Podcast
Questions and Answers
In a hypothetical scenario where a novel, highly virulent, and drug-resistant pathogen is identified in a dental clinic, necessitating a complete overhaul of existing disinfection protocols, which of the following strategies represents the MOST comprehensive and forward-thinking approach to ensure patient and staff safety?
In a hypothetical scenario where a novel, highly virulent, and drug-resistant pathogen is identified in a dental clinic, necessitating a complete overhaul of existing disinfection protocols, which of the following strategies represents the MOST comprehensive and forward-thinking approach to ensure patient and staff safety?
- Relying solely on enhanced barrier protection, such as the use of double barriers on all clinical contact surfaces, coupled with rigorous hand hygiene practices using alcohol-based hand rubs.
- Implementing a multi-tiered disinfection system, including UV-C irradiation, hydrogen peroxide vapor sterilization for enclosed spaces, and a switch to quaternary ammonium compounds with documented efficacy against the novel pathogen, alongside enhanced PPE protocols including powered air-purifying respirators (PAPRs). (correct)
- Increasing the concentration of currently used EPA-registered disinfectants by 20% and mandating double gloving for all procedures.
- Quarantine the dental clinic for a mandatory 3-days while using only an EPA-registered disinfectant.
Considering a dental surgery technician who has a known latex allergy, yet must frequently handle clinical contact surfaces and assist in procedures involving latex-containing materials, what preemptive strategy would MOST effectively mitigate the risk of an allergic reaction while maintaining optimal infection control standards?
Considering a dental surgery technician who has a known latex allergy, yet must frequently handle clinical contact surfaces and assist in procedures involving latex-containing materials, what preemptive strategy would MOST effectively mitigate the risk of an allergic reaction while maintaining optimal infection control standards?
- Rotating job duties to minimize contact with latex-containing materials, delegating such tasks to colleagues without latex allergies.
- Implementing a complete transition to nitrile or vinyl gloves for all personnel throughout the clinic, coupled with rigorous surface decontamination protocols to eliminate residual latex allergens and regular monitoring for any allergic symptoms among staff. (correct)
- Administering prophylactic antihistamines prior to each shift and relying on thorough handwashing after potential latex exposure.
- Applying a thick layer of petroleum-based barrier cream to the hands before donning latex gloves to minimize direct skin contact.
Envision a scenario where a dental clinic is located in an area with frequent water supply disruptions. What modification to standard environmental hygiene protocols is MOST crucial to ensure continuous and effective infection control?
Envision a scenario where a dental clinic is located in an area with frequent water supply disruptions. What modification to standard environmental hygiene protocols is MOST crucial to ensure continuous and effective infection control?
- Investing in a closed-loop water purification and recycling system with integrated antimicrobial treatment, coupled with the use of single-use disposable wipes pre-impregnated with an EPA-registered disinfectant and ensure proper function of the system through testing and strict quality control measures. (correct)
- Suspending all non-essential dental procedures until the water supply is restored to normal levels.
- Utilizing bottled water for hand hygiene and surface disinfection, prioritizing clinical areas over housekeeping surfaces to conserve resources.
- Stockpiling large quantities of pre-mixed disinfectant solutions and relying on dry surface wiping techniques to minimize water usage.
In a dental clinic aiming to minimize its environmental impact while upholding stringent hygiene standards, what innovative approach to waste disposal would be MOST effective in reducing the volume of regulated medical waste requiring special handling?
In a dental clinic aiming to minimize its environmental impact while upholding stringent hygiene standards, what innovative approach to waste disposal would be MOST effective in reducing the volume of regulated medical waste requiring special handling?
Suppose a dental surgery technician consistently experiences skin irritation despite adhering to recommended hand hygiene protocols. What advanced investigative step should be undertaken to determine the root cause of the irritation and implement targeted preventative measures?
Suppose a dental surgery technician consistently experiences skin irritation despite adhering to recommended hand hygiene protocols. What advanced investigative step should be undertaken to determine the root cause of the irritation and implement targeted preventative measures?
Flashcards
Environmental Hygiene
Environmental Hygiene
Maintaining cleanliness to prevent cross-contamination and infection spread in dental settings.
Surface Disinfection
Surface Disinfection
Cleaning and disinfecting surfaces after each patient using EPA-registered disinfectants.
