Podcast
Questions and Answers
What is the most striking feature observed on PB smears?
What is the most striking feature observed on PB smears?
- High white blood cell count
- Presence of blast cells
- Rouleaux formation (correct)
- Leucoerythroblastic picture
Rouleaux formation is related to which of the following?
Rouleaux formation is related to which of the following?
- Severity of anemia
- Increased platelet count
- Number of lymphocytes
- Quantity and type of M protein (correct)
Which picture may be observed in some cases along with Rouleaux formation?
Which picture may be observed in some cases along with Rouleaux formation?
- Hemolytic anemia picture
- Leucoerythroblastic picture (correct)
- Granulocytic picture
- Thrombocytopenic picture
Which factor is NOT typically associated with Rouleaux formation?
Which factor is NOT typically associated with Rouleaux formation?
What does Rouleaux formation indicate about the blood's composition?
What does Rouleaux formation indicate about the blood's composition?
What can be said about the variation of plasma cells in the observed cases?
What can be said about the variation of plasma cells in the observed cases?
What is the upper limit of plasma cell variation reported?
What is the upper limit of plasma cell variation reported?
What is the minimum change reported for plasma cells?
What is the minimum change reported for plasma cells?
What is observed in trephine biopsy sections in certain instances?
What is observed in trephine biopsy sections in certain instances?
In which month was the update regarding plasma cells reported?
In which month was the update regarding plasma cells reported?
Which feature may be present alongside increased PCs in trephine biopsy sections?
Which feature may be present alongside increased PCs in trephine biopsy sections?
What is implied about the consistency of plasma cell increase across cases?
What is implied about the consistency of plasma cell increase across cases?
What types of arrangements of PCs might be evident in trephine biopsy sections?
What types of arrangements of PCs might be evident in trephine biopsy sections?
Besides PCs, which of the following is NOT mentioned as potentially being observed in trephine biopsy sections?
Besides PCs, which of the following is NOT mentioned as potentially being observed in trephine biopsy sections?
Which of the following correctly describes the plasma cell distribution possible in trephine biopsy sections?
Which of the following correctly describes the plasma cell distribution possible in trephine biopsy sections?
What does a bone marrow trephine biopsy indicate?
What does a bone marrow trephine biopsy indicate?
What characteristic is seen in some plasma cells according to the biopsy results?
What characteristic is seen in some plasma cells according to the biopsy results?
Which type of infiltration is indicated by the biopsy findings?
Which type of infiltration is indicated by the biopsy findings?
What does the presence of clusters of plasma cells in the biopsy suggest?
What does the presence of clusters of plasma cells in the biopsy suggest?
What type of cells shows cytological atypia in the bone marrow biopsy?
What type of cells shows cytological atypia in the bone marrow biopsy?
What is an important use of MRI imaging in clinical assessment?
What is an important use of MRI imaging in clinical assessment?
In which scenario would MRI imaging be particularly beneficial?
In which scenario would MRI imaging be particularly beneficial?
When is detailed imaging of a symptomatic area necessary using MRI?
When is detailed imaging of a symptomatic area necessary using MRI?
What condition can MRI help assess that involves the spinal cord?
What condition can MRI help assess that involves the spinal cord?
Which of the following is NOT a reason to utilize MRI imaging?
Which of the following is NOT a reason to utilize MRI imaging?
What primarily defines a phenotypically aberrant plasma cell population?
What primarily defines a phenotypically aberrant plasma cell population?
Which marker is used to confirm the clonal plasma cell population?
Which marker is used to confirm the clonal plasma cell population?
What does the presence of normal residual plasma cells indicate?
What does the presence of normal residual plasma cells indicate?
What color represents the phenotypically aberrant plasma cell population in the description?
What color represents the phenotypically aberrant plasma cell population in the description?
Which statement accurately describes the distinction between aberrant and normal plasma cells?
Which statement accurately describes the distinction between aberrant and normal plasma cells?
Flashcards
Plasma cell count
Plasma cell count
The number of plasma cells can be slightly higher than normal or as much as 90% higher than normal.
Plasma Cell
Plasma Cell
A type of immune cell that produces antibodies.
