Podcast
Questions and Answers
Which clinical feature is NOT associated with hypophosphatemia?
Which clinical feature is NOT associated with hypophosphatemia?
- Rhabdomyolysis
- Increased insulin sensitivity (correct)
- Cardiomyopathy
- Growth retardation
Severe vitamin D deficiency can lead to hypophosphatemia.
Severe vitamin D deficiency can lead to hypophosphatemia.
True (A)
What is the most common metabolic abnormality seen in refeeding syndrome?
What is the most common metabolic abnormality seen in refeeding syndrome?
Hypophosphatemia
Patients with hypophosphatemia should avoid foods rich in __________.
Patients with hypophosphatemia should avoid foods rich in __________.
Match the causes of hypophosphatemia with their descriptions:
Match the causes of hypophosphatemia with their descriptions:
Which of the following is the most common cause of excess phosphorus intake?
Which of the following is the most common cause of excess phosphorus intake?
Hyperphosphatemia primarily causes symptoms similar to hypercalcemia.
Hyperphosphatemia primarily causes symptoms similar to hypercalcemia.
Name one condition that can lead to the redistribution of phosphorus from cell to blood.
Name one condition that can lead to the redistribution of phosphorus from cell to blood.
Familial tumoral calcinosis is inherited in an ______ manner.
Familial tumoral calcinosis is inherited in an ______ manner.
Match the following phosphate binders with their respective examples:
Match the following phosphate binders with their respective examples:
Which condition is associated with x-linked inheritance related to hypophosphatemic rickets?
Which condition is associated with x-linked inheritance related to hypophosphatemic rickets?
Autosomal dominant conditions related to phosphorus metabolism lead to an increase in FGF 23.
Autosomal dominant conditions related to phosphorus metabolism lead to an increase in FGF 23.
What is the daily requirement of phosphorus for an individual?
What is the daily requirement of phosphorus for an individual?
In severe hypophosphatemia, phosphorus is administered via _____ at a dosage of 10 mg/kg over 12 hours.
In severe hypophosphatemia, phosphorus is administered via _____ at a dosage of 10 mg/kg over 12 hours.
Match the following gene mutations with their outcomes:
Match the following gene mutations with their outcomes:
What happens during the end stages of Chronic Kidney Disease regarding FGF-23?
What happens during the end stages of Chronic Kidney Disease regarding FGF-23?
In Fanconi syndrome, phosphate depletion can lead to severe rickets.
In Fanconi syndrome, phosphate depletion can lead to severe rickets.
Which cotransporter is primarily responsible for the reabsorption of phosphorus in the proximal convoluted tubule?
Which cotransporter is primarily responsible for the reabsorption of phosphorus in the proximal convoluted tubule?
In Chronic Kidney Disease, increased levels of parathyroid hormone (PTH) lead to an increase in ______.
In Chronic Kidney Disease, increased levels of parathyroid hormone (PTH) lead to an increase in ______.
Match the conditions with their corresponding effects on phosphorus:
Match the conditions with their corresponding effects on phosphorus:
What is the range for hypophosphatemia in mg/dL?
What is the range for hypophosphatemia in mg/dL?
Inorganic phosphorus is primarily extracellular and mainly used to measure serum phosphorus.
Inorganic phosphorus is primarily extracellular and mainly used to measure serum phosphorus.
Where in the body is the majority of phosphorus stored?
Where in the body is the majority of phosphorus stored?
Vitamin D aids in the absorption of calcium and __________.
Vitamin D aids in the absorption of calcium and __________.
Match the following forms of phosphorus with their characteristics:
Match the following forms of phosphorus with their characteristics:
Which of the following is NOT a cause of hypomagnesemia?
Which of the following is NOT a cause of hypomagnesemia?
Torsades de pointes is associated with a decreased QT interval.
Torsades de pointes is associated with a decreased QT interval.
What is the recommended daily allowance (RDA) for magnesium?
What is the recommended daily allowance (RDA) for magnesium?
In cases of severe hypomagnesemia with arrhythmia, IV __________ is administered.
In cases of severe hypomagnesemia with arrhythmia, IV __________ is administered.
