Podcast
Questions and Answers
What is the primary organism associated with the development of cysts described in the context?
What is the primary organism associated with the development of cysts described in the context?
- Echinococcus granulosus (correct)
- Taenia saginata
- Diphyllobothrium latum
- Ascaris lumbricoides
Which sonographic appearance is characterized by a mother cyst containing daughter cysts?
Which sonographic appearance is characterized by a mother cyst containing daughter cysts?
- Mother cyst with peripherally placed daughter cysts (correct)
- Fluid collections with septa
- Solid-looking cysts with calcification
- Solitary cyst with calcification
What does the 'water-lily sign' represent in the context of cyst formation?
What does the 'water-lily sign' represent in the context of cyst formation?
- Presence of multiple daughter cysts
- Solid appearance of a cyst
- Detachment of the endocyst membrane (correct)
- Separation of cyst wall from pericyst
Which of the following is associated with the Casoni skin test?
Which of the following is associated with the Casoni skin test?
What appearance might a solid-looking cyst exhibit?
What appearance might a solid-looking cyst exhibit?
What is the main job of the liver?
What is the main job of the liver?
What do the umbilical vein and ductus venosus become after birth?
What do the umbilical vein and ductus venosus become after birth?
The liver is located primarily in the left hypochondrium.
The liver is located primarily in the left hypochondrium.
What can be indicated by a liver size greater than 15.5 cm?
What can be indicated by a liver size greater than 15.5 cm?
Match the following liver segments with their classifications:
Match the following liver segments with their classifications:
The liver receives its dual blood supply from the hepatic artery and the __________.
The liver receives its dual blood supply from the hepatic artery and the __________.
What does GGT indicate when increased?
What does GGT indicate when increased?
Which of the following is more specific for liver disease than AST?
Which of the following is more specific for liver disease than AST?
Prothrombin time is primarily affected by liver dysfunction or absence of vitamin K.
Prothrombin time is primarily affected by liver dysfunction or absence of vitamin K.
What are hepatocytes?
What are hepatocytes?
What is the main job of the liver?
What is the main job of the liver?
Which of the following structures carry oxygenated blood from the placenta to the fetus?
Which of the following structures carry oxygenated blood from the placenta to the fetus?
The umbilical vein remains open after birth.
The umbilical vein remains open after birth.
What is indicated by hepatomegaly?
What is indicated by hepatomegaly?
How many lobes does the liver have?
How many lobes does the liver have?
What does the hepatic artery branch off from?
What does the hepatic artery branch off from?
The main portal vein originates at the junction of the splenic vein and _____ vein.
The main portal vein originates at the junction of the splenic vein and _____ vein.
What is the function of Kupffer cells?
What is the function of Kupffer cells?
Which liver function test is considered more specific for liver disease?
Which liver function test is considered more specific for liver disease?
Alpha-fetoprotein (AFP) levels decrease during the first year of life.
Alpha-fetoprotein (AFP) levels decrease during the first year of life.
What can elevated GGT and ALP together indicate?
What can elevated GGT and ALP together indicate?
What is the main job of the liver?
What is the main job of the liver?
The umbilical vein carries deoxygenated blood from the placenta to the fetus.
The umbilical vein carries deoxygenated blood from the placenta to the fetus.
Which ligament is the remnant of the umbilical vein?
Which ligament is the remnant of the umbilical vein?
How many lobes does the liver have?
How many lobes does the liver have?
The right and left lobes of the liver are divided by a plane between the gallbladder and the ___.
The right and left lobes of the liver are divided by a plane between the gallbladder and the ___.
What is indicated by hepatomegaly?
What is indicated by hepatomegaly?
The liver receives a dual blood supply.
The liver receives a dual blood supply.
Which of the following is NOT a liver function test?
Which of the following is NOT a liver function test?
What does an increased level of Gamma Glutamyl Transpeptidase (GGT) indicate?
What does an increased level of Gamma Glutamyl Transpeptidase (GGT) indicate?
What is the normal upper limit size of the main portal vein (MPV)?
What is the normal upper limit size of the main portal vein (MPV)?
What does the liver produce in addition to filtering blood?
What does the liver produce in addition to filtering blood?
