Podcast
Questions and Answers
In the context of inflammation, what happens to the glycocalyx layer on endothelial cells?
In the context of inflammation, what happens to the glycocalyx layer on endothelial cells?
- It remains unchanged, unaffected by inflammation.
- It becomes thicker, preventing the movement of substances.
- It is completely destroyed, leading to a complete loss of barrier function.
- It is damaged, allowing for easier movement of substances. (correct)
What is the typical percentage of albumin lost from the vascular space into the interstitial space?
What is the typical percentage of albumin lost from the vascular space into the interstitial space?
- 5% or less (correct)
- 1% or less
- 15% or less
- 10% or less
In the context of inflammation, what happens to the permeability of the vascular space?
In the context of inflammation, what happens to the permeability of the vascular space?
- It remains the same, there is no significant change.
- It decreases, limiting the movement of fluids and substances.
- It increases, allowing for increased movement of fluids and substances. (correct)
- It fluctuates randomly, making fluid movement unpredictable.
How might inflammation affect albumin levels?
How might inflammation affect albumin levels?
Which of the following monitoring techniques is considered a standard monitor for assessing volume status?
Which of the following monitoring techniques is considered a standard monitor for assessing volume status?
What type of monitoring might be required for a patient with a complex surgery or significant comorbidities?
What type of monitoring might be required for a patient with a complex surgery or significant comorbidities?
What type of parameters are primarily used to assess volume status?
What type of parameters are primarily used to assess volume status?
Why is it crucial to monitor intravascular volume status?
Why is it crucial to monitor intravascular volume status?
Why is controlled mechanical ventilation used when assessing respiratory variation?
Why is controlled mechanical ventilation used when assessing respiratory variation?
Which of these factors can affect the accuracy of respiratory variation assessment?
Which of these factors can affect the accuracy of respiratory variation assessment?
What is the main purpose of monitoring respiratory variation?
What is the main purpose of monitoring respiratory variation?
What happens to intrathoracic pressure during positive pressure ventilation?
What happens to intrathoracic pressure during positive pressure ventilation?
How does increased intrathoracic pressure potentially affect cardiovascular function?
How does increased intrathoracic pressure potentially affect cardiovascular function?
Which of the following parameters can be used to assess respiratory variation?
Which of the following parameters can be used to assess respiratory variation?
What is the significance of observing a significant drop in blood pressure during inspiration?
What is the significance of observing a significant drop in blood pressure during inspiration?
Why is it important to consider the overall clinical picture in addition to dynamic parameters?
Why is it important to consider the overall clinical picture in addition to dynamic parameters?
Which method is NOT commonly used for measuring cardiac output in the operating room?
Which method is NOT commonly used for measuring cardiac output in the operating room?
What is the main principle behind the use of a phenylephrine drip in determining cardiac output?
What is the main principle behind the use of a phenylephrine drip in determining cardiac output?
By interrupting an arterial blood gas (ABG) and analyzing the lactate level, what key information about tissue perfusion can be deduced?
By interrupting an arterial blood gas (ABG) and analyzing the lactate level, what key information about tissue perfusion can be deduced?
What is the primary difference between the Expiratory Occlusion Test and the Respiratory Variation (SVV) method for assessing fluid responsiveness?
What is the primary difference between the Expiratory Occlusion Test and the Respiratory Variation (SVV) method for assessing fluid responsiveness?
Which of these methods uses a pulse oximeter to assess fluid responsiveness?
Which of these methods uses a pulse oximeter to assess fluid responsiveness?
Which of these methods is considered a non-invasive method to measure cardiac output?
Which of these methods is considered a non-invasive method to measure cardiac output?
What is the primary function of CO2 rebreathing in assessing fluid responsiveness?
What is the primary function of CO2 rebreathing in assessing fluid responsiveness?
What does an increase in lactate levels indicate?
What does an increase in lactate levels indicate?
What is a common symptom of iron deficiency?
What is a common symptom of iron deficiency?
Which of the following is NOT a potential cause of iron deficiency?
Which of the following is NOT a potential cause of iron deficiency?
What is the primary role of iron in the body?
What is the primary role of iron in the body?
What is the main reason why iron deficiency can lead to anemia?
What is the main reason why iron deficiency can lead to anemia?
What is a potential risk associated with blood transfusions?
What is a potential risk associated with blood transfusions?
What is the role of reticuloendothelial cells in iron metabolism?
What is the role of reticuloendothelial cells in iron metabolism?
How does the body respond to an increase in the need for hemoglobin production?
How does the body respond to an increase in the need for hemoglobin production?
What is agglutination?
What is agglutination?
What is the recommended transfusion time frame for Cryoprecipitate (Cryo)?
