Podcast
Questions and Answers
What initiates the relaxation of the internal urethral sphincter during the micturition reflex?
What initiates the relaxation of the internal urethral sphincter during the micturition reflex?
- Stimulation of the pontine micturition center
- Increased bladder volume (correct)
- Activation of the spinal reflex
- Contraction of the external urethral sphincter
Which term describes excessive urine production often related to metabolic issues?
Which term describes excessive urine production often related to metabolic issues?
- Polyuria (correct)
- Anuria
- Oliguria
- Hydroureter
What is indicated by a daily urine output of 0-50 mL?
What is indicated by a daily urine output of 0-50 mL?
- Polyuria
- Normal kidney function
- Anuria (correct)
- Oliguria
Which substance would NOT typically be present in a normal urinalysis?
Which substance would NOT typically be present in a normal urinalysis?
Which reflex blocks urination until it is consciously relaxed during the micturition process?
Which reflex blocks urination until it is consciously relaxed during the micturition process?
What is a common cause of urinary retention in males?
What is a common cause of urinary retention in males?
Which type of incontinence involves the inability to delay urination?
Which type of incontinence involves the inability to delay urination?
Which symptom is specifically associated with urinary bladder disorders?
Which symptom is specifically associated with urinary bladder disorders?
What condition is characterized by pain in the flank radiating to the upper quadrants?
What condition is characterized by pain in the flank radiating to the upper quadrants?
What underlying issue can cause increased urgency or frequency of urination?
What underlying issue can cause increased urgency or frequency of urination?
What is the main purpose of countercurrent multiplication in the nephron?
What is the main purpose of countercurrent multiplication in the nephron?
Which part of the nephron is primarily responsible for the reabsorption of water?
Which part of the nephron is primarily responsible for the reabsorption of water?
What is the primary function of the nephron loop in urine concentration?
What is the primary function of the nephron loop in urine concentration?
How does the thick ascending limb of the nephron contribute to the concentration gradient?
How does the thick ascending limb of the nephron contribute to the concentration gradient?
Where does obligatory water reabsorption primarily occur?
Where does obligatory water reabsorption primarily occur?
What effect does countercurrent multiplication have on urine concentration?
What effect does countercurrent multiplication have on urine concentration?
What characterizes the thin descending limb of the loop of Henle?
What characterizes the thin descending limb of the loop of Henle?
What effect does ADH (antidiuretic hormone) have on urine volume?
What effect does ADH (antidiuretic hormone) have on urine volume?
Which fluid surrounds the ascending and descending limbs of the nephron, facilitating countercurrent multiplication?
Which fluid surrounds the ascending and descending limbs of the nephron, facilitating countercurrent multiplication?
Which statement accurately describes facultative water reabsorption?
Which statement accurately describes facultative water reabsorption?
What is the typical urea concentration in the tubular fluid when it reaches the papillary duct?
What is the typical urea concentration in the tubular fluid when it reaches the papillary duct?
What would likely happen if Na+ and Cl– transport in the thick ascending limb were inhibited?
What would likely happen if Na+ and Cl– transport in the thick ascending limb were inhibited?
How much filtrate is recovered during obligatory water reabsorption?
How much filtrate is recovered during obligatory water reabsorption?
Which statement accurately describes the transport mechanisms in the thick ascending limb?
Which statement accurately describes the transport mechanisms in the thick ascending limb?
What role does the collecting duct's papillary region play in the medullary ion gradient?
What role does the collecting duct's papillary region play in the medullary ion gradient?
What occurs in the absence of ADH in the DCT and collecting tubule?
What occurs in the absence of ADH in the DCT and collecting tubule?
What effect does the ascending limb of the nephron loop have on the osmotic concentration of tubular fluid?
What effect does the ascending limb of the nephron loop have on the osmotic concentration of tubular fluid?
What is the primary function of the collecting duct in urine concentration?
What is the primary function of the collecting duct in urine concentration?
What role does the vasa recta play in the renal system?
What role does the vasa recta play in the renal system?
Which of the following statements about renal failure is false?
Which of the following statements about renal failure is false?
What is a key characteristic of the distal convoluted tubule (DCT)?
What is a key characteristic of the distal convoluted tubule (DCT)?
How does renal failure typically impact the body's systems?
How does renal failure typically impact the body's systems?
What is the consequence of the ascending limb's impermeability to water?
