Podcast
Questions and Answers
Which of the following is a shared characteristic between Crohn's disease and Ulcerative Colitis (UC)?
Which of the following is a shared characteristic between Crohn's disease and Ulcerative Colitis (UC)?
- Both are triggered by environmental factors in individuals with a genetic predisposition. (correct)
- Both are primarily treated with surgical interventions.
- Both are characterized by inflammation limited to the upper gastrointestinal tract.
- Both exclusively affect the large intestine.
A patient with IBD is prescribed Sulfasalazine. What are the active metabolites produced when this drug is metabolized in the colon?
A patient with IBD is prescribed Sulfasalazine. What are the active metabolites produced when this drug is metabolized in the colon?
- Prednisone and Methotrexate.
- 5-aminosalicylic acid (5-ASA) and Prednisone.
- Sulfapyridine and Methotrexate.
- 5-ASA and Sulfapyridine. (correct)
What is the primary mechanism of action of aminosalicylates in treating IBD?
What is the primary mechanism of action of aminosalicylates in treating IBD?
- Stimulating the body's natural production of corticosteroids.
- Suppressing the immune system through direct cytotoxic effects on immune cells.
- Reducing inflammation via a salicylate (NSAID) and immunomodulatory activity. (correct)
- Providing a physical barrier to protect the inflamed intestinal lining.
A patient undergoing a colonoscopy reports feeling anxious about the procedure. Which explanation best describes the purpose of a colonoscopy?
A patient undergoing a colonoscopy reports feeling anxious about the procedure. Which explanation best describes the purpose of a colonoscopy?
Which of the following best describes the underlying cause of asthma?
Which of the following best describes the underlying cause of asthma?
What are the three main components of asthma presentation?
What are the three main components of asthma presentation?
Which of the following strategies is NOT a primary focus in the long-term management of asthma?
Which of the following strategies is NOT a primary focus in the long-term management of asthma?
Why are inhaled glucocorticoids often prescribed as a first-line maintenance treatment for asthma?
Why are inhaled glucocorticoids often prescribed as a first-line maintenance treatment for asthma?
Which of the following best describes the mechanism of action of omalizumab (Xolair) in long-term asthma maintenance?
Which of the following best describes the mechanism of action of omalizumab (Xolair) in long-term asthma maintenance?
A patient experiencing an asthma attack presents with wheezing, shortness of breath, and tachycardia. Which underlying pathophysiological process contributes most directly to these symptoms?
A patient experiencing an asthma attack presents with wheezing, shortness of breath, and tachycardia. Which underlying pathophysiological process contributes most directly to these symptoms?
In the context of asthma treatment, what is the primary advantage of using anticholinergics like ipratropium (Atrovent) in conjunction with beta-2 adrenergic agonists?
In the context of asthma treatment, what is the primary advantage of using anticholinergics like ipratropium (Atrovent) in conjunction with beta-2 adrenergic agonists?
During the management of a severe asthma attack in the emergency room, why is magnesium sulfate (MgSO4) administered intravenously?
During the management of a severe asthma attack in the emergency room, why is magnesium sulfate (MgSO4) administered intravenously?
A patient with a severe asthma exacerbation is not responding adequately to initial treatments. Which of the following interventions would be MOST appropriate to consider next?
A patient with a severe asthma exacerbation is not responding adequately to initial treatments. Which of the following interventions would be MOST appropriate to consider next?
Why might a physician prescribe montelukast (Singulair) to an asthma patient?
Why might a physician prescribe montelukast (Singulair) to an asthma patient?
During an asthma attack, a patient's arterial blood gas shows hypoxemia and hypercarbia. Which of the following physiological changes contributes directly to hypercarbia?
During an asthma attack, a patient's arterial blood gas shows hypoxemia and hypercarbia. Which of the following physiological changes contributes directly to hypercarbia?
A patient is prescribed cromolyn for long-term asthma management. How does this medication help to control asthma symptoms?
A patient is prescribed cromolyn for long-term asthma management. How does this medication help to control asthma symptoms?