What is the recommended transfusion time frame for Cryoprecipitate (Cryo)?
What is the primary reason for administering Cryo to patients?
What is the primary reason for administering Cryo to patients?
What is the standard dosage of Cryoprecipitate for a patient weighing 80 kilos?
What is the standard dosage of Cryoprecipitate for a patient weighing 80 kilos?
What is the typical storage temperature for platelet preparations?
What is the typical storage temperature for platelet preparations?
What is a potential risk associated with platelet transfusion?
What is a potential risk associated with platelet transfusion?
What is the typical lifespan of platelets in the body?
What is the typical lifespan of platelets in the body?
Why are platelets often leuko-reduced before transfusion?
Why are platelets often leuko-reduced before transfusion?
How much can a single-donor apheresis platelet pack increase a recipient's platelet count?
How much can a single-donor apheresis platelet pack increase a recipient's platelet count?
Which of the following is a potential risk of using large volumes of balanced salt solutions like Lactated Ringer's (LR)?
Which of the following is a potential risk of using large volumes of balanced salt solutions like Lactated Ringer's (LR)?
What is the primary concern regarding the use of normal saline in patients with renal insufficiency?
What is the primary concern regarding the use of normal saline in patients with renal insufficiency?
Which of the following statements is TRUE regarding the use of balanced salt solutions in patients with normal potassium levels?
Which of the following statements is TRUE regarding the use of balanced salt solutions in patients with normal potassium levels?
Which of the following is a characteristic of colloids?
Which of the following is a characteristic of colloids?
Why might 25% albumin be used instead of 5% albumin?
Why might 25% albumin be used instead of 5% albumin?
Which of the following is NOT a reason why normal saline might be used for a patient with renal insufficiency?
Which of the following is NOT a reason why normal saline might be used for a patient with renal insufficiency?
Which of the following situations might warrant the use of 25% albumin instead of 5% albumin?
Which of the following situations might warrant the use of 25% albumin instead of 5% albumin?
Which type of intravenous fluid is MOST LIKELY to be used in a patient with normal potassium levels who needs fluid replacement but has a history of renal dysfunction?
Which type of intravenous fluid is MOST LIKELY to be used in a patient with normal potassium levels who needs fluid replacement but has a history of renal dysfunction?
Flashcards
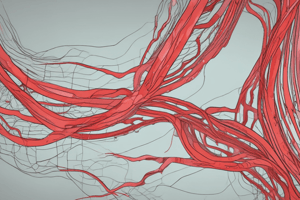
Glycocalyx
Glycocalyx
A protective layer on endothelial cells that can be damaged during inflammation.
Transcellular movement
Transcellular movement
The movement of substances across the cell membrane.
Paracellular movement
Paracellular movement
The movement of substances between adjacent cells.
Albumin movement
Albumin movement
Signup and view all the flashcards
Inflammation effects
Inflammation effects
Signup and view all the flashcards
Monitoring volume status
Monitoring volume status
Signup and view all the flashcards
Static parameters
Static parameters
Signup and view all the flashcards
Dynamic parameters
Dynamic parameters
Signup and view all the flashcards
Hyperchloremic Metabolic Acidosis
Hyperchloremic Metabolic Acidosis
Signup and view all the flashcards
Balanced Salt Solutions
Balanced Salt Solutions
Signup and view all the flashcards
Hyperlactatemia
Hyperlactatemia
Signup and view all the flashcards
Metabolic Alkalosis
Metabolic Alkalosis
Signup and view all the flashcards
Hypotonicity
Hypotonicity
Signup and view all the flashcards
Citrate Binding
Citrate Binding
Signup and view all the flashcards
Colloids
Colloids
Signup and view all the flashcards
Albumin
Albumin
Signup and view all the flashcards
Phenylephrine Effect
Phenylephrine Effect
Signup and view all the flashcards
Frank-Starling Curve
Frank-Starling Curve
Signup and view all the flashcards
Expiratory Occlusion Test
Expiratory Occlusion Test
Signup and view all the flashcards
Cardiac Output Measurement
Cardiac Output Measurement
Signup and view all the flashcards
Lactate Level
Lactate Level
Signup and view all the flashcards
Fluid Responsiveness Assessment
Fluid Responsiveness Assessment
Signup and view all the flashcards
Pulse Wave Analysis
Pulse Wave Analysis
Signup and view all the flashcards
End-Tidal CO2 Measurement
End-Tidal CO2 Measurement
Signup and view all the flashcards
Cryoprecipitate (Cryo)
Cryoprecipitate (Cryo)
Signup and view all the flashcards
Fibrinogen increase
Fibrinogen increase
Signup and view all the flashcards
Platelet lifespan
Platelet lifespan
Signup and view all the flashcards
Normal platelet count
Normal platelet count
Signup and view all the flashcards
Platelet transfusion types
Platelet transfusion types
Signup and view all the flashcards