What is the consequence of the ascending limb's impermeability to water?
What ultimately happens to urine as it passes through the collecting duct?
What ultimately happens to urine as it passes through the collecting duct?
What type of epithelium lines the neck of the urethra?
What type of epithelium lines the neck of the urethra?
Which structure is involved in voluntary control of urination?
Which structure is involved in voluntary control of urination?
What initiates the afferent impulses that trigger the micturition reflex?
What initiates the afferent impulses that trigger the micturition reflex?
Upon bladder distension, which nerve activity is increased to promote urine storage?
Upon bladder distension, which nerve activity is increased to promote urine storage?
What is the primary function of the thick, elastic lamina propria in the urethra?
What is the primary function of the thick, elastic lamina propria in the urethra?
Which response is NOT part of the spinal reflex involved in urine storage?
Which response is NOT part of the spinal reflex involved in urine storage?
What role do mucin-secreting cells in the urethra play?
What role do mucin-secreting cells in the urethra play?
What is the effect of stretching receptors in the urinary bladder as it fills?
What is the effect of stretching receptors in the urinary bladder as it fills?
Flashcards
Countercurrent Multiplication
Countercurrent Multiplication
The process by which the descending and ascending limbs of the nephron create a concentration gradient in the renal medulla.
Descending Limb of the Loop of Henle
Descending Limb of the Loop of Henle
The part of the nephron that is permeable to water but impermeable to solutes. As water moves out, the tubular fluid becomes increasingly concentrated.
Ascending Limb of the Loop of Henle
Ascending Limb of the Loop of Henle
The part of the nephron that actively pumps sodium (Na+) and chloride (Cl-) out of the tubular fluid, creating a concentration gradient. It is impermeable to water.
Peritubular Fluid
Peritubular Fluid
Signup and view all the flashcards
Water Reabsorption in the Medulla
Water Reabsorption in the Medulla
Signup and view all the flashcards
Urine Concentration
Urine Concentration
Signup and view all the flashcards
Medullary Ion Gradient
Medullary Ion Gradient
Signup and view all the flashcards
Active Ion Pumping
Active Ion Pumping
Signup and view all the flashcards
Water Reabsorption
Water Reabsorption
Signup and view all the flashcards
Descending Limb of Nephron Loop
Descending Limb of Nephron Loop
Signup and view all the flashcards
Ascending Limb of Nephron Loop
Ascending Limb of Nephron Loop
Signup and view all the flashcards
Collecting Duct
Collecting Duct
Signup and view all the flashcards
Obligatory Water Reabsorption
Obligatory Water Reabsorption
Signup and view all the flashcards
Facultative Water Reabsorption
Facultative Water Reabsorption
Signup and view all the flashcards
How does the Ascending Limb contribute to urine concentration?
How does the Ascending Limb contribute to urine concentration?
Signup and view all the flashcards
What role does the vasa recta play in urine concentration?
What role does the vasa recta play in urine concentration?
Signup and view all the flashcards
How do the DCT and collecting system influence urine concentration?
How do the DCT and collecting system influence urine concentration?
Signup and view all the flashcards
What is the key principle behind urine concentration in the collecting duct?
What is the key principle behind urine concentration in the collecting duct?
Signup and view all the flashcards
What is the medullary ion gradient and why is it important?
What is the medullary ion gradient and why is it important?
Signup and view all the flashcards
Define renal failure.
Define renal failure.
Signup and view all the flashcards
How does renal failure lead to anemia?
How does renal failure lead to anemia?
Signup and view all the flashcards
How does renal failure affect the central nervous system?
How does renal failure affect the central nervous system?