Match the following liver ligaments with their descriptions:
Match the following liver ligaments with their descriptions:
Flashcards are hidden until you start studying
Study Notes
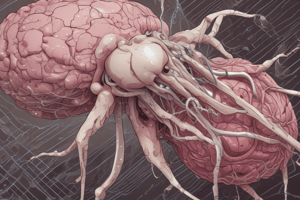
Hydatid Cysts
- Hydatid cysts are caused by the parasitic tapeworm Taenia echinococcus or Echinococcus granulosus.
- Larvae can invaginate and develop into encysted structures, leading to the formation of daughter cysts.
- Eventually, the original unilocular cyst becomes filled with numerous cysts of varying sizes.
- The sonographic appearance of hydatid cysts depends on the stage of larval maturation.
- A solitary cyst with possible mural or shell-like calcification is one possible appearance.
- Another possibility is a mother cyst containing internal, peripherally placed daughter cysts.
- Fluid collections with septa can create a honeycomb appearance.
- Solid-looking cysts, with or without calcification, are also possible.
- The "cyst within a cyst" or "water-lily sign" occurs when the endocyst membrane detaches, resulting in floating membranes within the pericyst.
- The Casoni skin test can be used to detect anti-echinococcus antibodies.
Liver Function
- The liver is responsible for filtering blood from the digestive tract.
- The liver detoxifies chemicals and metabolizes drugs.
- The liver secretes bile, which ends up back in the intestines.
- The liver makes proteins essential for blood clotting and other functions.
Embryology and Fetal Circulation
- The umbilical vein carries oxygenated blood from the placenta to the fetus.
- The umbilical vein ascends the fetal abdomen and courses towards the liver.
- A portion of the umbilical vein bypasses the liver via the ductus venosus.
- After birth, both the umbilical vein and ductus venosus close and exist as ligaments.
- The ligamentum teres is the remnant of the umbilical vein and runs from the umbilicus to the left portal vein.
- The ligamentum venosum is the remnant of the ductus venosus and runs from the left portal vein to the IVC.
Liver Location
- The liver is located in the right hypochondrium and epigastrium.
- The liver extends at variable degrees based on its size and shape into the left hypochondrium.
- The size and shape of the liver are determined by the lateral left segment and length of the right lobe.
Liver Size
- Measuring liver size by ultrasound can be difficult and subjective.
- Hepatomegaly is indicated in 75% of patients with a superior-inferior dimension greater than 15.5 cm.
- Hepatomegaly can be caused by infection, hepatic tumors, congenital or metabolic disorders.
- Reidel’s lobe is an inferior projection of the right lobe and can be mistaken for hepatomegaly.
Liver Anatomy
- The liver has 3 lobes: right, left, and caudate (the quadrate is the medial aspect of the left lobe).
- The liver is divided based on portal and hepatic vein distribution.
First Order Division
- The right and left hepatic lobes are divided by a plane between the gallbladder and the IVC.
- This plane marks the division of the main portal vein into its right and left branches.
Second Order Division
- The right and left lobes are further divided by hepatic veins into four separate parts (segments).
- The four segments are: left lateral (segments II & III), left medial (segments IVa & IVb), right anterior (segments V & VIII), and right posterior (segments VI & VII).
- The right lobe is supplied by the right portal vein.
- The left lobe is supplied by the left portal vein.
- The caudate lobe receives branches from both the right and left portal veins.
Third Order Division
- Hepatic veins divide the liver longitudinally into 4 parts/segments.
- Portal veins divide the liver transversely to create 8 segments.
- Segment I = Caudate Lobe
- Segment II = Left Lateral Superior
- Segment III = Left Lateral Inferior
- Segment IVa = Left Medial Superior
- Segment IVb = Left Medial Inferior
- Segment V = Right Anterior Inferior
- Segment VI = Right Posterior Inferior
Intersegmental / Intrasegmental Vessels
- Intersegmental vessels are hepatic veins.
- Hepatic veins course between the lobes and segments.
- Hepatic veins have no echogenic walls.
- Intrasegmental vessels are portal veins.
- Portal veins course to the center of each segment.
- Portal veins are encased by Glisson’s capsule, which gives them hyperechoic walls.
- The portal triad includes the main portal vein, proper hepatic artery, and common hepatic duct.
Liver Blood Supply
- The liver receives dual blood supply: hepatic arterial blood (oxygen-rich) and portal venous blood (nutrient-rich).
- Hepatic arterial blood accounts for 25% of blood supplied to the liver.