Flashcards
IBD
IBD
Chronic inflammatory bowel disease, including Crohn’s disease and Ulcerative Colitis (UC).
Location of Crohn's disease
Location of Crohn's disease
Anywhere within the GI tract.
Location of Ulcerative Colitis (UC)
Location of Ulcerative Colitis (UC)
Large intestine.
Colonoscopy
Colonoscopy
Signup and view all the flashcards
Sulfasalazine
Sulfasalazine
Signup and view all the flashcards
Asthma
Asthma
Signup and view all the flashcards
Asthma Treatment Focus
Asthma Treatment Focus
Signup and view all the flashcards
Inhaled Glucocorticoids
Inhaled Glucocorticoids
Signup and view all the flashcards
Cromolyn
Cromolyn
Signup and view all the flashcards
Leukotriene Modifiers
Leukotriene Modifiers
Signup and view all the flashcards
Omalizumab (Xolair)
Omalizumab (Xolair)
Signup and view all the flashcards
Asthma Attack Symptoms
Asthma Attack Symptoms
Signup and view all the flashcards
Asthma Pathophysiology
Asthma Pathophysiology
Signup and view all the flashcards
Beta 2 Adrenergic Agonists
Beta 2 Adrenergic Agonists
Signup and view all the flashcards
Anticholinergics (for Asthma)
Anticholinergics (for Asthma)
Signup and view all the flashcards
Magnesium Sulfate (MgSO4) for Asthma
Magnesium Sulfate (MgSO4) for Asthma
Signup and view all the flashcards
Study Notes
- Inflammation 4
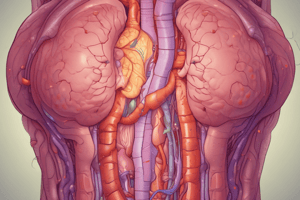
Inflammatory Bowel Disease (IBD)
- Involves chronic inflammatory conditions of the digestive tract
- Includes Crohn's disease and Ulcerative Colitis (UC)
- Risk factors are family history and environmental or bacterial triggers
- Has autoimmune components. GI cells get targeted by an atypical immune response
- Systemic signs and symptoms include fever, anemia, fatigue, weight loss, and rash
- Crohn’s disease can occur anywhere within the GI tract and causes patchy (skip) lesions which can cause lesions in the mouth
- UC affects the large intestine and starts low near rhe anus, and spreads upwards
Treatment for IBD
- Drugs classes
- Glucocorticoids provide short-term treatment and are good for flare-ups
- Aminosalicylates are a good treatment option
- DMARDs (Methotrexate) decreases the immune response and must be used in low doses due to high potency
- Stem cell research using mesenchymal stem cells offers potential treatments
Colonoscopy
- A scope is inserted into the lower GI tract for imaging
- Can help locate cobblestone appearance of surface
- Can help search for fistulas
- Can help search for patchy inflammation
- Can help search for thickening of colon wall
Aminosalicylates
- Sulfasalazine (Azulfidine, Salazopyrin) is a type of aminosalicylate
- PO administered
- Metabolizes in the colon to active metabolites
- 5-ASA: salicylate (NSAID)
- Sulfapyridine: immunomodulatory activity (DMARD)
Salicylates
- 5-ASA (Asacol, Teva, Mesalamine) is another
- Route of administration is PO or rectal and works as an NSAID
Asthma
- Also known as bronchial asthma
- A chronic inflammatory airway disorder, but not autoimmune
- Incidence: up to 10% of Canadians
- Risk factors: family history and atopy
- Etiology involves extrinsic asthma. Noxious stimuli trigger allergens, particles, infection, or stress
- There is reactivity of the airways to the mentioned stimuli
- Chronic hypersensitivity develops over time.
- Chronic inflammatory changes can cause epithelial injury
- High goblet cell activity leads to excessive mucous production
- Presentation includes bronchial inflammation, bronchoconstriction, and mucus production.