Increased Plasma Cells
Increased Plasma Cells
Plasma cells in the blood increase to as high as 90%.
Rouleaux formation
Rouleaux formation
Signup and view all the flashcards
PB smears
PB smears
Signup and view all the flashcards
M protein
M protein
Signup and view all the flashcards
Leucoerythroblastic picture
Leucoerythroblastic picture
Signup and view all the flashcards
MRI use in extramedullary disease
MRI use in extramedullary disease
Signup and view all the flashcards
MRI for cord compression
MRI for cord compression
Signup and view all the flashcards
MRI for detailed imaging
MRI for detailed imaging
Signup and view all the flashcards
Trephine biopsy
Trephine biopsy
Signup and view all the flashcards
Plasma Cells (PCs)
Plasma Cells (PCs)
Signup and view all the flashcards
Focal clusters/nodular aggregates of PCs
Focal clusters/nodular aggregates of PCs
Signup and view all the flashcards
Sheets of PCs
Sheets of PCs
Signup and view all the flashcards
Increased PCs
Increased PCs
Signup and view all the flashcards
Bone marrow infiltration
Bone marrow infiltration
Signup and view all the flashcards
Plasma cell clusters
Plasma cell clusters
Signup and view all the flashcards
Cytologic atypia
Cytologic atypia
Signup and view all the flashcards
Bone marrow trephine biopsy
Bone marrow trephine biopsy
Signup and view all the flashcards
Massive infiltration
Massive infiltration
Signup and view all the flashcards
Phenotypically aberrant plasma cells
Phenotypically aberrant plasma cells
Signup and view all the flashcards
CD56 expression
CD56 expression
Signup and view all the flashcards
Lack of CD19
Lack of CD19
Signup and view all the flashcards
Light chain restriction (CyIgκ)
Light chain restriction (CyIgκ)
Signup and view all the flashcards
Study Notes
Multiple Myeloma - 2024 Update
- Multiple myeloma is a clonal plasma cell disorder, characterized by an abnormal increase in monoclonal immunoglobulins.
- It accounts for 1% of all cancers and approximately 10% of hematological malignancies.
- Slightly more common in men than women, and twice as common in African-Americans compared to Caucasians.
- Median age at diagnosis is approximately 65 years.
Disease Overview
- Unlike other malignancies that metastasize to bone, osteolytic lesions in MM don't exhibit new bone formation. Bone disease is the primary cause of morbidity.
- Other major clinical manifestations include anemia, hypercalcemia, renal failure, and an increased risk of infections.
- Extramedullary disease (EMD) occurs in approximately 1-2% of patients at initial diagnosis, and 8% develop EMD later.
Symptoms of Multiple Myeloma
- Hypercalcemia
- Renal dysfunction
- Anemia
- Bone pain
Monoclonal Gammopathy of Undetermined Significance (MGUS)
- Almost all myeloma patients originate from MGUS, a pre-malignant, asymptomatic stage.
- MGUS occurs in approximately 5% of the population over 50, and is two-fold higher in blacks versus whites.
- MGUS progresses to multiple myeloma at a rate of 1% per year. Over half of those diagnosed with MGUS have had the condition for more than 10 years before clinical diagnosis.
- An intermediate stage, called smoldering multiple myeloma (SMM), can exist between MGUS and active myeloma.
Smoldering Multiple Myeloma (SMM)
- SMM is prevalent in approximately 0.5% of the general population aged 40 or older.
- It progresses to multiple myeloma at an approximate rate of 10% in the first 5 years after diagnosis, then 3% in the next 5 years, and 1.5% per year thereafter.
- Cytogenetic abnormalities (e.g., t(4;14), del(17p), gain(1q)) are associated with a higher risk of progression to multiple myeloma.
Diagnosis
- Diagnosis necessitates the presence of one or more myeloma-defining events (MDE) in conjunction with evidence of at least 10% clonal plasma cells in a bone marrow examination or a biopsy-proven plasmacytoma.
- Myeloma-defining events (MDE): established CRAB features (hypercalcemia, renal failure, anemia, and/or lytic bone lesions), along with 3 specific biomarkers.
