Podcast
Questions and Answers
Which of the following is NOT a common advantage of using polyclonal antibodies in immunohistochemistry?
Which of the following is NOT a common advantage of using polyclonal antibodies in immunohistochemistry?
- They can recognize multiple epitopes on the same antigen.
- They are highly specific for a single epitope, minimizing false-positive reactions. (correct)
- They offer higher sensitivity in detecting antigens.
- They allow for the use of higher dilutions, reducing the risk of background noise.
Which of the following is NOT a common characteristic of markers used in immunohistochemistry?
Which of the following is NOT a common characteristic of markers used in immunohistochemistry?
- They must be able to alter the characteristics of the substance they mark. (correct)
- They must be able to create permanent complexes with the antibody.
- They must show the binding sites of antigen with antibody.
- They must be detectable directly or indirectly, using fluorescent dyes, enzymes, or metals.
Which of the following fluorescent dyes is NOT commonly used in immunofluorescence?
Which of the following fluorescent dyes is NOT commonly used in immunofluorescence?
- Fluorescein isothiocyanate (FITC)
- Texas Red (TR)
- Fluorescein isocyanate (FIC)
- Rhodamine 123 (correct)
What is the primary reason for using enzymes as markers in immunohistochemistry?
What is the primary reason for using enzymes as markers in immunohistochemistry?
Which of the following is a potential disadvantage of using polyclonal antibodies in immunohistochemistry?
Which of the following is a potential disadvantage of using polyclonal antibodies in immunohistochemistry?
What is the primary difference between polyclonal and monoclonal antibodies?
What is the primary difference between polyclonal and monoclonal antibodies?
What is the main advantage of using fluorescent dyes as markers in immunohistochemistry?
What is the main advantage of using fluorescent dyes as markers in immunohistochemistry?
Which of the following is NOT a common enzymatic marker used in immunohistochemistry?
Which of the following is NOT a common enzymatic marker used in immunohistochemistry?
What is the primary advantage of using monoclonal antibodies in immunochemistry techniques?
What is the primary advantage of using monoclonal antibodies in immunochemistry techniques?
Which of the following is NOT a disadvantage of using monoclonal antibodies?
Which of the following is NOT a disadvantage of using monoclonal antibodies?
Which type of antibody is most commonly used in immunocytochemistry, immunohistochemistry, and immunofluorescence techniques?
Which type of antibody is most commonly used in immunocytochemistry, immunohistochemistry, and immunofluorescence techniques?
What is the purpose of the 'somatic hybridization' process used in the production of monoclonal antibodies?
What is the purpose of the 'somatic hybridization' process used in the production of monoclonal antibodies?
Why is it important to select for clones producing the desired antibody during the production of monoclonal antibodies?
Why is it important to select for clones producing the desired antibody during the production of monoclonal antibodies?
Which of the following accurately describes the term 'paratope'?
Which of the following accurately describes the term 'paratope'?
What is the main reason why using monoclonal antibodies to examine an antigen with multiple epitopes may give inadequate results?
What is the main reason why using monoclonal antibodies to examine an antigen with multiple epitopes may give inadequate results?
Which of these factors does NOT influence the process of obtaining monoclonal antibodies?
Which of these factors does NOT influence the process of obtaining monoclonal antibodies?
Which method for retrieving epitopes involves controlled digestion of tissue sections using proteolytic enzymes?
Which method for retrieving epitopes involves controlled digestion of tissue sections using proteolytic enzymes?
What is the purpose of incubating tissue sections in 3% H2O2 solution during immunohistochemistry?
What is the purpose of incubating tissue sections in 3% H2O2 solution during immunohistochemistry?
Which of the following is NOT a proteolytic enzyme commonly used in enzyme-induced epitope retrieval (EIER)?
Which of the following is NOT a proteolytic enzyme commonly used in enzyme-induced epitope retrieval (EIER)?
What is the primary purpose of using bovine serum albumin (BSA) in immunohistochemistry?
What is the primary purpose of using bovine serum albumin (BSA) in immunohistochemistry?
Which of the following is a common method for performing heat-induced epitope retrieval (HIER)?
Which of the following is a common method for performing heat-induced epitope retrieval (HIER)?
What is the main advantage of using the indirect immunohistochemistry reaction over the direct reaction?
What is the main advantage of using the indirect immunohistochemistry reaction over the direct reaction?
