Repetitive practice of specific tasks.
- Shaping: Gradually increasing the complexity of tasks.
- Functional Exercises: Exercises that mimic real-life activities..
-
Transfer Package Recommendations: A comprehensive plan that addresses the patient's needs and prepares them for successful home integration, including a referral to home health services, community resources, and assistive devices.
-
Inclusion Criteria: Patients eligible for CIMT should meet the following criteria:
- Spontaneous Muscle Recovery: Some level of voluntary movement in the affected limb.
- Motivation: Patient's willingness to participate in intensive therapy.
- Cognitive Ability: Ability to understand and follow instructions.
- Physical Health: Not having any medical conditions that would prevent participation in intensive therapy.
Shaping vs. Functional Exercises:
- Shaping: Focuses on breaking down complex movements into smaller, more manageable steps.
- Functional Exercises: Mimic real-life activities, focusing on improving skills needed for daily tasks.
Mirror Therapy
- Mirror Therapy: Evidence suggests that mirror therapy can improve motor function in the affected limb after stroke.
- Recommendations: Combine mirror therapy with other motor rehabilitation interventions for enhanced outcomes.
FES (Functional Electrical Stimulation)
- Evidence: FES can assist with improving muscle function and reducing spasticity in people with stroke, impacting daily activities, and enhancing the ability to perform tasks independently.
- Recommendations: Use FES selectively in specific patient populations and collaborate with medical professionals for appropriate application.
Treadmill Training
- Benefits: Improves cardiovascular fitness, helps to reduce spasticity, and facilitates gait retraining.
- Types of Exercise: Overground walking, body weight supported treadmill training, or gait training.
- Evidence: Treadmill training shows promise in improving gait, balance, and functional mobility in people with stroke.
Contraversive Pushing
Burke Lateropulsion Scale:
- Assesses the severity of contraversive pushing, a phenomenon where patients with stroke push away from or lean towards the less affected side.
Scale for Contraversive Pushing:
- Features:
- Quantifies the amount of pushing behavior.
- Use: Identifies and determines the severity of contraversive pushing in stroke patients.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.