Podcast
Questions and Answers
Which cardiorespiratory problem can lead to impaired gas exchange?
Which cardiorespiratory problem can lead to impaired gas exchange?
- Decreased exercise tolerance
- Respiratory muscle dysfunction
- Impaired airway clearance
- Low lung volumes (correct)
What is a common cardiorespiratory problem related to increased work of breathing?
What is a common cardiorespiratory problem related to increased work of breathing?
- Decreased exercise tolerance
- Dyspnea (correct)
- Decrease mobility
- Pain
Which factor can cause low lung volumes in cardiorespiratory patients?
Which factor can cause low lung volumes in cardiorespiratory patients?
- Dyspnea
- Impaired gas exchange
- Pain
- Decreased mobility (correct)
What problem is commonly associated with impaired airway clearance in cardiorespiratory physiotherapy?
What problem is commonly associated with impaired airway clearance in cardiorespiratory physiotherapy?
Which aspect is considered when using clinical reasoning in cardiorespiratory physiotherapy?
Which aspect is considered when using clinical reasoning in cardiorespiratory physiotherapy?
What is a direct benefit of using the problem lists flow chart in cardiorespiratory clinical reasoning?
What is a direct benefit of using the problem lists flow chart in cardiorespiratory clinical reasoning?
What does the term 'atelectasis' refer to in the context of cardiorespiratory physiotherapy?
What does the term 'atelectasis' refer to in the context of cardiorespiratory physiotherapy?
How is positive end-expiratory pressure (PEEP) used in cardiorespiratory physiotherapy?
How is positive end-expiratory pressure (PEEP) used in cardiorespiratory physiotherapy?
Which of the following problems are commonly encountered in cardiorespiratory physiotherapy?
Which of the following problems are commonly encountered in cardiorespiratory physiotherapy?
What is the primary function of removing secretions in cardiorespiratory physiotherapy?
What is the primary function of removing secretions in cardiorespiratory physiotherapy?
How can low lung volumes impact cardiorespiratory function?
How can low lung volumes impact cardiorespiratory function?
In what way does 'atelectasis' affect alveoli?
In what way does 'atelectasis' affect alveoli?
'Equal pressure point theory' is related to the concept of:
'Equal pressure point theory' is related to the concept of:
'Closing capacity (CC)' is a term commonly associated with:
'Closing capacity (CC)' is a term commonly associated with:
What is the main purpose of using 'Collateral ventilation' in the context of respiratory therapy?
What is the main purpose of using 'Collateral ventilation' in the context of respiratory therapy?
Which clinical finding is associated with atelectasis on palpation?
Which clinical finding is associated with atelectasis on palpation?
What are the signs of atelectasis on chest X-ray?
What are the signs of atelectasis on chest X-ray?
Why does being in a supine position increase the risk of atelectasis?
Why does being in a supine position increase the risk of atelectasis?
What is the volume of gas in the lung after a normal expiration?
What is the volume of gas in the lung after a normal expiration?
Which lung capacity is required to produce an effective cough?
Which lung capacity is required to produce an effective cough?
What law determines airway resistance in the respiratory tract?
What law determines airway resistance in the respiratory tract?
Which factor influences a patient's work of breathing besides lung compliance?
Which factor influences a patient's work of breathing besides lung compliance?
'Closing volume' is a critical value within which lung capacity?
'Closing volume' is a critical value within which lung capacity?
What are the three important processes to reverse atelectasis?
What are the three important processes to reverse atelectasis?
Which lung volume is essential to maintain distal lung patency on expiration?
Which lung volume is essential to maintain distal lung patency on expiration?
Why is it important for physiotherapists to encourage an upright position in post-operative patients?
Why is it important for physiotherapists to encourage an upright position in post-operative patients?
What is the significance of equal pressure points in the context of lung health?
What is the significance of equal pressure points in the context of lung health?
How does pursed lip breathing benefit patients with COPD?
How does pursed lip breathing benefit patients with COPD?
Which factor contributes to the closing capacity in the lungs during expiration?
Which factor contributes to the closing capacity in the lungs during expiration?
What is the primary purpose of maintaining the movement of air by utilizing equal pressure points?
What is the primary purpose of maintaining the movement of air by utilizing equal pressure points?
How does a low vital capacity affect a patient's ability to maintain spontaneous ventilation?
How does a low vital capacity affect a patient's ability to maintain spontaneous ventilation?
What is the meaning of atelectasis?
What is the meaning of atelectasis?
Which pressure is used to achieve complete recruitment of alveoli in atelectasis?
Which pressure is used to achieve complete recruitment of alveoli in atelectasis?
What is the main role of PEEP in the context of atelectasis?
What is the main role of PEEP in the context of atelectasis?
Which is NOT a type of atelectasis?
Which is NOT a type of atelectasis?