Which of the following buffers is commonly used in heat-induced epitope retrieval (HIER), specifically for the purpose of adjusting the pH to facilitate epitope exposure?
Which of the following buffers is commonly used in heat-induced epitope retrieval (HIER), specifically for the purpose of adjusting the pH to facilitate epitope exposure?
What is the primary difference between direct and indirect immunohistochemistry reactions?
What is the primary difference between direct and indirect immunohistochemistry reactions?
What is the primary purpose of using IHC testing in breast cancer diagnosis?
What is the primary purpose of using IHC testing in breast cancer diagnosis?
Which of the following is NOT a routine use of IHC testing in breast cancer diagnosis?
Which of the following is NOT a routine use of IHC testing in breast cancer diagnosis?
Which of the following conditions is NOT routinely diagnosed using IHC testing?
Which of the following conditions is NOT routinely diagnosed using IHC testing?
Which of the following antibodies is specifically used to identify cells within the cytoplasm?
Which of the following antibodies is specifically used to identify cells within the cytoplasm?
What is a potential consequence of finding HER2-positive breast cancer cells?
What is a potential consequence of finding HER2-positive breast cancer cells?
Why is IHC testing generally not part of the standard diagnostic process for most cancer types?
Why is IHC testing generally not part of the standard diagnostic process for most cancer types?
What is the purpose of using a cover glass and DPX resin in the IHC staining technique?
What is the purpose of using a cover glass and DPX resin in the IHC staining technique?
Which of the following steps is NOT involved in the IHC process?
Which of the following steps is NOT involved in the IHC process?
What is the primary reason for the need for a second pathologist to review findings in most accredited labs?
What is the primary reason for the need for a second pathologist to review findings in most accredited labs?
Which of the following is NOT a factor that can influence the accuracy of IHC tests?
Which of the following is NOT a factor that can influence the accuracy of IHC tests?
What is the primary benefit of IHC testing in cancer diagnosis?
What is the primary benefit of IHC testing in cancer diagnosis?
What is the primary reason for the delay in releasing IHC test results compared to routine tests?
What is the primary reason for the delay in releasing IHC test results compared to routine tests?
Why are IHC test kits regulated by the U.S. Food and Drug Administration?
Why are IHC test kits regulated by the U.S. Food and Drug Administration?
Which of the following is a potential consequence of a false-negative IHC test result?
Which of the following is a potential consequence of a false-negative IHC test result?
What is the primary reason for the need to regularly validate IHC systems?
What is the primary reason for the need to regularly validate IHC systems?
Which of the following is NOT a potential reason for a misdiagnosis in an IHC test result?
Which of the following is NOT a potential reason for a misdiagnosis in an IHC test result?
Why is it crucial to close glass slides in medium during the final stages of preparing histological slides?
Why is it crucial to close glass slides in medium during the final stages of preparing histological slides?
Which step in the IHC protocol aims to remove the endogenous peroxidase activity that may interfere with the detection of the target antigen?
Which step in the IHC protocol aims to remove the endogenous peroxidase activity that may interfere with the detection of the target antigen?
What is the purpose of the 'negative control' in an immunohistochemistry procedure?
What is the purpose of the 'negative control' in an immunohistochemistry procedure?
What is the role of 'citric buffer' or 'EDTA' in the antigen retrieval step of immunohistochemistry?
What is the role of 'citric buffer' or 'EDTA' in the antigen retrieval step of immunohistochemistry?
Why is the application of 'blocking agents' like BSA after antigen retrieval necessary in immunohistochemistry?
Why is the application of 'blocking agents' like BSA after antigen retrieval necessary in immunohistochemistry?
Which of the following reagents are commonly used for the detection of peroxidase activity in immunohistochemistry?
Which of the following reagents are commonly used for the detection of peroxidase activity in immunohistochemistry?
What is the primary purpose of the 'deparaffinization and hydration' step in immunohistochemistry?
What is the primary purpose of the 'deparaffinization and hydration' step in immunohistochemistry?
What is the difference between the primary antibody and the secondary antibody in immunohistochemistry?
What is the difference between the primary antibody and the secondary antibody in immunohistochemistry?
Flashcards
Classes of antibodies
Classes of antibodies
Five types identified: IgA, IgD, IgE, IgG, IgM
Paratope
Paratope
The antigen binding site on an antibody that binds to an epitope
Monoclonal antibodies
Monoclonal antibodies
Antibodies produced by identical B lymphocyte clones, recognizing one antigen.