- Portal venous blood accounts for 75% of blood supplied to the liver.
- Portal vein and hepatic artery blood mixes in the liver sinusoids.
- Hepatic veins drain blood into the IVC.
Hepatic Artery
- The common hepatic artery branches off the celiac axis.
- The hepatic artery lies to the left of the CBD.
- The proper hepatic artery is the continuation of the common hepatic artery.
- Doppler demonstrates a low-resistance waveform in a normal hepatic artery.
- A post-operative liver transplant with a high-resistive hepatic artery suggests venous congestion of the liver or possible organ rejection.
- A parvus tardus hepatic artery suggests proximal anastomotic stenosis.
Portal Vein
- The MPV originates to the right midline at the junction of the splenic vein and the SMV.
- It courses superiorly towards the porta hepatis.
- The MPV divides into the LPV and RPV.
- Color Doppler is used to screen for direction of blood flow: hepatopetal (flow toward the liver) and hepatofugal (flow away from the liver).
- The portal vein should have a low velocity continuous flow toward the liver.
- The size of the PV is 13mm at its upper limits (range is 6-15mm).
- The MPV is anterior to the IVC and superior to the pancreatic head.
Hepatic Veins
- Hepatic veins drain into the superior aspect of the IVC.
- There are three hepatic veins: the right, middle, and left hepatic veins.
- Color Doppler shows blood flow toward the IVC and away from the transducer.
- The hepatic veins have a triphasic waveform.
Liver Ligaments
- The coronary ligament connects the posterior-superior liver surface to the diaphragm.
- The coronary ligament surrounds the bare area of the liver.
- The right and left triangular ligaments are formed by the upper and lower ends of the coronary ligaments.
- The ligamentum teres is the remnant of the umbilical vein.
- The falciform ligament separates the right and left lobes on the anterior surface of the liver.
Liver Echogenicity
- Normal liver is homogeneous and slightly hyperechoic compared to the normal renal cortex.
Liver Physiology
- The liver carries out over 500 functions.
- A single liver cell carries out diverse activities analogous to: a factory for many chemical compounds, a warehouse for storage, a power plant, a waste disposal plant, and a scientist that can regenerate tissue.
Liver Cell Types
- The liver has three types of cells: hepatocytes in the parenchyma, biliary epithelial cells lining the biliary system, and Kupffer cells lining the sinusoids.
Liver Function Tests
- Aspartate Aminotransferase (AST) / SGOT: present in various organs like the liver, heart, skeletal muscle, kidney, and brain; an increase is not specific for liver disease.
- Alanine Aminotransferase (ALT) / SGPT: more specific for liver disease than AST; present in high levels within liver tissue.
- Gamma Glutamyl Transpeptidase (GGT): present in hepatocytes and bile duct epithelium; increased levels indicate hepatocellular disease and biliary obstruction.
- Lactic Dehydrogenase (LDH): enzyme found in various body tissues; cellular damage causes an elevation in total serum LDH.
- Alpha Fetopretein (AFP): protein synthesized by the fetal liver; elevated levels are associated with hepatocellular carcinoma, germ cell tumors, metastatic liver disease, or hepatoblastoma in children.
- Platelets: contribute to hemostasis.
- Prothrombin Time (PT): a clotting factor used to diagnose unexplained bleeding or inappropriate blood clots.
- Partial Thromboplastin Time (PTT): characterizes blood coagulation and can detect abnormalities in clotting factors.
- INR: used to monitor patients on blood thinners like Warfarin.
- **PT, INR, PTT, and platelets are all monitored prior to an invasive procedure to ensure appropriate clotting factors.
Tumor Markers
- The tumor marker AFP is associated with hepatocellular carcinoma, germ cell tumors, and testicular cancer.
- The tumor marker HCG is associated with germ cell tumors and testicular cancer.
- The tumor marker CA-15-3 and CA 27-29 are associated with breast cancer.
- The tumor marker CA 125 is associated with ovarian, uterine, and lung cancer.
- The tumor marker PSA is associated with prostate cancer.
- The tumor marker CA 72-4 is associated with gastric, ovarian, and colorectal cancer.
- The tumor marker CA 19-9 is associated with pancreatic cancer, lung cancer, cholangiocarcinoma, colorectal cancer, and gastrointestinal cancer.
