Podcast
Questions and Answers
Which route of lung parenchyma infection is least likely in immunocompetent individuals?
Which route of lung parenchyma infection is least likely in immunocompetent individuals?
- Direct inoculation.
- Inhalation of infectious particles.
- Hematogenous deposition. (correct)
- Aspiration of oropharyngeal contents.
A patient presents with fever, cough, and chest pain. On examination, you note rales in the right lower lobe. Which finding would be inconsistent with typical pneumonia caused by Streptococcus pneumoniae?
A patient presents with fever, cough, and chest pain. On examination, you note rales in the right lower lobe. Which finding would be inconsistent with typical pneumonia caused by Streptococcus pneumoniae?
- Bronchial breath sounds.
- Pleuritic chest pain.
- Increased tactile fremitus.
- Greenish sputum production. (correct)
Which of the following factors is least likely to predispose an individual to pneumonia?
Which of the following factors is least likely to predispose an individual to pneumonia?
- Defects in pulmonary defenses.
- Chronic lung disease.
- Increased cellular immune response. (correct)
- Advanced age.
A patient who recently had a stroke and has difficulty swallowing is at increased risk of pneumonia due to which mechanism??
A patient who recently had a stroke and has difficulty swallowing is at increased risk of pneumonia due to which mechanism??
Which of the following is the most prevalent etiological agent in community-acquired pneumonia (CAP)?
Which of the following is the most prevalent etiological agent in community-acquired pneumonia (CAP)?
What is the primary treatment strategy for acute bronchitis?
What is the primary treatment strategy for acute bronchitis?
A patient displays symptoms indicative of 'typical' pneumonia but cultures are negative for common bacterial pathogens. Broad-spectrum antibiotics are ineffective. Which less common mechanism of pneumonia should be further investigated?
A patient displays symptoms indicative of 'typical' pneumonia but cultures are negative for common bacterial pathogens. Broad-spectrum antibiotics are ineffective. Which less common mechanism of pneumonia should be further investigated?
A patient with a history of chronic alcoholism is admitted with suspected pneumonia. Sputum gram stain reveals numerous Gram-negative rods. Which of the following virulence mechanisms is most likely contributing to this patient's increased susceptibility to pneumonia?
A patient with a history of chronic alcoholism is admitted with suspected pneumonia. Sputum gram stain reveals numerous Gram-negative rods. Which of the following virulence mechanisms is most likely contributing to this patient's increased susceptibility to pneumonia?
Which characteristic is LEAST likely to be associated with 'atypical' community-acquired pneumonia (CAP)?
Which characteristic is LEAST likely to be associated with 'atypical' community-acquired pneumonia (CAP)?
A patient presents with suspected atypical pneumonia and recent exposure to birds. Which pathogen is MOST likely responsible?
A patient presents with suspected atypical pneumonia and recent exposure to birds. Which pathogen is MOST likely responsible?
Which of the following viruses associated with atypical CAP is also known to cause common colds?
Which of the following viruses associated with atypical CAP is also known to cause common colds?
A patient who recently explored caves in the Ohio River Valley presents with atypical pneumonia. Which etiological agent should be suspected?
A patient who recently explored caves in the Ohio River Valley presents with atypical pneumonia. Which etiological agent should be suspected?
Which of the following pathogens associated with atypical pneumonia is also a recognized cause of Q fever?
Which of the following pathogens associated with atypical pneumonia is also a recognized cause of Q fever?
A patient who develops pneumonia following a camping trip tests positive for an intracellular bacterium that requires arthropod vectors for transmission. Which ONE of the following microorganisms is MOST likely responsible?
A patient who develops pneumonia following a camping trip tests positive for an intracellular bacterium that requires arthropod vectors for transmission. Which ONE of the following microorganisms is MOST likely responsible?
A bone marrow transplant recipient develops atypical pneumonia. Reactivation of which latent virus is MOST suspected?
A bone marrow transplant recipient develops atypical pneumonia. Reactivation of which latent virus is MOST suspected?
Following a severe dust storm in an area known for bat guano deposits, several individuals develop atypical pneumonia characterized by granuloma formation. Which pathogen is MOST plausibly involved?
Following a severe dust storm in an area known for bat guano deposits, several individuals develop atypical pneumonia characterized by granuloma formation. Which pathogen is MOST plausibly involved?