Advantages of monoclonal antibodies
Advantages of monoclonal antibodies
Highly specific, enable detection of minimal antigen differences.
Signup and view all the flashcards
Disadvantages of monoclonal antibodies
Disadvantages of monoclonal antibodies
Highly specific, may miss multi-epitope antigens and are costly to produce.
Signup and view all the flashcards
Somatic hybridization
Somatic hybridization
The process of fusing two cells to obtain monoclonal antibodies.
Signup and view all the flashcards
Hybridoma
Hybridoma
A hybrid cell line that produces monoclonal antibodies, formed from a B cell and a myeloma cell.
Signup and view all the flashcards
Steps to obtain monoclonal antibodies
Steps to obtain monoclonal antibodies
Involves immunization, cell fusion, cloning, selection, and propagation.
Signup and view all the flashcards
Polyclonal antibodies
Polyclonal antibodies
A group of antibodies recognizing one antigen but different epitopes; made by different plasma cell populations.
Signup and view all the flashcards
Advantages of polyclonal antibodies
Advantages of polyclonal antibodies
Benefits include recognition of multiple epitopes, higher dilution use, strong signals, and quick production.
Signup and view all the flashcards
Disadvantages of polyclonal antibodies
Disadvantages of polyclonal antibodies
Potential large quantities of unspecific antibodies and uniqueness in production may lead to variability.
Signup and view all the flashcards
Fluorochromes
Fluorochromes
Fluorescent dyes that emit light after radiation; used in immunofluorescence.
Signup and view all the flashcards
Common fluorochromes
Common fluorochromes
Famous types include FITC, TRITC, and Texas Red, used for fluorescence detection.
Signup and view all the flashcards
Enzyme markers
Enzyme markers
Antibodies marked with enzymes that react and produce visual signals under microscopy.
Signup and view all the flashcards
Common enzyme markers
Common enzyme markers
Examples include horseradish peroxidase and alkaline phosphatase used for detection in IHC.
Signup and view all the flashcards
Observation methods
Observation methods
Using light or electron microscopes to view the reaction of marked antibodies with antigens.
Signup and view all the flashcards
EIER
EIER
Enzyme-Induced Epitope Retrieval; uses proteolytic enzymes to retrieve antigens.
Signup and view all the flashcards
Proteolytic Enzymes
Proteolytic Enzymes
Enzymes that digest proteins; includes K proteinase and trypsin.
Signup and view all the flashcards
HIER
HIER
Heat-Induced Epitope Retrieval; involves boiling tissues in buffer solutions.
Signup and view all the flashcards
Endogenous Peroxidase Quenching
Endogenous Peroxidase Quenching
Process to prevent false-positive reactions during immunoassays.
Signup and view all the flashcards
Inhibiting Enzymatic Activity
Inhibiting Enzymatic Activity
Blocking enzyme activities like peroxidase using hydrogen peroxide.
Signup and view all the flashcards
Immunoglobulin Blocking
Immunoglobulin Blocking
Preventing non-specific binding of antibodies in tissues.
Signup and view all the flashcards
Direct Reaction
Direct Reaction
Immunoassay method using a marked antibody directly binding to an antigen.
Signup and view all the flashcards
Indirect Reaction
Indirect Reaction
Common immunoassay method; involves a secondary antibody for signal amplification.
Signup and view all the flashcards
Dehydration in slide preparation
Dehydration in slide preparation
The process of using alcohols of increasing concentrations to remove water from samples.
Signup and view all the flashcards
Clearing agents
Clearing agents
Substances like xylene used to make tissues transparent before mounting.
Signup and view all the flashcards
Mounting medium
Mounting medium
Substance applied to cover slides, protecting samples and enhancing clarity.
Signup and view all the flashcards
Positive control reactions
Positive control reactions
Reactions expected to show immunopositive staining to confirm methodology accuracy.
Signup and view all the flashcards
Negative control reactions
Negative control reactions
Experiments where staining should not occur, helping to indicate errors.
Signup and view all the flashcards
Stages of IHC reaction
Stages of IHC reaction
A sequential process including deparaffinization, antigen reveal, and antibody incubation.
Signup and view all the flashcards
Blocking endogenous peroxidase activity
Blocking endogenous peroxidase activity
Using hydrogen peroxide to inhibit peroxidase before antibody incubation.
Signup and view all the flashcards
Markers for detection
Markers for detection
Substances like DAB used to visualize reactions in IHC by changing color.