- The tumor marker CEA is associated with bile duct cancer, bladder cancer, uterine cancer, breast cancer, gastrointestinal cancer, esophageal cancer.
- The tumor marker Calcitonin is associated with medullary thyroid cancer.
- The tumor marker Lactate Dehydrogenase is associated with gastrointestinal cancer, germ cell tumors, bone cancer, liver disorders, colorectal cancer, lung cancer, and thyroid cancer.
- The tumor marker Alkaline Phosphatase is associated with bone cancer, liver disorders, colorectal cancer, lung cancer, and thyroid cancer.
Liver Function
- Liver filters blood from the digestive tract.
- It detoxifies chemicals and metabolizes drugs.
- The liver secretes bile which goes back to the intestines.
- The liver produces proteins important for blood clotting and other bodily functions.
Embryology & Fetal Circulation
- The umbilical vein carries oxygenated blood from the placenta to the fetus.
- The umbilical vein ascends the fetal abdomen and courses toward the liver (Paraumbilical vein-Portal sinus).
- A portion bypasses the liver via the ductus venosus.
- After birth, both veins close and exist as ligaments.
- The Ligament Teres is the remnant of the umbilical vein and runs from the umbilicus to the left portal vein.
- The Ligamentum Venosum is the remnant of the ductus venosus and runs from the left portal vein to the IVC, separating the left liver lobe from the right.
Liver Location
- The liver is located in the right hypochondrium and epigastrium.
- It can extend into the left hypochondrium depending on size and shape.
- The liver is described as irregular, hemispheric, and wedge-shaped.
Liver Size
- Liver size can be subjective and difficult to measure with ultrasound.
- It is measured superior-inferiorly at the mid-clavicular sagittal or coronal mid-axial plane.
- Hepatomegaly is indicated in 75% of patients with a superior-inferior dimension greater than 15.5 cm.
- Hepatomegaly can be caused by infection, hepatic tumors, congenital, or metabolic disorders.
- Reidel’s lobe is an inferior projection of the right lobe that can be mistaken for hepatomegaly when viewing the superior-inferior dimension of the liver.
Liver Anatomy
- The liver has three lobes: right, left, and caudate.
- The quadrate is the medial aspect of the left lobe.
- The liver is divided based on the distribution of the portal and hepatic veins.
- Anatomists, surgeons, and radiologists use different terminology to classify the liver.
Liver Anatomy: First Order Division
- The right and left lobes are divided by a plane between the gallbladder and the IVC.
- This plane marks the division of the main portal vein into its right and left branches.
Liver Anatomy: Second Order Division
- The right and left lobes are further divided by hepatic veins into four separate parts.
- These four segments represent the second-order division or second branching of the portal veins.
- The left lateral segment consists of segments II and III.
- The left medial segment consists of segments IVa and IVb.
- The right anterior segment consists of segments V and VIII.
- The right posterior segment consists of segments VI and VII.
Liver Anatomy: Third Order Division
- Hepatic veins divide the liver longitudinally into four segments.
- Portal veins divide the liver transversely, creating eight segments.
- Segment I is the caudate lobe.
- Segment II is the left lateral superior.
- Segment III is the left lateral inferior.
- Segment IVa is the left medial superior.
- Segment IVb is the left medial inferior.
- Segment V is the right anterior inferior.
- Segment VI is the right posterior inferior.
Intersegmental & Intrasegmental Vessels
- Intersegmental vessels are the hepatic veins.
- Hepatic veins course between the lobes and segments.
- Hepatic veins do not have echogenic walls.
Liver Blood Supply
- The liver receives dual blood supply: hepatic arterial blood and portal venous blood.
- Hepatic arterial blood is oxygen-rich and supplies 25% of the blood to the liver.
- Portal venous blood is nutrient-rich after leaving the gastrointestinal tract and supplies 75% of the blood to the liver.
- Blood from the portal vein and the hepatic arteries mixes in the liver sinusoids.
- Hepatic veins drain blood into the IVC.
Hepatic Artery
- The common hepatic artery branches off the celiac axis.
- The hepatic artery is located to the left of the CBD.
- It is anterior to the left portal vein and the main portal vein.
- The proper hepatic artery continues and terminates into the right, middle, and left branches.
- The caudate lobe receives branches from the right and left branches.
- The cystic artery arises from the right hepatic artery.
- Doppler demonstrates a low-resistance waveform in a normal hepatic artery.