Asthma Challenges and Treatment
- Chronic bronchial inflammation is a key challenge
- Risk of acute attacks, such as a sudden extreme inflammatory response
- Stabilizing bronchial inflammation and minimizing attacks is the focus
- Avoidance of triggers is crucial
- Daily 'maintenance' drugs are used to decrease bronchial inflammation as controllers
- Correct administration technique using inhalation equipment is important
- Immunizations decrease respiratory infection risk, such as Prevnar to help pneumococcal issues
- Recognizing the signs and symptoms of an attack is beneficial
- Asthma attack drugs, known as 'rescue' drugs or 'relievers,' are available in an emergency
- Call 911 if the attack persists
Asthma Controllers
- Anti-inflammatory drugs that are inhaled
- First-line 'maintenance' treatment
- Offer prophylaxis against 'attacks'
- Drug class: Glucocorticoids such as Pulmicort (Budenoside), Qvar (Beclomethasone), Flovent (Fluticasone)
Asthma treatments
- Mast cell stabilizers like Cromolyn (cromoglicic acid)
- Leukotriene modifiers such as Singulair (montelukast)
Maintenance Biologics
- Biologics, specifically antibodies offer long term maintenance
- Drug: Xolair (omalizumab) as an SC shot
- Has a high affinity for free IgE
- Decreases expression of mast cell-bound IgE
- Reduces mast cell response and allergic inflammation
Asthma Symptoms
- Without treatment bronchoniles narrow due to cytokine release
- Goblet cells increase mucous production
- Trapping CO2 in the alveoli
Asthma Attacks
- Wheezing, shortness of breath, and decreased or no air entry into lung lobes
- Tachycardia is another symptom
- Patients can experience anxiety or panic during an attack
- Sufferers may become fatigued.
- Involves limited inspiration and a longer expiration phase, leading to air trapping in alveoli
- Hyper-inflated lungs occur with low gas exchange
- Ventilation-perfusion mismatch can lead to respiratory issues
- Hypoxemia and hypercarbia can both stem from attacks
- High pulmonary pressures can cause increased RVED, resulting in low CO
Asthma Rescue
- Bronchodilator drugs are inhaled
- Beta 2 adrenergic agonists
- The class of drugs are inhaled, like Albuterol
- The use non-inhalation routes if airways are closed
- Potent, high receptor affinity
- Stimulate SNS's B2 receptors
- Work fast
Asthma Treatment
- Asthma can be countered with Anticholinergics
- They are less potent
- Work to antagonize PNS responses
- They have a slower onset of action
- Offer synergy with Beta2 adrenergic agonists
- Atrovent (Ipratropium) is one such drug
Severe Asthma
- Severe attack could mean ER admission and symptoms of that could be life threatening
- Intervention is needed to help 02 levels, or beta2 adrenergic, or inhaled Ventolin
- Calcium channel blockers can help smooth muscles, as can magnesium sulfate(MgSO4), IV
- Anticholinergics and synergies can help too
- Adrenergics/Sympathomimetics, IV, and Epinephrine (Adrenalin) causes vasoconstriction
Supportive treatments for asthma
- Glucocorticoids IV of Dexamethasone
- Antihistamines IV like Benadryl
- Magnesium sulfate (MgSO4), IV can treat severe bronchoconstriction
- Electrolyte solution is an enzymatic activator
- Calcium channel blocker, with asthma treatment
- Stabilizes mast cells & T-cells, decreasing pro-inflammatory mediators
- Enhances release of NO. Vasodilation and improved has exchanged
- Caution. May result in hypotension. Risk is ok during asthma attacks
Asthma vs Anaphylactic Shock
- Anaphylaxis: systemic vasodilation & bronchoconstriction; Tx: ABCs
- Asthma: airway/breathing
- Asthma Attack something will bronchodilate
- ASTHMA ATTACKS and ANAPHYLAXIS share features, clear differences too
- ANAPHYLAXIS. trouble breathingcoughing, wheezing, stridor,
- asthma. no hives, swelling, vomiting, o diarrhea
- both asthma atacks anaphylaxis cause bluish skin, increased heart, decreased blood pressure, altered mental
- If not sure if attack ot anaphylaxix TREAT BOTH epinephrine then albuterol
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.