Signup and view all the flashcards
IHC testing purpose
IHC testing purpose
IHC tests are used to diagnose cancers after initial tests.
Signup and view all the flashcards
Breast cancer types diagnosed by IHC
Breast cancer types diagnosed by IHC
IHC helps diagnose invasive, metastatic, and recurrent breast cancers.
Signup and view all the flashcards
Hormone receptor status in IHC
Hormone receptor status in IHC
Tests for ER and PR to guide hormone therapy treatment options.
Signup and view all the flashcards
HER2 status in IHC
HER2 status in IHC
Checking HER2 receptors indicates fast-growing breast cancer.
Signup and view all the flashcards
Localized Ag in cells
Localized Ag in cells
Ag can be localized in nuclear, cytoplasmic, or membrane regions.
Signup and view all the flashcards
Lynch syndrome testing
Lynch syndrome testing
IHC tests identify MSH2, MSH6, PMS2, MLH1 for cancer risk.
Signup and view all the flashcards
Nuclear markers
Nuclear markers
KI67 is used as a marker for cell proliferation in tumors.
Signup and view all the flashcards
Common IHC markers for breast cancer
Common IHC markers for breast cancer
Commonly tested markers include ER, PR, HER2, and KI67.
Signup and view all the flashcards
Pathology report timeline
Pathology report timeline
The time it takes to finalize a pathology report is 2 to 10 days after a biopsy.
Signup and view all the flashcards
IHC testing duration
IHC testing duration
IHC tests usually take one day longer than routine tests.
Signup and view all the flashcards
False positives
False positives
Errors resulting in unnecessary treatment due to wrong diagnosis.
Signup and view all the flashcards
False negatives
False negatives
Errors that lead to treatment delays due to missed diagnoses.
Signup and view all the flashcards
Factors affecting IHC accuracy
Factors affecting IHC accuracy
Technology, handling of samples, and process errors can influence IHC results.
Signup and view all the flashcards
Regulation of IHC test kits
Regulation of IHC test kits
IHC kits are regulated by the U.S. FDA, requiring accuracy validation.
Signup and view all the flashcards
Validation of IHC systems
Validation of IHC systems
Pathologists must regularly validate their IHC systems for accuracy.
Signup and view all the flashcards
Second pathologist review
Second pathologist review
Most accredited labs require a second pathologist to review findings.
Signup and view all the flashcardsStudy Notes
Immunohistochemistry & Immunocytochemistry Techniques
- Immunohistochemistry and immunocytochemistry are techniques that rely on the specific binding between antigens and antibodies.
- Stereospecific interaction is characterized by the highest specificity between chemical compounds.
- Covalent bonds are not formed, but weak bonds cause molecular interaction.
- Antigenic-antibody binding involves hydrogen bonding, electrostatic interactions, and Van der Waals forces.
- Affinity histochemistry is a key histochemical technique leveraging high affinity bonding of antigens an antibodies.
- Immunohistochemistry (IHC) and hybrid cytochemistry are examples of affinity histochemistry.
Introduction
- Antibodies are characterized by their highest specificity for binding to antigens.
- This specificity results from the spatial matching (complementarity) of bonding molecules.
- Antibody-antigen binding, or purine-pyrimidine bonding in nucleic acids, occurs via weak multiple bonds from atom proximity.
Immuno... Reactions
- IHC methods rely on antigen-antibody reactions to detect and localize cells and tissues.
- These methods allow for the detection of substances with specific antigenic characteristics.
- Routinely used in cell type identification and cancer marker detection.
Cancer Type/Useful Markers
- Useful cancer markers are provided for various cancer types.
Antigen
- Antigens are multi-component substances recognized by the immune system— eliciting an immune response with specific antibody production.
- Immunogenicity refers to the antigen's ability to generate an immune response.
- Antigenicity describes an antigen's ability to bind to antibodies or receptors.
- Immunogenes possess both immunogenicity and antigenicity whereas haptens exhibit only antigenicity.
Antigen cont.
- An epitope is a part of an antigen that the immune system recognizes, usually via antibodies, B-cells, or T-cells.
- Antigens can be monovalent (possessing one epitope) or polyvalent (possessing multiple epitopes).
Antibody
- Antibodies (immunoglobulins) are glycoproteins produced by differentiated B lymphocytes (plasma cells).
- They bind specifically to antigens via variable regions (V) and constant regions (C).