- Post-operative liver transplant: a high-resistive hepatic artery suggests venous congestion of the liver or possible organ rejection.
- Parvus tardus hepatic artery suggests proximal anastomotic stenosis.
Portal Vein
- The MPV originates to the right midline at the junction of the splenic vein and SMV.
- It courses superiorly towards the porta hepatis.
- It divides into the LPV & RPV.
- Color Doppler is used to screen for the direction of blood flow: hepatopetal (flow towards the liver) or hepatofugal (flow away from the liver).
- The portal vein should have low-velocity, continuous flow toward the liver.
- Portal vein flow can increase after eating.
- The normal portal vein size is 6-15 mm.
- The MPV is anterior to the IVC and superior to the pancreatic body.
Hepatic Veins
- Hepatic veins drain into the superior aspect of the IVC.
- They include the RHV, MHV, and LHV.
- Scanning the anterior abdominal surface with color Doppler shows blood flow towards the IVC and away from the transducer.
- Hepatic veins have a triphasic waveform reflecting right atrial filling, contraction and relaxation.
Liver Ligaments
-
Coronary Ligament: Connects the posterior-superior liver surface to the diaphragm.
- Has anterior and posterior layers.
- Is highly reflective when visualized and suspends the liver from the diaphragm surrounding the bare area.
- It is continuous on each side of the right and left triangular ligaments and anteriorly with the falciform ligament.
-
Right & Left Triangular Ligament:
- Formed by the upper and lower ends of the coronary ligaments.
- Highly reflective when visualized and seen to the far right and left of the bare area.
-
Ligamentum Teres (round ligament): Remnant of the umbilical vein that runs from the umbilicus to the left portal vein.
- Recanalizes in cirrhosis to function as a venous collateral.
- Is highly reflective and appears round or triangular.
-
Falciform Ligament:
- Highly reflective when visualized.
- It’s a broad thin anterior-posterior fold of the parietal peritoneum separating the right and left lobes on the anterior surface of the liver.
Liver Echogenicity
- Normal liver:
- Homogeneous.
- Slightly hyperechoic compared to normal renal cortex.
- Signal amplitude is compared between structures.
### Liver Physiology
- The liver is essential to life with over 500 separate functions.
- A single liver cell carries out diverse activities.
- The liver is analogous to a:
- Factory for chemical compounds.
- Warehouse with short- and long-term storage capabilities.
- Power plant producing heat.
- Waste disposal plant.
- Scientist capable of regenerating tissue.
Liver Physiology: Cells
- Hepatocyte:
- The most abundant cell in the liver.
- Carries out most metabolic functions.
- Biliary epithelial cells:
- Line the biliary system, bile ducts, canaliculi, and gallbladder.
- Kupffer cells:
- Phagocytic cells belonging to the reticuloendothelial system.
- Line the sinusoids.
Liver Function Tests
- Aspartate Aminotransferase (AST) or SGOT:
- Present in the liver, heart, skeletal muscle, kidney, and brain.
- An elevated AST alone is nonspecific for liver disease; it's very sensitive and elevated in almost all significant hepatocellular disease.
- An elevated AST with a normal ALT is seen with myocardial infarction, heart failure, muscle injury, CNS disease, or other non-hepatic diseases.
- Alanine Aminotransferase (ALT) or SGPT:
- More specific to liver disease than AST.
- Found in high levels within the liver tissue.
- Elevated AST and LDH with a normal ALT rule out hepatic disease.
- Gamma Glutamyl Transpeptidase (GGT):
- Present in the hepatocytes and bile duct epithelium.
- Elevated levels indicate hepatocellular disease and biliary obstruction.
- Elevated in most diseases with acute damage to the liver and bile ducts.
- Elevated in patients with acute and chronic alcohol abuse.
- Elevated GGT and ALP= Biliary obstruction.
- Elevated GGT and ALT = Hepatocellular disease.
- Lactic Dehydrogenase (LDH):
- Enzyme found in many body tissues; cell damage causes elevation to total serum LDH.
- LDH4 and LDH5 are found in the liver, and can be found with cirrhosis and chronic viral hepatitis.
Liver Function Tests: Other
- Alpha Fetoprotein (AFP):
- Protein synthesized by the fetal liver.
- Levels decrease during the first year of life.
- Elevated levels are seen with:
- HCC (Hepatocellular carcinoma).