- Clonal bone marrow plasma cells >60%
- Serum free light chain (FLC) ratio >100 (with involved FLC level ≥100 mg/L and urinary monoclonal protein excretion ≥200 mg/24hrs)
- More than one focal lesion on MRI
- All criteria must be met for diagnosis:
- Clonal bone marrow plasma cells ≥10% or biopsy-proven bony or extramedullary plasmacytoma
- Any one or more of the following myeloma-defining events (MDE): hypercalcemia, renal insufficiency, etc.
Other Tests
- 24-hour urine collection for protein electrophoresis and immunofixation to monitor urine M protein levels and detect possible renal complications.
- Serum free light chain assay is valuable for patients lacking measurable M protein (with abnormal FLC ratio and involved FLC level ≥100 mg/L).
Biochemical Tests
- Monitoring M protein level in serum and urine (≥1 g/dL in serum or ≥200 mg/day in urine) and by serum FLC assay (monitored monthly during therapy and every 3-4 months when off-therapy).
Imaging Studies
- Low-dose whole-body CT or PET/CT scans are the preferred imaging methods for assessing bone disease.
- MRI is helpful to evaluate suspected SMM, extramedullary disease, or suspected cord compression.
Bone Marrow Study
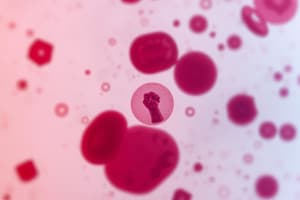
- Typically hypercellular
- Morphology of plasma cells (PCs) varies
- Classical PCs are oval with an eccentric nucleus and abundant basophilic cytoplasm.
- In some cases, plasma cells may show atypical features (e.g., Mott cells, plasmacytoses).
Other Plasma Cell Disorders
- Includes Non-IgM MGUS, characterized by serum monoclonal protein <3g/dL, clonal bone marrow plasma cells <10%, and absence of CRAB features.
- Also includes smoldering myeloma, characterized by serum monoclonal protein (and/or monoclonal protein in urine) and/or clonal bone marrow plasma cells (10-60%) without evidence of CRAB .
Clinical Presentation/Diagnosis
- A few cases may have insufficient BM aspirate or focal distribution of myeloma in the marrow, resulting in less than 10% PCs.
Solitary Plasmacytoma
- Criteria require a biopsy-proven solitary lesion of bone or soft tissue, with evidence of clonal plasma cells and a normal bone marrow with no clonal plasma cells.
- No evidence of other myeloma defining events or amyloidosis . A normal skeletal survey and MRI (except for the primary solitary lesion) of the spine and pelvis.
Solitary Plasmacytoma with Minimal Marrow Involvement
- Meets the criteria for solitary plasmacytoma, but with less than 10% clonal bone marrow plasma cells.
Molecular Cytogenetic Classification (Table 1)
- Classifies multiple myeloma based on affected genes/chromosomes. This includes hyperdiploid myeloma, IgH translocated myeloma, and others.
Prognosis and Risk Stratification
- Overall survival in transplant-eligible patients is >10 years. However, for elderly ( >75 years) patients, median survival is approximately 5 years.
- Prognosis factors include the clinical stage of disease, cytogenetic abnormalities (e.g., t(4;14), del(17p), and gain (1q), host characteristics, and response to therapy.
- The Durie-Salmon staging system and the International Staging System (ISS) are used to assess tumor burden and predict prognosis.
Disease Biology
- Reflected by multiple myeloma subtype (table 1), the presence/absence of secondary cytogenetic abnormalities (del17p, gain1q, del1p), elevated lactate dehydrogenase, and the presence of plasma cell leukemia in peripheral blood smear.
Risk Groups of Multiple Myeloma
- Standard risk: trisomies, t(11;14), and t(6;14)
- High risk: t(4;14), t(14;16), t(14;20), del(17p), and gain(1q), del(1p)
- Double and Triple-Hit Multiple Myeloma: Combination of these high risk factors
References
- https://onlinelibrary.wiley.com/doi/full/10.1002/ajh.27422
- WHO Haematolymphoid Tumours (5th edition).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.