- Five major immunoglobulin classes are: IgA, IgD, IgE, IgG, and IgM; IgG is most often used in immunocyto/histo/chemistry.
- Antibody variable regions contain specific antigen-binding sites (paratopes), which determine specificity.
Types of antibodies used in IHC
- Monoclonal antibodies: highly specific, recognize one antigen determinant.
- Advantages: highly specific; enabling differentiation of minimal variations in antigens; reduce background effects when compared to polyclonal antibodies.
- Disadvantages: can be expensive; time consuming; can struggle to bind to an antigen if its structure is modified, for example, due to denaturation as an epitope change.
- Polyclonal antibodies: less specific; recognize multiple epitopes, and generated from several different B cells clones.
- Advantages: react with various epitopes; high binding affinity, fewer chances of false negative results; potentially less expensive
- Disadvantages: high degree of non-specificity or cross reactivity; more background effects compared to monoclonal antibodies.
Markers used in IHC
- Markers can be directly observed using fluorochromes or indirectly through enzymes or metals.
- Fluorochromes: fluorescent dyes; visual under fluorescent microscope.
- Enzymes: require detection of enzyme activity, creating a visible marker; observed by light or electron microscope.
- Metals: observed under the electron microscope (e.g., gold); providing high contrast.
Markers used in immuno... methods
- Fluorochromes are substances that emit light after radiation.
- Commonly used fluorochromes include fluorescein isothiocyanate (FITC), tetramethylrhodamine isothiocyanate (TRITC) and Texas Red.
Markers used in IHC
- Enzymes are used for indirect detection methods.
- Examples include horseradish peroxidase, alkaline phosphatase, and glucose oxidase.
Heavy metals
- Heavy metals, such as ferritin and colloidal gold, are used for electron microscopy.
- Colloidal gold produces good contrast due to the binding of tissue with gold, and reduction of silver salt which forms a colorful precipitate.
Preparing histopathological material for tests
- Preparation involves steps like tissue fixation, processing, embedding in paraffin, slicing, deparaffinization, rehydration, staining, dehydration and clearing, concluding with slide mounting.
What's important during IHC reaction?
- Key steps include fixing, embedding, and cutting paraffin blocks, antigen retrieval, background busting, antibody selection, control reactions, and the direct or indirect method, in addition to examination.
- Each of the preceding process steps has a future influence on the final IHC reaction result.
What kind of material is used to perform IHC reaction?
- Formalin-fixed, paraffin-embedded (FFPE) tissue sections, typically 3-4 μm thick are commonly used.
- Smears can, in some circumstances, also be used.
Paraffin section preparation
- Tissue sections are deparaffinized using xylene at 56-60°C and subsequently at room temperature.
- Rehydration involves using decreasing concentrations of alcohols.
Utrwalenie materiału do IHC
- Buffered formalin (10%, pH 7.2) is a common tissue fixative.
- Aldehydes (formaldehyde, paraformaldehyde, glutaraldehyde) bind different functional groups on proteins creating crosslinks during fixation.
Antigen sites retrieval
- Fixation and embedding can modify antigen molecules, blocking antibody recognition.
- Retrieval methods restore original antigen characteristics to permit antibody binding.
- Techniques include proteolytic enzymes (e.g., trypsin, chymotrypsin) and microwaves.
Enzyme-induced epitope retrieval (EIER)
- Proteolytic enzymes are used to digest the tissue sections.
- Common proteolytic enzymes are K proteinase, E proteinase, and pronase, trypsin, or chymotrypsin in PBS buffer (pH 7.2).
- The digestion process occurs at room temperature or 37°C.
Heat-induced epitope retrieval (HIER)
- Tissue sections are boiled in a buffer, such as citrate buffer (pH 6.0), or EDTA (pH 9.0) at 95°C for 15–20 minutes, followed by cooling.
- This process can restore or expose hidden epitopes.
Inhibiting endogenous enzymatic activity
- Endogenous enzyme activity is neutralized to prevent unwanted background staining.
- This is done by incubating sections in 3% hydrogen peroxide solution for peroxidase.
- Specific inhibitors like levamisole can block alkaline phosphatase activity.
Immunoglobulins' unspecific binding sites blocking
- Blocking nonspecific sites on the tissues is crucial to prevent them from binding unrelated proteins, which can cause unwanted staining.
- Unspecific binding proteins are therefore blocked with solutions containing proteins from another species (e.g. bovine serum albumin (BSA) or non-immunized animal serum).