Barrier Protection
Barrier Protection
Using FDA-approved barriers to cover clinical contact surfaces, changing them between patients.
Housekeeping Surfaces
Housekeeping Surfaces
Signup and view all the flashcards
Waste Disposal
Waste Disposal
Signup and view all the flashcards
Study Notes
- This unit emphasizes environmental hygiene, personal hygiene, and infection control.
- Dental surgery technicians need expertise in these areas to ensure the safety of patients and healthcare personnel.
Environmental Hygiene
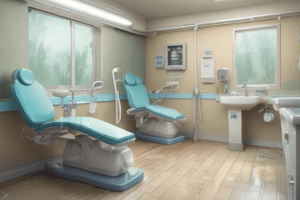
- Environmental hygiene in dental settings prevents cross-contamination and the spread of infections.
- Technicians must maintain a clean environment using strict cleaning and disinfection protocols.
Cleaning and Disinfecting Surfaces:
- Surfaces that contact patients/dental instruments should be cleaned/disinfected after each patient (e.g., light handles, chair switches, drawer knobs).
- EPA-registered disinfectants effective against bloodborne pathogens like HIV and HBV should be used.
- Use intermediate-level disinfectants with tuberculocidal claims on visibly contaminated surfaces like blood.
Barrier Protection:
- Clinical contact surfaces should be covered with FDA-approved surface barriers.
- Barriers should be changed between patients.
Housekeeping Surfaces:
- Floors, walls, and sinks should be cleaned regularly with soap and water or disinfected if visibly contaminated.
- Reusable cleaning materials like mops should be cleaned after use and dried before reuse.
Waste Disposal:
- Non-regulated medical waste, such as gloves and masks, can be disposed of as general waste.
- Regulated medical waste like blood-soaked gauze and used needles requires special handling and disposal in biohazard containers.
Personal Hygiene
- Personal hygiene is crucial for dental surgery technicians to minimize infection transmission.
- Proper hygiene protects healthcare workers and patients.
Hand Hygiene:
- Handwashing is the most important infection control measure.
- Hands should be washed before and after treating each patient.
- Also, wash hands before putting on gloves and immediately after removing them.
- Wash hands after touching potentially contaminated surfaces or instruments.
- Use soap and water or an alcohol-based hand rub for routine care if hands are not visibly soiled.
- A surgical hand scrub should be performed before donning sterile gloves for surgical procedures.
Personal Protective Equipment (PPE):
- Appropriate PPE, including gloves, masks, gowns, and protective eyewear, should be worn during all patient interactions.
- Change gloves between patients, remove them properly, and wash hands immediately.
- Gowns or laboratory coats should be changed if visibly soiled or at least daily.
Vaccination:
- Dental professionals should be vaccinated against common infectious diseases.
- Examples include hepatitis B, influenza, MMR (measles, mumps, rubella), chickenpox, and TDAP (tetanus, diphtheria, pertussis).
Infection Control
- Infection control measures prevent the spread of infections in dental settings.
- Dental surgery technicians must follow strict protocols to protect themselves and patients from infectious diseases.
Standard Precautions:
- Standard precautions apply to all patient care, regardless of infection status.
- These include hand hygiene, PPE (gloves, masks, eyewear), safe injection practices, proper handling of sharps, and instrument sterilization.
Sterilization of Instruments:
- All reusable dental instruments, like tweezers, chisels, and scrapers, must be sterilized between uses.
- Sterilization methods include autoclaving or using chemical sterilants, following manufacturer guidelines.
Respiratory Hygiene/Cough Etiquette:
- Patients with respiratory symptoms should be encouraged to cover their mouths/noses when coughing or sneezing.
- Provide tissues and no-touch receptacles for tissue disposal in waiting areas.
- Offer masks to symptomatic patients upon entry into the facility.
Sharps Safety:
- Use engineering controls like self-sheathing needles or needleless systems to reduce exposure risks.
- Dispose of all sharp objects in puncture-resistant containers labeled with biohazard symbols.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This lesson covers environmental and personal hygiene practices crucial for dental surgery technicians. It emphasizes cleaning, disinfection, and barrier protection to prevent cross-contamination and infection spread in dental settings, ensuring patient and staff safety.