A patient presents with a cough productive of sputum described as resembling 'red currant jelly'. Based on sputum characteristics alone, which of the following etiological agents is MOST strongly suggested?
A patient presents with a cough productive of sputum described as resembling 'red currant jelly'. Based on sputum characteristics alone, which of the following etiological agents is MOST strongly suggested?
Which physical examination finding is LEAST consistent with typical bacterial pneumonia localized to a lung zone?
Which physical examination finding is LEAST consistent with typical bacterial pneumonia localized to a lung zone?
A patient with suspected pneumonia reports recent travel involving a cruise ship and now presents with gastrointestinal symptoms alongside headache and confusion. Which pathogen should be of HIGHEST concern in this clinical scenario?
A patient with suspected pneumonia reports recent travel involving a cruise ship and now presents with gastrointestinal symptoms alongside headache and confusion. Which pathogen should be of HIGHEST concern in this clinical scenario?
Which of the following sputum descriptions is LEAST likely to be associated with Streptococcus pneumoniae pneumonia?
Which of the following sputum descriptions is LEAST likely to be associated with Streptococcus pneumoniae pneumonia?
In the context of pneumonia diagnosis, 'miliary' radiographic patterns are MOST suggestive of which broad category of pathogens?
In the context of pneumonia diagnosis, 'miliary' radiographic patterns are MOST suggestive of which broad category of pathogens?
A patient diagnosed with pneumonia exhibits a widened mediastinum on chest X-ray, but notably LACKS pulmonary infiltrates. Considering the radiographic presentation in isolation, which etiological agent should be immediately and primarily suspected?
A patient diagnosed with pneumonia exhibits a widened mediastinum on chest X-ray, but notably LACKS pulmonary infiltrates. Considering the radiographic presentation in isolation, which etiological agent should be immediately and primarily suspected?
Erythema multiforme, splenomegaly, and relative bradycardia are listed as atypical signs of pneumonia. If a patient presents with these findings alongside interstitial infiltrates on CXR, which of the following organisms would be the MOST plausible etiological agent?
Erythema multiforme, splenomegaly, and relative bradycardia are listed as atypical signs of pneumonia. If a patient presents with these findings alongside interstitial infiltrates on CXR, which of the following organisms would be the MOST plausible etiological agent?
A patient presents with pneumonia and reports working in a facility that recently experienced a suspected bioterrorism event. While awaiting confirmatory diagnostics, which of the following historical details coupled with the presenting symptoms should MOST heighten suspicion for Bacillus anthracis as the causative pathogen?
A patient presents with pneumonia and reports working in a facility that recently experienced a suspected bioterrorism event. While awaiting confirmatory diagnostics, which of the following historical details coupled with the presenting symptoms should MOST heighten suspicion for Bacillus anthracis as the causative pathogen?
Which diagnostic test, if positive, would most specifically suggest an etiology of community-acquired pneumonia (CAP) due to Legionella pneumophila?
Which diagnostic test, if positive, would most specifically suggest an etiology of community-acquired pneumonia (CAP) due to Legionella pneumophila?
A sputum Gram stain reveals numerous Gram-negative coccobacilli. Which organism is most likely to be identified?
A sputum Gram stain reveals numerous Gram-negative coccobacilli. Which organism is most likely to be identified?
In cases of severe community-acquired pneumonia (CAP) where initial diagnostic tests are unrevealing, and the patient's condition is deteriorating, which invasive procedure allows for direct visualization and sampling of the lower respiratory tract?
In cases of severe community-acquired pneumonia (CAP) where initial diagnostic tests are unrevealing, and the patient's condition is deteriorating, which invasive procedure allows for direct visualization and sampling of the lower respiratory tract?
A patient with suspected community-acquired pneumonia (CAP) exhibits a concerning clinical trajectory. Initial broad-spectrum antibiotics show no effect, and the patient's respiratory status continues to decline, necessitating mechanical ventilation. Standard diagnostic tests have been unrevealing. Which of the following advanced diagnostic strategies poses the greatest risk of complications such as pneumothorax or bleeding, but may provide critical diagnostic information when other methods have failed?