- Germ cell tumors in the testes and ovaries.
- Metastatic liver disease.
- Hepatoblastoma in children.
- Platelets:
- Contribute to hemostasis (the process of stopping bleeding at the site of interrupted endothelium).
- Low platelet concentration = thrombocytopenia.
- Elevated platelet concentration = thrombocytosis (can be congenital, reactive or unregulated production).
- Prothrombin Time (PT):
- Clotting factor affected by liver dysfunction or vitamin K deficiency.
- Helps diagnose unexplained bleeding or inappropriate blood clots.
- INR (International Normalized Ratio) monitors patients on blood thinners, such as Warfarin or Coumadin.
- Partial Thromboplastin Time (PTT):
- Identifies blood coagulation abnormalities apart from clotting factor defects.
- Used to monitor patients on Heparin.
- PT, INR, PTT, and platelets are all monitored prior to invasive procedures to ensure proper clotting factors.
Tumor Markers
- AFP: HCC, Germ cell tumors (Testicular Cancer)
- Calcitonin: Medullary Thyroid Cancer
- HCG: Germ Cell Tumor, Testicular cancer
- CA-15-3 & CA 27-29: Breast Cancer
- PSA: Prostate Cancer
- CA 125: Ovarian Cancer, Uterine Cancer
- LDH: Gastrointestinal Cancer, Germ cell tumor
- ALP: Bone Cancer, Liver disorders, Colorectal cancer, lung cancer, Thyroid cancer
- CEA (Carcinoembryonic antigen): Bile duct cancer, Bladder Cancer, Uterine cancer, Breast cancer, Gastrointestinal cancer, Esophageal cancer
- CA 72-4: Gastric Cancer, Ovarian Cancer
- CA 19-19: Pancreatic Cancer, Lung Cancer, Cholangiocarcinoma, Colorectal Cancer, Gastrointestinal Cancer
Liver Function
- The liver is the main filter for blood coming from the digestive tract.
- It detoxifies chemicals and metabolizes drugs.
- The liver secretes bile, which goes back to the intestines.
- It makes proteins important for blood clotting and various other functions.
Embryology - Fetal Circulation
- The umbilical vein carries oxygenated blood from the placenta to the fetus.
- It travels up the fetal abdomen towards the liver (Paraumbilical vein - Portal sinus).
- Some blood bypasses the liver via the ductus venosus.
- After birth, both the umbilical vein and ductus venosus close and become ligaments.
- Ligamentum Teres is a remnant of the umbilical vein, connecting the umbilicus to the left portal vein.
- Ligamentum Venosum is a remnant of the ductus venosus, connecting the left portal vein to the IVC. It separates the left lobe of the liver from the right lobe.
Liver Location
- The liver is located in the right hypochondrium and epigastrium.
- It can extend, depending on size and shape, into the left hypochondrium.
- The lateral left segment and the length of the right lobe influence its contour and shape.
- The liver can be described as irregular, hemispheric, or wedge-shaped.
Liver Size
- Liver size measured by ultrasound can be difficult and subjective due to limitations in field of view and measuring techniques.
- The liver's size is measured superior-inferiorly at the mid-clavicular sagittal or coronal mid-axial plane.
- Hepatomegaly is indicated when the superior-inferior dimension exceeds 15.5 cm in 75% of patients.
- Hepatomegaly can be caused by infections, tumors, congenital or metabolic disorders such as hepatitis, polycystic liver disease, non-alcoholic fatty liver disease (NAFLD), and Riedel's lobe.
- Riedel's lobe is an inferior projection of the right lobe and can be mistaken for hepatomegaly in a superior-inferior view of the liver.
Liver Anatomy
- The liver has three lobes: right, left, and caudate. The quadarte lobe is the medial aspect of the left lobe.
- The liver's divisions are based on the distribution of the portal and hepatic veins.
- Different anatomical terminology can be used by anatomists, surgeons, and radiologists.
- We use functional liver anatomy, describing the liver as a first-order, second-order, and third-order division:
- Halves: Right & Left
- Lobes: Right, Left, Caudate
- Divisions: Sectors, Segments, Subsegments
First Order Division - Lobar/Hemiliver Anatomy
- The right and left lobes are divided by a plane between the gallbladder and the IVC.
- This plane marks the division of the main portal vein into its right and left branches.