IHC reactions
- IHC reactions can either be direct (using a primary antibody that is marked) or indirect (using a primary antibody followed by a secondary, marked antibody).
- Direct methods bind a marked antibody directly with the target antigen, while indirect methods use a secondary antibody.
- Indirect methods are generally considered to be more sensitive to signal the reaction.
Direct reaction
- This involves incubating a tissue sample with a marked primary antibody that directly binds to the target antigen.
Indirect reaction
- This involves incubating a tissue sample with an unmarked primary antibody, followed by marked secondary antibody that binds to the primary antibody.
Detection of marking enzymes
- Detection of enzymes is the final step of immunoenzyme processes.
- A reaction detecting enzyme activity results in a colourful insoluble product, marking the antigen-antibody complex location.
Detection of Peroxidase activity
- Peroxidase activity is detected by a reaction involving diaminobenzidine (DAB) which oxidizes into a brown/dark brown product.
- The use of DAB produces a deposition product which is then visualized.
Detection of alkaline phosphatase activity
- Alkaline phosphatase activity can be detected via reactions using BCIP in conjunction with NBT.
- This yields an indigo visible product.
Staining basophilic structures
- Hematoxylin, according to Mayer, stains basophilic structures, like nuclei, dark purple/dark blue, highlighting important morphological features.
Final stages of preparing slides
- Final stages include steps like dehydration using increasing alcohol concentrations, clearing the slides with xylene I-IV, applying mounting medium, and covering with a cover slip.
Closing glass slides in medium
- Mounting medium is used to close glass slides.
- This helps improve microscopic image quality/clarity, protects the staining from physical damage/environmental factors during microscopic imaging.
Control reactions
- Control reactions are a crucial aspect of IHC testing.
- They help control results credibility, confirm methodology specificity, and highlight any artefacts.
- Positive controls reveal appropriate staining of antigens in a tissue/process; negative controls are the samples which should not stain.
Positive control reaction
- A positive control reaction uses a known positive tissue sample to confirm whether antibody-related procedures are correctly executed and will result in a positive outcome.
Negative control reactions
- Negative controls are samples that should not show staining under specific circumstances to confirm methodology accuracy and the absence of cross-reactions.
Stages of IHC reaction - Reagents
- Reagents for the different stages of IHC are detailed. This includes the processing stages such as deparaffinization and hydration, antigen retrieval, blocking endogenous peroxidase activity, background elimination, antibody incubation, and visualization and staining of basophilic structures
Detecting markers
- Markers like DAB and NBT/BCIP, used for peroxidase and alkaline phosphatase respectively, are mentioned and how their detection is accomplished.
Localization of the Ag
- Localization of target antigens is described in relation to different cellular structures.
Panels IHC
- Panels are used to examine multiple antigens using IHC, improving the evaluation of specific cancer cases.
Other markers
- List of other markers utilized for tumor detection.
Metastasis
- Information about biomarkers relevant to metastasis in various cancer types
Histology
- Examples of markers for detecting various cancer types.
Why is IHC testing done?
- IHC testing can provide a more specific diagnosis after other standard tests have been completed.
- Pathologists may use IHC tests for specific cancer types when other processes don't yield enough information.
- Individual cases may require or not require IHC testing.
Benefits and Risks of IHC testing
- IHC benefits in improving the diagnosis and treatment of various cancers.
- IHC accuracy and risks are associated with several factors.
IHC test kits
- Procedures and regulations affecting IHC tests are highlighted.
More information
- Useful web links regarding immunohistochemistry are provided.
Immunohistochemistry
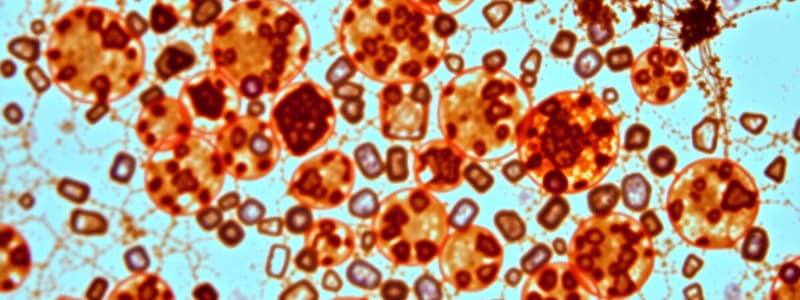
- Illustrative diagram showing the general concept of an IHC technique.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.