Match the following conditions with their related side effects:
Match the following conditions with their related side effects:
What is the primary site of gastrointestinal absorption for magnesium?
What is the primary site of gastrointestinal absorption for magnesium?
Thiazide drugs can lead to hypomagnesemia by affecting magnesium absorption in the kidneys.
Thiazide drugs can lead to hypomagnesemia by affecting magnesium absorption in the kidneys.
Which syndrome is inherited that affects magnesium absorption?
Which syndrome is inherited that affects magnesium absorption?
Magnesium absorption in the kidney occurs primarily through the _____ pathway.
Magnesium absorption in the kidney occurs primarily through the _____ pathway.
Match the following components with their functions:
Match the following components with their functions:
Which of the following drugs is known to impair gastrointestinal absorption of magnesium?
Which of the following drugs is known to impair gastrointestinal absorption of magnesium?
Hypomagnesemia causes an increase in the secretion of parathyroid hormone (PTH).
Hypomagnesemia causes an increase in the secretion of parathyroid hormone (PTH).
What is one common cause of hypermagnesemia related to medication intake?
What is one common cause of hypermagnesemia related to medication intake?
Symptoms such as cardiac arrest occur when magnesium levels exceed ______ meq/L.
Symptoms such as cardiac arrest occur when magnesium levels exceed ______ meq/L.
Match the conditions with their causes of hypermagnesemia:
Match the conditions with their causes of hypermagnesemia:
Which of the following drugs is known to cause tubular injury?
Which of the following drugs is known to cause tubular injury?
In hungry bone syndrome, serum calcium levels are decreased.
In hungry bone syndrome, serum calcium levels are decreased.
What causes pseudohypoparathyroidism?
What causes pseudohypoparathyroidism?
The infusion of intravenous calcium levels recommended for treating hypocalcemia is __________ grams per day.
The infusion of intravenous calcium levels recommended for treating hypocalcemia is __________ grams per day.
Match each type of pseudohypoparathyroidism with its characteristic:
Match each type of pseudohypoparathyroidism with its characteristic:
Which characteristic feature is associated with Albright's Hereditary Osteodystrophy (AHO)?
Which characteristic feature is associated with Albright's Hereditary Osteodystrophy (AHO)?
Short stature and round facies are associated findings of Down's Syndrome.
Short stature and round facies are associated findings of Down's Syndrome.
What is the characteristic feature of Turner's Syndrome?
What is the characteristic feature of Turner's Syndrome?
In Pseudohypoparathyroidism type 1a, the characteristic features include short _____ and _____ metacarpal bones.
In Pseudohypoparathyroidism type 1a, the characteristic features include short _____ and _____ metacarpal bones.
Match the following conditions with their characteristic features:
Match the following conditions with their characteristic features:
Flashcards are hidden until you start studying
Study Notes
Hypophosphatemia
- Serum phosphorus levels < 1 mg/dl
- May cause growth retardation, RBC hemolysis, rhabdomyolysis, cardiomyopathy, insulin resistance, proximal myopathy
- Low phosphorus is a risk factor for rhabdomyolysis, but in the case of rhabdomyolysis, high phosphorus is observed.
- Only severe vitamin D deficiency, severe low calcium levels cause low phosphorus.