Second Order Division - Portal Vein Branching
- The right and left lobes are further divided by hepatic veins into four separate parts (segments).
- Left Lateral: Segments II & III
- Left Medial: Segments IVa & IVb
- Right Anterior: Segments V & VIII
- Right Posterior: Segments VI & VII
Third Order Division - Portal Vein Branching
- Hepatic veins divide the liver vertically into four parts/segments.
- Portal veins divide the liver horizontally, creating eight segments.
- Segment I: Caudate Lobe
- Segment II: Left Lateral Superior
- Segment III: Left Lateral Inferior
- Segment IVa: Left Medial Superior
- Segment IVb: Left Medial Inferior
- Segment V: Right Anterior Inferior
- Segment VI: Right Posterior Inferior
- Segment VII: Right Posterior Superior
- Segment VIII: Right Anterior Superior
Intersegmental and Intrasegmental Vessels
- Intersegmental: Hepatic veins course between lobes and segments, both interlobar and intersegmental. These veins have no echogenic walls.
- Intrasegmental: Portal veins course towards the center of each segment. They are encased by Glisson's Capsule, a fibrofatty sheath, resulting in hyperechoic walls.
- The portal triad, consisting of the main portal vein, proper hepatic artery, and common hepatic duct, is all surrounded by Glisson's Capsule.
Liver Blood Supply
- The liver receives a dual blood supply:
- Hepatic Arterial Blood: Oxygen-rich, providing 25% of the liver's blood supply.
- Portal Venous Blood: Nutrient-rich, delivering 75% of the liver's blood supply, coming from the walls of the gastrointestinal tract.
- Blood from both the portal vein and hepatic arteries mixes in the liver sinusoids.
- Hepatic veins drain blood into the IVC.
Hepatic Artery
- It branches off the celiac axis.
- It is located to the left of the common bile duct (CBD) and anterior to the left and main portal vein.
- The proper hepatic artery continues and terminates into the right, middle, and left hepatic artery.
- The caudate receives blood supply from both the right and left branches.
- The cystic artery arises from the right hepatic artery.
- Doppler demonstrates a low-resistance waveform in a normal hepatic artery.
- In a post-liver transplant, a high-resistive waveform suggests venous congestion within the liver or possible organ rejection.
- A "parvus tardus" waveform suggests proximal anastomotic stenosis.
Portal Vein
- The main portal vein (MPV) originates at the right midline at the junction of the splenic vein and superior mesenteric vein (SMV).
- It courses upwards towards the porta hepatis.
- It then divides into the left portal vein (LPV) and the right portal vein (RPV).
- Color Doppler is used to screen for blood flow direction:
- Hepatopetal: Flow towards the liver.
- Hepatofugal: Flow away from the liver.
- The portal vein should demonstrate continuous low-velocity flow towards the liver. Increased flow can occur after eating.
- The MPV is typically anterior to the IVC and superior to the pancreatic head.
- The upper size limit of the portal vein is 13 mm (range: 6-15 mm).
Hepatic Veins
- They drain into the superior aspect of the IVC.
- The three main hepatic veins are: right hepatic vein (RHV), middle hepatic vein (MHV), and left hepatic vein (LHV).
- When scanning the anterior abdominal surface, color Doppler shows blood flow towards the IVC and away from the transducer.
- The waveform is triphasic, reflecting right atrial filling, contraction, and relaxation.
Liver Ligaments
- Coronary Ligament: Connects the posterior-superior liver surface to the diaphragm. It has anterior and posterior layers.
- It is highly reflective when visualized and suspends the liver from the diaphragm, surrounding the bare area.
- It is continuous on each side of the right and left triangular ligaments and anteriorly with the falciform ligament.
- Right & Left Triangular Ligament: Formed by the upper and lower ends of the coronary ligaments. These are also highly reflective when visualized and are seen to the far right and left of the bare area.
- Ligamentum Teres: Also known as the round ligament, it is a remnant of the umbilical vein extending from the umbilicus to the left portal vein.
- It can recanalize in cirrhosis to function as a venous collateral.
- It is highly reflective, appearing round or as a triangular shape.
- Falciform Ligament: Is a highly reflective broad, thin, anterior-posterior fold of the parietal peritoneum. It separates the right and left lobes on the anterior surface.
Liver Echogenicity
- Normal Liver:
- Homogeneous in appearance.