A patient with suspected community-acquired pneumonia (CAP) exhibits a concerning clinical trajectory. Initial broad-spectrum antibiotics show no effect, and the patient's respiratory status continues to decline, necessitating mechanical ventilation. Standard diagnostic tests have been unrevealing. Which of the following advanced diagnostic strategies poses the greatest risk of complications such as pneumothorax or bleeding, but may provide critical diagnostic information when other methods have failed?
A previously healthy 30-year-old patient presents with atypical pneumonia symptoms. Diagnostic workup, including sputum Gram stain and culture, blood cultures, and common respiratory viral PCR panel, are all negative. Given the epidemiological context of a recent outbreak of pneumonia among attendees of a large technology conference, which of the following serological tests would be LEAST helpful in establishing a diagnosis?
A previously healthy 30-year-old patient presents with atypical pneumonia symptoms. Diagnostic workup, including sputum Gram stain and culture, blood cultures, and common respiratory viral PCR panel, are all negative. Given the epidemiological context of a recent outbreak of pneumonia among attendees of a large technology conference, which of the following serological tests would be LEAST helpful in establishing a diagnosis?
A patient with a known history of Chronic Obstructive Pulmonary Disease (COPD) presents with pneumonia. Which of the following pathogens is MOST frequently associated with pneumonia in individuals with COPD?
A patient with a known history of Chronic Obstructive Pulmonary Disease (COPD) presents with pneumonia. Which of the following pathogens is MOST frequently associated with pneumonia in individuals with COPD?
Which of the following clinical manifestations is considered a typical symptom presentation in a patient with pneumonia?
Which of the following clinical manifestations is considered a typical symptom presentation in a patient with pneumonia?
An elderly patient is diagnosed with pneumonia and presents with new onset confusion. While confusion can be multifactorial in older adults, which specific pneumonia pathogen is particularly associated with this atypical symptom?
An elderly patient is diagnosed with pneumonia and presents with new onset confusion. While confusion can be multifactorial in older adults, which specific pneumonia pathogen is particularly associated with this atypical symptom?
Compared to community-acquired pneumonia, hospital-acquired pneumonia is characterized by a greater prevalence of which category of pathogens?
Compared to community-acquired pneumonia, hospital-acquired pneumonia is characterized by a greater prevalence of which category of pathogens?
A patient with a history of chronic alcohol abuse and diabetes mellitus develops pneumonia. Sputum examination reveals 'current jelly' appearance. Which of the following organisms is MOST likely responsible for this clinical picture?
A patient with a history of chronic alcohol abuse and diabetes mellitus develops pneumonia. Sputum examination reveals 'current jelly' appearance. Which of the following organisms is MOST likely responsible for this clinical picture?
While fever and cough are expected in pneumonia, which of the following atypical symptoms, if prominent, should raise the strongest suspicion for Legionella pneumophila as the causative agent?
While fever and cough are expected in pneumonia, which of the following atypical symptoms, if prominent, should raise the strongest suspicion for Legionella pneumophila as the causative agent?
A patient who recently explored caves in the southwestern United States presents with pneumonia. Which fungal pathogen is of GREATEST concern in this geographical and exposure context?
A patient who recently explored caves in the southwestern United States presents with pneumonia. Which fungal pathogen is of GREATEST concern in this geographical and exposure context?
In pneumonia resulting from aspiration, why is the consideration of anaerobic bacteria MORE critical compared to typical community-acquired pneumonia without aspiration risk?
In pneumonia resulting from aspiration, why is the consideration of anaerobic bacteria MORE critical compared to typical community-acquired pneumonia without aspiration risk?
Flashcards
Acute Bronchitis
Acute Bronchitis
Inflammation of the bronchi, usually viral.
Pneumonia
Pneumonia
Infection of the lung parenchyma.
Community-Acquired Pneumonia (CAP)
Community-Acquired Pneumonia (CAP)
Pneumonia acquired outside of hospitals or long-term care facilities.
