Podcast
Questions and Answers
What is the primary function of fibroblasts?
What is the primary function of fibroblasts?
- Secretion of antibodies
- Synthesis of all types of connective tissue fibers (correct)
- Production of heparin
- Phagocytosis of pathogens
Which of the following cells is specifically involved in allergic reactions?
Which of the following cells is specifically involved in allergic reactions?
- Macrophage
- Plasma cell
- Mast cell (correct)
- Fibroblast
What constitutes the structural unit of white collagenous fibers?
What constitutes the structural unit of white collagenous fibers?
- Elastin molecules
- Type-I tropocollagen molecules (correct)
- Type-II tropocollagen molecules
- Myofibrils
Where are yellow elastic fibers predominantly found?
Where are yellow elastic fibers predominantly found?
Which staining technique reveals collagen fibers as blue?
Which staining technique reveals collagen fibers as blue?
What is a characteristic histological feature of plasma cells as observed under light microscopy?
What is a characteristic histological feature of plasma cells as observed under light microscopy?
What condition is associated with mutations in the fibrillin gene?
What condition is associated with mutations in the fibrillin gene?
Which characteristic is true regarding yellow elastic fibers?
Which characteristic is true regarding yellow elastic fibers?
Which of the following statements accurately describes the function of mast cells?
Which of the following statements accurately describes the function of mast cells?
What is the role of macrophages in connective tissue?
What is the role of macrophages in connective tissue?
Which structural component is notably abundant in the cytoplasm of plasma cells?
Which structural component is notably abundant in the cytoplasm of plasma cells?
In the histological examination, which feature distinguishes mast cells from other connective tissue cells?
In the histological examination, which feature distinguishes mast cells from other connective tissue cells?
Which pathological condition is associated with abnormal proliferation of plasma cells?
Which pathological condition is associated with abnormal proliferation of plasma cells?
What is the major role of heparin secreted by mast cells?
What is the major role of heparin secreted by mast cells?
Which description best fits the cytological appearance of a plasma cell's nucleus when examined under electron microscopy?
Which description best fits the cytological appearance of a plasma cell's nucleus when examined under electron microscopy?
Which component of mast cells helps in attracting eosinophils to sites of allergic reactions?
Which component of mast cells helps in attracting eosinophils to sites of allergic reactions?
What is the primary role of IgE in the sequence of events during anaphylaxis?
What is the primary role of IgE in the sequence of events during anaphylaxis?
Which mediator is responsible for the rapid contraction of smooth muscle during anaphylactic reactions?
Which mediator is responsible for the rapid contraction of smooth muscle during anaphylactic reactions?
Which type of hypersensitivity reaction involves IgE-mediated mast cell activation?
Which type of hypersensitivity reaction involves IgE-mediated mast cell activation?
What is the consequence of mast cell degranulation during anaphylaxis?
What is the consequence of mast cell degranulation during anaphylaxis?
Which component of mast cells primarily promotes blood anticoagulation?
Which component of mast cells primarily promotes blood anticoagulation?
What distinguishes the cytoplasm of mast cells from that of other cells?
What distinguishes the cytoplasm of mast cells from that of other cells?
What happens to blood capillaries during anaphylaxis?
What happens to blood capillaries during anaphylaxis?
What is the consequence of leukotrienes during anaphylaxis?
What is the consequence of leukotrienes during anaphylaxis?
What is the primary consequence of an autosomal dominant defect in α1-antitrypsin?
What is the primary consequence of an autosomal dominant defect in α1-antitrypsin?
Which type of collagen is found in reticular fibers?
Which type of collagen is found in reticular fibers?
What characterizes the structural properties of ground substance in connective tissue?
What characterizes the structural properties of ground substance in connective tissue?
What is the underlying cause of Hurler syndrome?
What is the underlying cause of Hurler syndrome?
Which of the following glycosaminoglycans is non-sulfated?
Which of the following glycosaminoglycans is non-sulfated?
Which tissue condition may result from the degradation of elastic fibers by pancreatic elastase?
Which tissue condition may result from the degradation of elastic fibers by pancreatic elastase?
What happens to reticular fibers when stained with silver?
What happens to reticular fibers when stained with silver?
What is NOT a major component of ground substance in connective tissue?
What is NOT a major component of ground substance in connective tissue?
Flashcards are hidden until you start studying
Study Notes
Plasma Cells
- Originate from B lymphocytes
- LM: Ovoid shape, small eccentric nucleus with heterochromatin radiating from the center, giving a cartwheel appearance. Cytoplasm is strong basophilic with a pale area representing the Golgi apparatus, called the negative Golgi image.
- EM: Extensive RER, Golgi, and numerous mitochondria
- Function: Responsible for humoral immunity (Antibodies), present in the submucosa of GIT.
- Medical Application: Multiple myeloma - Abnormal plasma cells (myeloma cells) accumulate in bone marrow, activating osteoclasts, resulting in painful, lytic bone lesions, hypercalcemia, and suppression of hematopoiesis (anemia, leukopenia, and thrombocytopenia). Overproduction of immunoglobulin can lead to myeloma nephropathy (increased serum creatinine and hematuria).
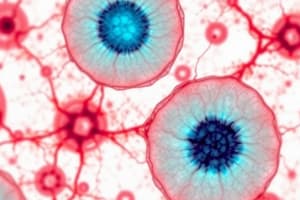
Mast Cells
- LM: Oval or rounded shape, abundant in loose CT along blood vessels. Central, rounded nucleus. Cytoplasm is full of basophilic secretory granules.