What is a common clinical sign of atelectasis?
What is a common clinical sign of atelectasis?
How does atelectasis affect oxygen levels in the blood?
How does atelectasis affect oxygen levels in the blood?
Which term describes the imperfect expansion of alveoli in atelectasis?
Which term describes the imperfect expansion of alveoli in atelectasis?
What does Positive End-Expiratory Pressure (PEEP) help achieve in the alveoli?
What does Positive End-Expiratory Pressure (PEEP) help achieve in the alveoli?
Which term describes a condition where alveoli do not fully expand, causing collapsed air sacs?
Which term describes a condition where alveoli do not fully expand, causing collapsed air sacs?
What does Surfactant Impairment contribute to in the context of lung function?
What does Surfactant Impairment contribute to in the context of lung function?
Which type of atelectasis occurs due to the effects of gravity on the lungs?
Which type of atelectasis occurs due to the effects of gravity on the lungs?
In what way does Positive End-Expiratory Pressure (PEEP) affect alveolar pressure?
In what way does Positive End-Expiratory Pressure (PEEP) affect alveolar pressure?
Flashcards are hidden until you start studying
Study Notes
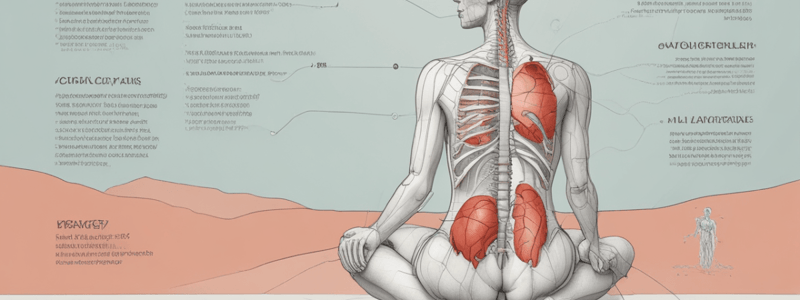
Atelectasis
- Atelectasis refers to collapsed alveoli
- The word "atelectasis" means: "Atel" = imperfect, "ectasis" = expansion
- Atelectasis can involve small groups of alveoli, or a lung segment or lobe, or it can reference the whole lung
- Palpation signs: decreased chest wall movement, increased temperature
- Auscultation signs: decreased or absent breath sounds, end-inspiratory crackles
- CXR signs: shift of structures, fissures, diaphragms, mediastinum, trachea, crowding of vessels, increased density, silhouette sign, separation of lung markings
- Risk factors: surgical incision, previous respiratory condition, smoking history, obesity, age, impaired cognitive function, monotonous pattern of mechanical ventilation, body position
Reversing Atelectasis
- Three important processes: critical opening pressure, slow laminar flow, inspiratory hold
- Critical opening pressure: necessary to open collapsed alveoli
- Slow laminar flow: helps to maintain airway patency
- Inspiratory hold: helps to recruit collapsed alveoli
Airway Resistance
- Influences work of breathing (WOB)
- References the resistance of the respiratory tract to airflow during inspiration and expiration
- Determined by Poiseuille's Law: directly proportional to the fourth power of the internal radius, inversely proportional to its length, inversely proportional to the viscosity of gas
- Clinical note: too much resistance can restrict airflow, too little resistance can stop airflow
Functional Residual Capacity (FRC)
- Volume of gas in the lung after a normal expiration
- Continues to participate in gas exchange during inspiration and expiration
- Balance between the inward recoil of the lungs and the outward recoil of chest wall
- Clinical note: low lung volumes can lead to impaired gas exchange, decreased exercise tolerance, and increased work of breathing
Lung Volumes and Capacities
- Tidal Volume (TV): necessary to maintain oxygenation and CO2 clearance
- Inspiratory Reserve Volume (IRV): required to produce an effective cough and necessary to sustain increased level of activity or exercise
- Expiratory Reserve Volume (ERV): extra volume of air that can be forcefully expelled after passive/normal expiration
- Residual Volume (RV): increased in obstructive lung disease due to air trapping
- Vital Capacity (VC): a VC of 1L is the critical value used to identify if a patient is able to maintain spontaneous ventilation
Equal Pressure Point Theory
- Equal pressure point (EPP): point in an airway where the pressure on the outside is equal to the pressure on the inside
- Creates a "squeeze point" to milk secretions from smaller airways to larger central airways and mouthward for clearing
- Clinical note: EPP is one of the factors that maintains the movement of air
Problem-Solving Framework
- Problem lists: impaired airway clearance, dyspnea/increased work of breathing, decreased exercise tolerance, low lung volumes, impaired gas exchange, decreased mobility, respiratory muscle dysfunction, pain
- Flow chart: shows how various cardiorespiratory problems are connected to each other
- Clinical reasoning table: used to determine interventions needed
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.