Hospital-Acquired Pneumonia (Nosocomial)
Hospital-Acquired Pneumonia (Nosocomial)
Signup and view all the flashcards
Decreased Pulmonary Resistance
Decreased Pulmonary Resistance
Signup and view all the flashcards
Inhalation of Infectious Particles
Inhalation of Infectious Particles
Signup and view all the flashcards
Streptococcus pneumoniae
Streptococcus pneumoniae
Signup and view all the flashcards
Typical CAP Presentation
Typical CAP Presentation
Signup and view all the flashcards
Coccidioides immitis
Coccidioides immitis
Signup and view all the flashcards
Nursing home pneumonia
Nursing home pneumonia
Signup and view all the flashcards
Hospital-Acquired Pneumonia Pathogens
Hospital-Acquired Pneumonia Pathogens
Signup and view all the flashcards
Typical Pneumonia Symptoms
Typical Pneumonia Symptoms
Signup and view all the flashcards
Atypical Pneumonia Symptoms
Atypical Pneumonia Symptoms
Signup and view all the flashcards
COPD Pneumonia Pathogens
COPD Pneumonia Pathogens
Signup and view all the flashcards
Aspiration Pneumonia Pathogens
Aspiration Pneumonia Pathogens
Signup and view all the flashcards
Postinfluenza Pneumonia Pathogens
Postinfluenza Pneumonia Pathogens
Signup and view all the flashcards
Pulse Oximetry
Pulse Oximetry
Signup and view all the flashcards
Complete Blood Count (CBC)
Complete Blood Count (CBC)
Signup and view all the flashcards
Complete Metabolic Profile (CMP)
Complete Metabolic Profile (CMP)
Signup and view all the flashcards
Gram Stain
Gram Stain
Signup and view all the flashcards
Legionella Urinary Antigen Test
Legionella Urinary Antigen Test
Signup and view all the flashcards
Atypical CAP
Atypical CAP
Signup and view all the flashcards
Mycoplasma pneumoniae
Mycoplasma pneumoniae
Signup and view all the flashcards
Chlamydophila (Chlamydia) pneumoniae
Chlamydophila (Chlamydia) pneumoniae
Signup and view all the flashcards
Legionella pneumophila
Legionella pneumophila
Signup and view all the flashcards
Respiratory Viruses
Respiratory Viruses
Signup and view all the flashcards
COVID-19, MERS-CoV, SARS-CoV
COVID-19, MERS-CoV, SARS-CoV
Signup and view all the flashcards
Coxiella burnetii
Coxiella burnetii
Signup and view all the flashcards
Francisella tularensis
Francisella tularensis
Signup and view all the flashcards
Pertussis cough
Pertussis cough
Signup and view all the flashcards
Legionella exposure
Legionella exposure
Signup and view all the flashcards
S. pneumoniae sputum
S. pneumoniae sputum
Signup and view all the flashcards
Klebsiella sputum
Klebsiella sputum
Signup and view all the flashcards
Anaerobic infection sputum
Anaerobic infection sputum
Signup and view all the flashcards
Atypical Pneumonia signs and symptoms
Atypical Pneumonia signs and symptoms
Signup and view all the flashcards
Interstitial CXR pathogens
Interstitial CXR pathogens
Signup and view all the flashcards
Study Notes
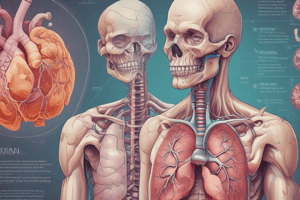
- Pneumonia and pulmonary infections are the main topics.
Acute Bronchitis
- Most cases are viral.
- Common signs and symptoms include cough, fever, scattered rhonchi, and wheezing.
- The recommended treatment includes rest, fluids, analgesics, and bronchodilators.
Pneumonia
- An infection of the lung parenchyma.
- A frequent cause of death, specifically in older adults with chronic diseases.
- Types of pneumonia include community-acquired (CAP), nursing home pneumonia, and hospital-acquired (nosocomial) pneumonia.
Pathophysiology of Pneumonia
- Mechanisms involve:
- Common inhalation of infectious particles. -Aspiration of oropharyngeal or gastric contents.
- Uncommon hematogenous deposition. -Uncommon direct inoculation. -Rare invasion from contiguous structures.
- More common re-activation in immunocompromised patients.
- Decreased resistance due to defects in pulmonary defenses and decreased cellular/humoral immune response.
"Typical" CAP Pathogens
- Classic presentation includes fever, productive cough with purulent sputum, dyspnea, and pleuritic chest pain.
- Characteristic pulmonary findings are tachypnea and rales over the involved lobe or segment.