- Slightly hyperechoic compared to the normal renal cortex.
- Signal amplitudes should be compared between different structures.
- HYPERechoic: Renal sinus, pancreas
- HYPOechoic: Spleen, liver, renal cortex
Liver Physiology
- The liver has a vital role in maintaining life, performing over 500 separate activities.
- A single liver cell carries out a diverse range of functions, akin to:
- A factory for various chemical compounds.
- A warehouse with short-term and long-term storage capabilities.
- A power plant producing heat.
- A waste disposal plant excreting waste.
- A scientist capable of tissue regeneration when not too severely damaged.
Liver Physiology - Cells
- Three types of cells contribute to liver function:
- Hepatocytes: The most abundant cell, carrying out most metabolic functions.
- Biliary Epithelial Cells: Line the biliary system, including bile ducts, canaliculi, and gallbladder.
- Kupffer Cells: Phagocytic cells belonging to the reticuloendothelial system. They line the sinusoids.
Liver Function Tests
- Aspartate Aminotransferase (AST) / SGOT: Found in the liver, heart, skeletal muscle, kidney, and brain. An increase in AST alone is non-specific for liver disease, though it is sensitive and elevated in almost all significant hepatocellular diseases. An elevated AST without an elevated ALT may indicate myocardial infarction, heart failure, muscle injury, CNS disease, or other non-hepatic conditions. AST and ALT are usually elevated in most liver diseases, with higher values more typical of viral hepatitis.
- Alanine Aminotransferase (ALT) / SGPT: More specific for liver disease than AST. Present in high levels within liver tissue. An elevated AST and LDH with a normal ALT rules out hepatic disease.
- Gamma Glutamyl Transpeptidase (GGT): Located in hepatocytes and bile duct epithelium. An increase suggests hepatocellular disease and biliary obstruction. Elevated in most liver diseases with acute damage to liver and bile ducts. Also elevated in patients with acute and chronic alcohol abuse.
- GGT + ALP: Biliary obstruction
- GGT + ALT: Hepatocellular disease
- Lactic Dehydrogenase (LDH): An enzyme found in cells of many body tissues. Elevated levels are due to cellular damage. LDH4 and LDH5 are found in the liver. Elevated levels can indicate cirrhosis and chronic viral hepatitis.
- Alpha Fetoprotein (AFP): A protein synthesized by the fetal liver, decreasing during the first year of life. Elevated levels can be seen in:
- Hepatocellular carcinoma (HCC).
- Germ cell tumors in the testes and ovaries.
- Metastatic liver disease.
- Hepatoblastoma in children.
- Platelets: Contribute to hemostasis. Low platelet concentration is known as thrombocytopenia. Elevated platelet concentration is called thrombocytosis.
- Prothrombin Time (PT): A clotting factor. Elevated levels indicate liver dysfunction or vitamin K deficiency. Used to diagnose unexplained bleeding or unusual blood clots. The international normalized ratio (INR) helps monitor patients on blood thinners like Warfarin or Coumadin.
- Partial Thromboplastin Time (PTT): Measures blood coagulation separate from abnormalities in clotting factors. Used to monitor patients on Heparin.
- PT, INR, PTT, and Platelets: These tests are monitored before invasive procedures to ensure adequate clotting factors.
Tumor Markers
- AFP: Hepatocellular carcinoma (HCC), germ cell tumors (testicular cancer)
- HCG: Germ cell tumors, testicular cancer
- CA 15-3 & CA 27-29: Breast Cancer
- PSA: Prostate Cancer
- CA 125: Ovarian Cancer, Uterine Cancer
- CA 72-4: Gastric Cancer, Ovarian Cancer, Colorectal Cancer, Pancreatic Cancer, Lung cancer, Cholangiocarcinoma
- CEA: (Carcinoembryonic Antigen): Bile duct cancer, Bladder cancer, Uterine cancer, Breast cancer, Gastrointestinal cancer, Esophageal cancer
- CA 19-9: Pancreatic Cancer, Lung cancer, Cholangiocarcinoma, Colorectal cancer, Gastric cancer
- Calcitonin: Medullary thyroid cancer
- Lactate Dehydrogenase: Gastrointestinal cancer, germ cell tumor
- Alkaline Phosphatase: Bone cancer, liver disorders, colorectal cancer, lung cancer, thyroid cancer
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.