Causes of Hypophosphatemia
- Nutritional vitamin D dependent rickets
- Redistribution of phosphorus from blood to cells
- Insulin after DKA (diabetic ketoacidosis)
- Refeeding syndrome (most common metabolic abnormality - low phosphorus)
- Hungry bone syndrome
- Sepsis: Decreased calcium levels → decreased phosphorus levels
- Heat stroke
- Hyperthermia
Treatment
- Dialysis (best method)
- Treat associated hypocalcemia
- Restrict phosphorus intake
- Avoid foods rich in phosphorus such as dairy products, pickles, nuts, chocolate, and dates
Renal Causes
- Increased excretion
- Type II RTA (renal tubular acidosis)
- Hypophosphatemic rickets
- X-linked
- Autosomal recessive
- Autosomal dominant
Gene Mutation and Outcome
PatternGene mutationOutcomex linkedPHEX gene mutation - most commonDecreased cleavage of FGF 23Autosomal recessiveDMP mutationDecreased FGF 23Autosomal dominantFGF 23 mutationIncreased FGF 23
Autosomal Dominant Hypophosphatemic Rickets
- Lower limb predominant
- Low serum phosphorus (due to increased FGF 23)
- Increased ALP (alkaline phosphatase)
Tubular Injury
- Tumor induced osteomalacia (TIO): mesenchymal tumors → Gain of function mutation of FGF 23
Management
- Daily phosphorus requirement: 2 grams
- Mild hypophosphatemia: Oral Adphos tablets (250 mg)
- Low-fat milk (phosphorus content of 0.9 mg/ml)
- Severe hypophosphatemia: IV phosphorus (10 mg/kg over 12 hours)
Hyperphosphatemia
- Medial calcification in vessels
- Similar symptoms to hypocalcemia
Causes
- Excess phosphorus intake
- Phosphate-containing enema (most common)
- Decreased phosphorus excretion: renal failure or CKD (most common)
- Redistribution of phosphorus from cells to blood
- Rhabdomyolysis
- Hemolysis
- Tumor lysis syndrome
- Respiratory or metabolic acidosis
- Conditions producing 1α-hydroxylase
- Acromegaly
- Tumors (e.g., lymphomas)
- Sarcoid cells
- Granulomas
- Familial tumoral calcinosis:
- Autosomal recessive inheritance
- Missense mutation (loss of function) of FGF-23
Mechanism (Diagram)
- Stress → Cells → Phosphate
- Phosphate traps calcium
- Decreased serum calcium levels, Increased serum phosphorus levels
Phosphorus Excretion Impaired
- Increased phosphorus reabsorption
- Phosphorus traps calcium
Calcific masses (CaPO₄) features
- Most common in knee joint
- Presents like tumors
- Slow-growing soft tissue masses
- Calcification shows up on X-ray
Management
- Phosphate binders (increase calcium excretion)
- Examples: Sevalamer, Ferric citrate, Sucroferric oxyhydroxide
Phosphorus in Kidney Disease
- 99% of phosphorus is reabsorbed in the proximal convoluted tubule (PCT)
- Na⁺-P cotransporter (II A & II C - secondary active transport)
Types of Dysfunction
- Fanconi syndrome/Type II RTA/Proximal RTA:
- Generalized dysfunction of the PCT
- Severe phosphate depletion leads to bone mineral changes and severe rickets
- Chronic Kidney Disease (CKD):
- Can lead to increased phosphorus
- Early stages:
- FGF-23 → Na⁺-P cotransporter → Phosphaturia → Normal serum phosphorus
- Decreased calcium absorption due to impaired 1-alpha hydroxylase
- End stages (ESKD):
- FGF23 is inactivated (due to Klotho resistance)
- Increased Serum phosphorus
- Endothelial cell damage
- Osteoblast activation leads to medial calcification
- This can lead to the patient becoming unfit for renal transplant
Notes
- Vessel intimal calcification: Seen in atherosclerosis