Leukoreduction
Leukoreduction
Signup and view all the flashcards
Platelet count increase per dose
Platelet count increase per dose
Signup and view all the flashcards
Storage temperature for platelets
Storage temperature for platelets
Signup and view all the flashcards
Sensitivity and Specificity
Sensitivity and Specificity
Signup and view all the flashcards
Clinical Picture
Clinical Picture
Signup and view all the flashcards
Respiratory Variation
Respiratory Variation
Signup and view all the flashcards
Positive Pressure Breath
Positive Pressure Breath
Signup and view all the flashcards
Intrathoracic Pressure
Intrathoracic Pressure
Signup and view all the flashcards
Vasomotor Tone
Vasomotor Tone
Signup and view all the flashcards
Cardiac Function Stability
Cardiac Function Stability
Signup and view all the flashcards
Tidal Volume Consistency
Tidal Volume Consistency
Signup and view all the flashcards
Iron delivery
Iron delivery
Signup and view all the flashcards
Hemoglobin synthesis
Hemoglobin synthesis
Signup and view all the flashcards
Iron deficiency
Iron deficiency
Signup and view all the flashcards
GI absorption issues
GI absorption issues
Signup and view all the flashcards
Iron deficiency anemia
Iron deficiency anemia
Signup and view all the flashcards
Blood transfusion risks
Blood transfusion risks
Signup and view all the flashcards
Rh factor
Rh factor
Signup and view all the flashcards
Red blood cell storage
Red blood cell storage
Signup and view all the flashcards
Study Notes
Introduction
- Lecture begins with checking for questions on the previous module's content, specifically regarding dye dosing.
- Review of electrolytes and fluids is initiated.
- Total body water differences in males, females, and across age groups are highlighted.
- Intracellular and extracellular fluid compartments are discussed in terms of their relative contents of sodium, chloride, potassium, and phosphate.
Body Fluid Compartments
- Total body water in a 70 kg person is approximately 42 liters.
- Extracellular fluid is composed of about 80% interstitial fluid and 20% plasma.
- Intracellular fluid is rich in potassium.
- Extracellular fluid is rich in sodium and chloride.
- Plasma proteins contribute to oncotic pressure.
- The composition of fluids in various body compartments is described.
Tissue Fluid Movement
- Substances can move freely between interstitial fluid and plasma compartments.
- Molecules' passage through endothelial cell tight junctions, basement membrane, and glycocalyx is discussed.
- The blood-brain barrier, lungs, and heart as examples of tight compartments with continuous endothelium are mentioned.
- Vascular space interactions and influences, especially the role of inflammatory conditions, are touched upon.
Monitoring and Volume Status
- Static parameters like blood pressure, heart rate, and urine output are used to assess overall volume status.
- Limitations exist regarding the use of static monitoring during time-sensitive situations like surgery.
- Dynamic parameters, particularly changes in pulse pressure during breathing, can help evaluate volume responsiveness.
- Dynamic parameters are more useful in surgical patients, especially with massive blood loss.
Treatment of Fluid Imbalances
- Treatment options for hyperkalemia (high potassium levels) include insulin and glucose (to shift potassium into cells), calcium, and bicarbonate.
- Hypokalemia is also discussed but without details given.
- Treatment for acidosis (low pH) is addressed but not in great detail.
Fluid Therapy
- The choice between crystalloids and colloids in fluid therapy is mentioned.
- Crystalloids, like normal saline or lactated ringers, are often used initially for fluid replacement, but the use of colloids, like albumin solutions, may be preferred in cases of significant blood loss or hypovolemia.
- The need for careful monitoring, and the associated potential for complications (e.g., hypervolemia or electrolyte imbalances) is stressed, especially in hypovolemic patients.
Electrolyte Concentrations
- Key electrolytes, including their approximate concentrations in body fluids (plasma), are discussed.
- The difference between isotonic, hypotonic, and hypertonic solutions in relation to plasma is covered.
- Functions of sodium and chloride in extracellular fluids and potassium in intracellular fluid are described.
Measuring Body Composition
- Calculation and interpretation of pulse pressure variations, along with their use in assessing volume response during fluid resuscitation in an acute care setting, is demonstrated.
- Various types and uses of solutions in relation to different medical conditions are touched upon, including the potential issues that can arise.
Discussion and Conclusion
- An overview of various clinical scenarios, including cases with massive blood loss in surgical settings, was covered.
- Specific types of surgical procedures and complications were discussed.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.