- Increased tactile fremitus, bronchial breath sounds, and egophony may be present if consolidation has occurred.
- Streptococcus pneumoniae is the most common pathogen.
- Other pathogens include Haemophilus influenzae and Moraxella catarrhalis.
"Atypical" CAP Pathogens
- Often subacute and frequently indolent.
- Patients may present with subtle pulmonary findings, nonlobar infiltrates on radiography and various extrapulmonary manifestations like diarrhea or otalgia.
- Common pathogens include Mycoplasma pneumoniae, Chlamydophila (Chlamydia) pneumoniae, and Legionella pneumophila (Legionnaires' disease).
- Other respiratory viruses include influenza A/B, rhinovirus, respiratory syncytial virus, human metapneumovirus, adenovirus 4/7 and parainfluenza virus.
- Rare CAP includes Coxsackievirus, Echovirus, Coronavirus (COVID-19, MERS-CoV, SARS-CoV), Hantavirus etc.
Nursing Home Pneumonia
- There is an increased incidence of gram-negative bacteria and Staphylococcus aureus.
Hospital-Acquired Pneumonia
- Common pathogens include aerobic gram-negative bacilli, Pseudomonas aeruginosa, Staphylococcus aureus, MRSA, and oral anaerobes.
History and Physical Exam for Pneumonia
- Typical symptoms are hyperthermia/hypothermia, chills, tachypnea, tachycardia/bradycardia, and productive cough.
- Elderly patients may present atypically.
- Atypical symptoms may also include confusion (Legionella), diarrhea (Legionella), and rash (Mycoplasma).
History and Associated Pulmonary Pathogens
- COPD is associated with H. influenzae or M. catarrhalis.
- Alcoholism or diabetes with "current jelly sputum" is linked to Klebsiella pneumoniae.
- Asplenia is associated with S. pneumoniae and H. influenzae.
- HIV infection is associated with bacterial pathogens, M. tuberculosis, Pneumocystis jiroveci, cytomegalovirus, Cryptococcus spp., Histoplasma spp., and Coccidioides spp.
- Bronchiectasis, cystic fibrosis, or ventilator use is associated with Pseudomonas aeruginosa.
- Aspiration is associated with mixed aerobic and anaerobic infections.
- Exposure to birds is linked to Chlamydia psittaci.
- Exposure to rabbits is linked to Francisella tularensis.
- Traveling to the Mississippi/Ohio river valley or exposure to bat/bird droppings, construction sites, or caves is linked to Histoplasma capsulatum.
- Travel to desert, southwest United States associated to Coccidioides spp., Hantavirus
- Known exposure to COVID-19 is linked to COVID-19.
- Post-influenza is linked to S. Aureus or S. pneumoniae.
- Cough > 2 weeks with whooping/posttussive vomiting is associated with Bordetella pertussis.
- Hotel or cruise ship stay within the previous 2 weeks is associated with Legionella spp.
- GI symptoms along with headache and CNS symptoms are associated with Legionella spp.
- Bioterrorism alerts for Bacillus anthracis
Sputum Character
- S. pneumoniae often produces rust-colored sputum.
- Pseudomonas, Haemophilus, and S. pneumonia species may produce green sputum.
- Klebsiella species pneumonia is classically associated with red currant jelly sputum.
- Anaerobic infections often produce foul-smelling or bad-tasting sputum.
Physical Exam Findings
- Typical signs are localized to a specific lung zone and may include rales, rhonchi, bronchial breath sounds, dullness to percussion, increased tactile fremitus, and positive egophony/bronchophony/whisper pectoriloquy.
- Atypical signs and symptoms may be seen with atypical pneumonia organisms such as mental confusion, headaches, myalgias, ear pain, abdominal pain, diarrhea, rash (Horder spots in psittacosis, erythema multiforme in Mycoplasma pneumonia), nonexudative pharyngitis, hemoptysis, splenomegaly, or relative bradycardia.
CXR Patterns
- Focal infiltrate: usually bacterial.
- Large pleural effusion: usually bacterial.
- Cavitary: bacterial abscess, fungal, Nocardia, TB.
- Miliary: fungal or miliary TB.
- Interstitial: viruses, Pneumocystis, Mycoplasma, or Chlamydia psittaci.
- Mediastinal widening with no infiltrate: inhalation anthrax.