- Parathyroid Hormone (PTH): Increased (PTH (+))
- Vitamin D: Increased (Vit D (+))
- FGF-23: Decreased (FGF-23 (-) in early stages, inactivated in end stages)
- Net effect of PTH and Vitamin D: Increases calcium (↑Ca²⁺) and decreases phosphorus (↓P)
- Osteoblasts: Secrete FGF-23 and sclerostin
Physiological Basis
Serum Phosphorus
- Hypophosphatemia: - 1-2.5 mg/dL: Asymptomatic. No RX needed - < 2.5 mg/dL : Symptomatic - < 4.5 mg/dL: Severe
- Forms
- Organic (intracellular): More
- Inorganic (HPO42-): Extracellular in blood. Predominantly used to measure serum phosphorus
Stores and Absorption
CalciumPhosphorusTotal body stores1200 g500-800 g% in:Bone99.3%85%Soft tissue0.6%14%Extracellular fluid0.1%1%% bound to albumin40%10%AbsorptionCa2+ + PO43-Vit D +calbindin (Vit D binding protein)Reabsorbed from jejunum 20% Net absorption% absorbed from GIT95% Active60% Net absorption 5% Passive 80% Active (with vit D) 20% Passive
Causes of Hypophosphatemia
- Intracellular redistribution
- DKA
- Hungry bone syndrome
- Refeeding
- Acute pancreatitis
- Decrease in calcium levels
- Decrease in magnesium levels
- Drugs:
- PPI
- Cisplatin, AGS
- Cetuximab
- Thiazides
- Inherited diseases:
- Gitelman syndrome: Na+-Cl- transporter defect
- Bartter syndrome: Na+-K+-2Cl- symport defect
- Hypomagnesemia: Claudin 16/19 defect
- Hypocalciuria, stones
- Isolated hypomagnesemia: TRPM6 defect
Symptoms
- Neuromuscular
- Increased glutamate mediated excitability → Seizures
- Vertical nystagmus
- CVS:
- Tachyarrhythmia
- ECG abnormalities
- Increased QT interval
- Polymorphic VT
- Torsades de pointes
Associated Conditions
- CVS
- MI (myocardial infarction)
- HTN (Hypertension)
- Electrolyte imbalance
- Decreased potassium levels (ROMK)
- Decreased calcium levels
- Other:
- Insulin resistance
- Migraine
- Colon cancer
Musculoskeletal
- Decrease in bone mass
ECG changes in hypomagnesemia
Treatment
- RDA: 420 mg (8.5 meq)/day
- Mild: 3 MgO tablets (140 mg each)
- Severe/arrhythmia:
- IV MgSO4
- Continue even after levels return to normal
- 1-2 mg rapidly over 2 minutes
- 4 g over next 24 hours
- Amiodaride/Triamterine maybe tried
- IV MgSO4
Magnesium Metabolism
Effect of Drugs
- Impaired GI absorption: Proton pump inhibitors (PPIs)
- Tubular injury:
- Cisplatin
- Aminoglycosides
- Calcineurin
- Defective transport pumps:
- Thiazide and loop diuretics
Hypermagnesemia
Causes
- Increased magnesium intake: Laxatives, purgatives, rectal enemas
- Renal failure: Decreased magnesium excretion
- Extracellular shift: Tumor lysis syndrome (TLS), Rhabdomyolysis, Hemolysis
- Acromegaly: Increased phosphate and calcium levels
- Familial hypocalciuric hypercalcemia: Loss of function of CaSR
- Addison's disease: Volume loss
- Pre-eclampsia therapy: Magnesium given as Rx
Symptoms
Blood Level (meq/L)Symptoms>72Cardiac arrest>10Flaccid quadriplegia, respiratory failure, hypocalcemia d/t PTH resistance, hypotension, bradycardia, decreased DTR (deep tendon reflex), flushing, headache, sluggish DTR.Arrhythmias: vague, no characteristic findings.6-104-6
Hypomagnesemia
Effect of Hypomagnesemia
- Decreased magnesium levels
- Patulous ROMK channel of THAL
- Potassium loss
- Decreased calcium levels
- Decreased PTH (parathyroid hormone)
- End organ resistance
- Patulous ROMK channel of THAL
- Always check serum magnesium levels in relation to potassium or calcium levels.