- EM: Well developed Golgi, mitochondria, ribosomes, and electron dense granules
- Function: Secrete heparin (anticoagulant, cofactor for lipoprotein lipase) and histamine (involved in antigen-antibody reaction in allergies), as well as eosinophilic chemotactic factor (stimulates eosinophil migration).
- Sequence of events in anaphylaxis (Activation & degranulation):
- Initial exposure to an allergen (e.g., bee venom) results in the production of IgE by plasma cells
- IgE binds to mast cells
- Subsequent exposure to the same allergen results in the binding of the antigen to IgE on the mast cells, activating receptor coupling factors
- This triggers the release of primary mediators from granules (histamine, heparin, ECF-A, leukotriens)
- Histamine: Contraction of smooth muscle, dilation of blood capillaries, and increased permeability leading to plasma leakage, red skin (wheals) and edema (urticaria).
- Leukotriens: Slow contraction of smooth muscle and increase vascular permeability
- ECF-A: Attracts blood eosinophils
- Heparin: Acts as an anticoagulant
- This leads to severe hypotension, mucosal edema of the respiratory tract, which can cause suffocation.
- Note: Some drugs (e.g., penicillin and cephalosporins) can cause acute urticaria by triggering IgE-mediated mast cell activation (type 1 hypersensitivity reaction).
Connective Tissue Cells Comparison Table
| Feature | Fibroblast | Macrophage | Mast Cell | Plasma Cell |
|---|---|---|---|---|
| Origin | UMC | Blood Monocyte | UMC | B-lymphocyte |
| LM: Shape | Irregular branched | Irregular branched | Oval or rounded | Oval |
| LM: Cytoplasm | Basophilic | Pale basophilic, vacuolated | Basophilic granular | Basophilic with negative Golgi image, spherical |
| LM: Nucleus | Central pale nucleus with prominent nucleolus | Central nucleus, eccentric kidney shaped | Eccentric nucleus with cartwheel appearance of chromatin | |
| EM | Rich RER, well-developed Golgi | Many lysosomes. Prominent RER & Golgi | Well-developed Golgi, heterogeneous granules, few mitochondria | Rich in RER & well-developed Golgi |
| Sites | CT. | Take different names in each organ (e.g., GIT, Osteoclast in bone, Kupffer cells in liver, Microglia in CNS) | Skin, Areas subjected to bacterial invasion (e.g., intestines) | Areas of chronic inflammation |
| Function | Fibroblast | Phagocytosis (ingestion and digestion) | Secretion of heparin (anti-coagulant), histamine (allergic reaction) | Synthesis of antibodies (produce all types of antibodies). |
| Ground substance | Fibroblast | Macrophage | Mast Cell | Plasma Cell |
Connective Tissue Fibers
- Collagen Fibers
- Triple helix (3 polypeptide α-chains)
- White in the fresh state
- Tough and resist stretch
- Form wavy bundles
- Bundles branch, but single fibers do not branch
- LM: Acidophilic with H & E, blue with Mallory trichrome stain
- EM: Each collagenous fiber is composed of fibrils
- Each fibril is formed of type-I tropocollagen molecules that are synthesized by fibroblasts
- Elastic Fibers
- Yellow in the fresh state
- Elastic in nature (can be stretched but recoil after release of the stretch)
- Fibers branch and may form elastic membranes
- LM: Acidophilic with H & E, yellow by Van-Gieson stain
- EM: Each fiber is formed of amorphous protein (elastin) in the center and microfibrills (oxytalan fibers) in the periphery.
- Sites: Walls of arteries, trachea, bronchi, bronchioles, ligamentum flavum between vertebrae
- Medical Application: Mutations in the fibrillin gene result in Marfan syndrome, a disease characterized by a lack of resistance in tissues rich in elastic fibers. This can lead to aortic aneurysms (life-threatening). Degradation of elastic fibers can occur via pancreatic elastase enzyme, which is inhibited by α1-antitrypsin. Autosomal dominant defect in α1-antitrypsin can lead to lung emphysema (damage of lung alveoli due to loss of supporting elastic tissue).
- Reticular Fibers
- Very thin fibers that branch and anastomose to form a network
- LM: Not stained with H & E, stained brown-black with silver
- EM: Composed of type-III collagen coated by glycoprotein
- Sites: Stroma of parenchymatous organs (e.g., liver, spleen, and lymph nodes)
Ground Substance
- The intercellular material in which the fibers and cells are embedded
- Not visible in ordinary sections because it is soluble in most solvents
- Complex mixture of glycosaminoglycans (GAGs) and glycoproteins
- Proteoglycans: Protein (5%) and repeating disaccharide units (polysaccharide chains) (95%). Examples: Hyaluronic acid (non-sulfated), chondroitin sulfate, dermatan sulfate, keratan sulfate, heparan sulfate
- Glycoproteins: Conjugation of protein & carbohydrates. Examples: chondronectin, fibronectin, integrins, laminin
- Also contains water and salts.
- Medical Application: Deficiency of lysosomal enzymes that degrade specific GAGs can lead to the accumulation of these macromolecules in tissues, causing disorders like Hurler and Hunter syndromes.
- Hurler syndrome is caused by a deficiency of a lysosomal enzyme breaks down dermatan sulfate and heparin sulfate (GAG). Leads to an accumulation of GAG in the body, causing severely dysfunctional cells and their death.
- Hunter syndrome is a rare, inherited disorder where the body cannot properly digest sugar molecules (mucopolysaccharides) in the body.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.