- Patients who present very early with CAP may have a negative CXR. Repeat CXR within 24 hours may be beneficial.
Additional diagnostic tests
- Pulse oximetry.
- Complete blood count.
- Complete metabolic profile.
- Rapid influenza molecular assay if influenza season.
- Sputum gram stain and culture.
- Blood cultures.
- Lactic acid level.
- C-reactive protein.
- Lactate dehydrogenase.
- Procalcitonin and CRP.
- Urinary antigen testing for Legionella species.
- Molecular diagnostics (PCR).
Gram Stain
- Gram stain results for:
- S. Pneumoniae.
- S. Aureus.
- Pseudomonas.
- Haemophilus influenzae.
- Klebsiella pneumoniae.
- Moraxella catarrhalis.
- Diagnostic testing for select patients should include Legionella serology, Mycoplasma serology, Chlamydophila serology, and stains/cultures for fungi (Pneumocystis jiroveci).
- SARS-associated coronavirus serology or PCR and cultures of pleural fluid via thoracentesis are also included.
- Bronchoscopy with bronchoalveolar lavage and transbronchial biopsy should be conducted if the patient is deteriorating and there is no definite pathogen identified.
- Additional tests include thoracoscopic or open-lung biopsy and radiographically guided transthoracic aspirate.
Pneumonia Severity Index and Curb-65
- Pneumonia Severity Index Calculator is preferred over CURB-65
Pneumonia Severity Index Risk of 30 Mortality
- Class I and II are treated with outpatient therapy, while class III is treated with outpatient or brief inpatient therapy and IV and V are treated with hospital admission.
CURB-65
- CURB-65 criteria include:
- Confusion.
- Uremia (BUN > 20 mg/dL).
- Respiratory rate (> 30/min).
- Low blood pressure (SBP < 90 or DBP ≤ 60 mmHg).
- Age (> 65 years).
- If Two or more present: hospital admission
- Newer expanded CURB-65 includes LDH, thrombocytopenia, and serum albumin.
Outpatient Empiric Treatment of CAP
- For patients with no comorbidities or risk factors for drug-resistant S. pneumoniae, the treatment is Amoxicillin 1 g PO three times a day or a macrolide (azithromycin 500 mg once then 250 mg daily or clarithromycin 500 mg twice daily) or Doxycycline 100 mg twice daily.
- For patients with comorbidities, use of antimicrobials within 90 days, or other risks for drug-resistant infection, the treatment is Beta-lactam (high-dose amoxicillin 1 g three times/day, amoxicillin/clavulanate 2 g/125 mg twice daily or 500 mg/125 mg three times daily or 875 mg/125 mg twice daily, cefpodoxime 200 mg twice daily, or cefuroxime 500 mg twice daily) plus a macrolide or doxycycline or Respiratory fluoroquinolones (moxifloxacin 400 mg daily, levofloxacin 750 mg daily).
- For children under 5 the treatment is High-dose amoxicillin and for children ages 5-16 years the treatment is Macrolides. Avoid tetracyclines/doxycyline and flouroquinolones in children.
- During influenza season, initiate oseltamivir (Tamiflu), zanamivir (Relenza), peramivir (Rapivab), or baloxavir (Xofluza) therapy in outpatients who present with a flulike illness and pneumonia.
- COVID-19/Non-hospitalized patients treatments include: -Monoclonal antibody bebtelovimab IV – FDA-authorized for people over age 12 with mild-moderate symptoms -Antiviral Paxlovid (nirmatrelvir/ritonavir) PO & Molnupiravir PO - reduces risk of covid-related hospitalization or death. Start within 5 days of symptoms for people ages 12 and older who are immunocompromised, elderly, unvaccinated.
- Patients who have not responded to therapy in 48-72 hours should be reevaluated.
Inpatient, Non-ICU and ICU treatments
- For inpatient, non-ICU treatment:
- Beta-lactams (ampicillin/sulbactam 1.5-3 g every 6 hours, ceftriaxone 1-2 g daily, cefotaxime 1-2 g every 8 hours, or ceftaroline 600 mg every 12 hours) plus a macrolide.
- Alternatively, a respiratory fluoroquinolone.
- If macrolides and fluoroquinolones are contraindicated, Beta-lactam as above plus doxycycline.