Treatment
- Dialysis: For Chronic Kidney Disease (CKD)
- Solute Toxicity: Calcium gluconate
Normal Levels
- 1.5 - 2.0 meq/L = 2.4 mg/dL
Gastrointestinal Absorption
- Site: Ileum (Along with bile acids)
- Transport
- Paracellular: 80-90%
- Transcellular: mediated by TRPM6, TRPM7
Kidney Absorption
SiteContributionPathwayTransportTHAL65%ParacellularPassivePCT25%ParacellularPassiveDCT10%TranscellularActive
- Net: 30%
- Inherited: Gitelman's syndrome
- Drug: Thiazide
ThAL (Thick Ascending Limb)
- Apical: EGF regulates TRPM6 (epidermal growth factor)
- Basolateral: Regulated by Na+, K+, 2Cl-
DCT (Distal convoluted tubule)
- Basolateral: Regulated by Na+, K+, 2Cl-
ThAL (Thick Ascending Limb)
- Apical surface:
- Blood calcium levels activate CaSR
- Na, K, 2Cl- pump opens
- Paracellular proteins (Claudin 16/19) drive calcium and magnesium reabsorption
- Calcium enters cells
- Basolateral surface:
- Disorders of Na, K, 2Cl- pump:
- Bartter Type 1: Hypercalciuria + Hypomagnesuria (80% patients)
- Disorders of Na, K, 2Cl- pump:
Mg2+^2+2+ transport in TAL & DCT (diagram)
- Visual representation of various channels and transporters involved in magnesium transport
Regulation
- Regulated by:
- Na+, K+, 2Cl-
- EGFR Pathway
Clinical implications:
- Decreased magnesium by: Cetuximab/Anticancer drugs --> Hypomagnesemia
Drugs
- Bisphosphonates
- Calcitonin
- Citrate
- Drugs causing tubular injury
Sequence of Ruling out Causes
- Decrease in serum calcium levels, check for corrected calcium levels to rule out
- Magnesium deficiency to rule out
Hungry Bone Syndrome
Ca2+Ca^{2+}Ca2+PO43−PO_4^{3-}PO43−PTHALPHungry Bone Syndrome↓↓↑(D/t matrix synthesis)Post op↓↑↓NormalHypoparathyroid↓↑↓Normal
Hypocalcemia
- Aminoglycosides
- Cisplatin
- Amphotericin &
- Hypoparathyroidism
- Other causes:
- Intravenous calcium (3-5 g/day) and magnesium (2-6 g/day) infusion with oral calcitriol (1-3 µg/day) supplementation
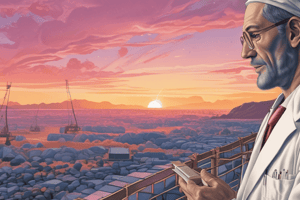
Zoledronate, Elcatonin, Parathyroidectomy
- Graph showing adjusted serum calcium and serum ALP levels over time after parathyroidectomy.
Pseudohypoparathyroidism (PHP)
Pathogenesis
- GNAS gene mutation → GSa defect → Resistance to PTH receptors.
Types
PHP Type IPHP Type IIPHP (Pseudo PHP)Ca2+Ca^{2+}Ca2+, S.PO43−S.PO_4^{3-}S.PO43−, S.PTHS.PTHS.PTH↑ ↑ ↑↓ ↓ ↓Normal.Resistance to PTH++-Response to PTH administration++-Resistance to others++-Albright's Hereditary Osteodystrophy (AHO)+-+GS α\alphaα receptors ↓in blood+ (maternal defect)-+ (paternal)CAMP levelsCompletePartialNormal
Albright's Hereditary Osteodystrophy (AHO)
- Characteristic feature: Short 4th metacarpal bone is longer than the metatarsal
- Associated findings: Short stature, round facies, and mental retardation.
Down's Syndrome
- Characteristic feature: Short 3rd metacarpal
- Associated findings: Knuckle Dimple Knuckle Knuckle sign.
Turner's Syndrome
- Characteristic feature: Short 4th metacarpal bone
- Associated findings: Knuckle Knuckle Dimple Knuckle sign.
Pseudohypoparathyroidism type 1a
- Characteristic feature: Short 4th and 5th metacarpal bones
- Associated findings: Knuckle Knuckle Dimple Dimple sign.
Normal
- Characteristic feature: Clenched fist has all knuckles.
Treatment of Acute Hypocalcemia
-
IV Infusion: 10 mL (1 amp) 10% Calcium Gluconate over 2-3 minutes. Administer 5 g in 500 mL of 5% Dextrose at 1-3 mg elemental calcium /kg/hr over 5 hours
-
Oral Calcium: Oral calcium supplements up to a certain amount per day
-
Images of hands and x-rays are included illustrating the physical features of each condition.
-
The diagrams show the location of knuckles and dimples on the hand.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.