For ICU treatment:
- Beta-lactam (ceftriaxone, cefotaxime, or ampicillin/sulbactam) plus either a macrolide or respiratory fluoroquinolone.
- For patients with penicillin allergies, use a respiratory fluoroquinolone and aztreonam.
- Special Considerations:
- If Pseudomonas is a consideration: Use anti-pneumococcal and anti-pseudomonal beta-lactam (piperacillin/tazobactam 4.5 g every 6 hours, cefepime 2 g every 8 hours, ceftazidime 2 g every 8 hours, aztreonam 2 g every 8 hours, meropenem 1 g every 8 hours, or imipenem 500 mg every 6 hours).
- If severe penicillin allergy, aztreonam may be used instead of the beta-lactam in the regimen listed above.
- If CA-MRSA is a consideration: Add vancomycin or linezolid Anaerobes: Consider covering with a beta-lactam or betalactamase inhibitor.
Antibiotic treatment length
- Typical antibiotic treatments includes uncomplicated patients 5 days or Pseudomonas or MRSA 7 days depending on the patient.
- Immunocompromised patients may require longer duration
- Patients should be afebrile for 48-72 hours and be stable before antibiotic therapy is stopped.
Pneumonia prophylaxis
- Vaccines can protect people from pneumonia.
- All high risk patients should get the pneumococcal vaccine
- All high-risk patients and heath care workers should recieve annual influenza vaccines
- 5 year old and older patients should recive the COVID 19 vaccine
Lung Abscess
-
Alterations of consciousness (due to alcoholism or neurologic disorders is often seen.
-
Periodontal disease is often present.
-
Mixed anaerobic bacteria are seen in most cases.
-
Other conditions that may cause include necrotizing bacterial pneumonias by S. aureus, K. pneumoniae, or other gram-negative bacilli.
-
Bronchial obstruction due to tumors, foreign bodies, or bronchial stenosis, septic pulmonary embolization, pulmonary tuberculosis, fungal infection, or actinomycosis may lead to cavity formation.
-
Immunosuppressed hosts w/ Nocardia and other opportunistic organisms may produce cavitation.
-
Treatment is anaerobic coverage with beta-lactams or beta-lactamase inhibitors.
-
Bronciectasis is an acquired disease that leads to pooling of secretions in the airways and recurrent infections. Results most often from neglected or recurrent infections.
-
Symptoms include cough, recurrent lower respiratory tract infections, and hemoptysis. CXR may show increased lung markings, honeycombing, atelectasis, or pleural changes .
Fungal Pulmonary Infections
- Fungal pulmonary infections include:
-
- Pneumocystis Jirovecii, -- Histoplasmosis, -- Coccidioidomycosis,
- --Aspergillosis
- They're often associated with being immunocompromised, neutropenia, HIV and transplant or other immunosuppresive therapy.
- Some are endemic to particular geographic areas
- Pneumocytis Pneuemonia (PCP) is caused by Pneumocystis Jirovecii (fungus) and presents as dyspnea, fever, non-productive cough, hypoxemia w/ diffusie, bilateral, symmetrical infiltrates on CXR
- PCP is treated and prophylaxed via PO Bactrim
- Histoplasmosis most common in midwestern states in Ohio or mississippi and is found in bird and bat droppings.
- Symptoms are mostly limited to the respiratory tract in HIV patients with CD4+ counts >300 cells/μL, Fever, fatigue, weight loss, hepatosplenomegaly, and lymphadenopathy. Cough, chest pain, and dyspnea
- It is dx via H. Capulatum Culture and TX with anti fungals (amphotericin B and itraconazole)
- Coccidiomycosis is caused by a soil-dwelling fungus that consists of two species: Coccidioides immitis and C. posadasii.
- It is endemic to the Southwestern US and has symptoms of focal pneumonia in immunocompromised patients.
- TX via antifungal such as Fluconazole or Itraconazole Asperigilosis- HIV + patients (CD4 <100) is diagnosed via isolation of Aspergillus spp and TX via Voriconazole and Amphotericin B
- Blastomycosis is caused by the dimorphic fungus Blastomyces that lives in soul. It is endemic in the mid-west and can cause cutaneus infections. It is dx via Isolation of Blastomyces spp. and TX via Ampotericin B
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.