Signup and view all the flashcards
Micturation Reflex
Micturation Reflex
Signup and view all the flashcards
Pontine Micturition Center
Pontine Micturition Center
Signup and view all the flashcards
Polyuria
Polyuria
Signup and view all the flashcards
Oliguria
Oliguria
Signup and view all the flashcards
Anuria
Anuria
Signup and view all the flashcards
Urinary frequency
Urinary frequency
Signup and view all the flashcards
Urinary incontinence
Urinary incontinence
Signup and view all the flashcards
Urinary retention
Urinary retention
Signup and view all the flashcards
Pain in the superior pubic region
Pain in the superior pubic region
Signup and view all the flashcards
Voluntary Urination
Voluntary Urination
Signup and view all the flashcards
Pontine Storage Center
Pontine Storage Center
Signup and view all the flashcards
Spinal Reflex (Storage)
Spinal Reflex (Storage)
Signup and view all the flashcards
Detrusor Muscle Contraction
Detrusor Muscle Contraction
Signup and view all the flashcards
Urination (Voiding)
Urination (Voiding)
Signup and view all the flashcards
Internal Urethral Sphincter
Internal Urethral Sphincter
Signup and view all the flashcards
External Urethral Sphincter
External Urethral Sphincter
Signup and view all the flashcards
Stretch Receptors
Stretch Receptors
Signup and view all the flashcards
Study Notes
Urinary (Renal) System - Nephron Physiology and Urination
- The urinary system, also known as the renal system, is responsible for urine production and excretion.
- The nephron is the functional unit of the kidney.
- Nephron processes include filtration, reabsorption, secretion, and excretion.
- Excretion = Filtration - Reabsorption + Secretion
Nephron locations of water and ion reabsorption
- The concentration of ions in the cortex is consistent (~300 mmol/L).
- There is an ion concentration gradient in the medulla, with higher concentrations at the distal end (~1200 mmol/L), decreasing towards the top (~400 mmol/L).
- The gradient is actively maintained to maximize water reabsorption at specific nephron sections.
Nephron locations of water and ion reabsorption (continued)
- Salt, water, and glucose are passively reabsorbed in the cortex by the proximal convoluted tubule (PCT) (60-80%).
- The medullary part maximizes passive water reabsorption driven by the concentration gradient.
- The ascending and descending limbs of the loop of Henle play a vital role in creating the medulla's high osmolarity.
- Active ion transport in the ascending limb maintains the gradient.
Medullary Osmotic Gradient
- The medulla's high osmolarity plays a critical role in maximizing water reabsorption, supporting dehydration survival.
- The descending limb is permeable to water, not solutes.
- The ascending limb is impermeable to water, permeable to solutes.
Countercurrent Multiplication
- The nephron loops use a countercurrent multiplication mechanism.
- Tubular fluids flow in opposite directions creating a concentration gradient.
- This gradient maximizes water reabsorption, leading to concentrated urine.
Variable Reabsorption from the Loop of Henle - Countercurrent Multiplier
- Thin descending limb is permeable to water, impermeable to solutes, and solute concentration increases.
- Thick ascending limb is impermeable to water, selectively permeable to Na+ and Cl-, and solute concentration decreases.
- Active ion transport (Na+ and Cl−) in the thick ascending limb helps maintain the medullary osmotic gradient.
Nephron Loop - Descending vs Ascending Limb
- The descending limb is permeable to water but not to solutes; water moves from the tubular fluid to the peritubular fluid by osmosis.
- The ascending limb actively transports Na+ and Cl− out of the tubular fluid, maintaining the medullary osmotic gradient.
Putting it All Together - Counter Current Multiplier
- Most water and solutes absorbed from the PCT in the cortex are redistributed back to the circulation from afferent arterioles.
- Water absorbed in the medulla is via the descending limb and redistributed back to circulation via the vasa recta of the peritubular capillaries.
- Tubular fluid is concentrated because water is removed creating a concentrated urine.
Nephron loop - Concentrates Urine and Maximizes Water Reabsorption
- Water is variably reabsorbed along the distal convoluted tubule (DCT) and collecting duct in relation to blood pressure.
- The papillary region of the collecting duct helps maintain the medullary ion gradient.
- Typical urea concentration in the papillary duct is 450 mols/L.
Urine Volume and Concentration
- Urine volume and concentration can be regulated to manage blood pressure hormonally.
- Obligatory water reabsorption occurs in the PCT and descending limb.
- Facultative water reabsorption occurs in the DCT and collecting duct.
Urine volume without ADH (antidiuretic hormone)
- No water is reabsorbed in the DCT and collecting tubule.
- No facultative water reabsorption occurs.
Urine volume with ADH
- ADH (antidiuretic hormone) allows water channels (aquaporins) to form in the apical plasma membranes of DCT and collecting tubule cells.
- Water permeability of the last tubular segments is increased; increasing water reabsorption.
Normal Urine Volume and Concentration
- Normal urine volume is about 1200 mL/day.
- Normal urine has an osmotic concentration of 1000 mOsm/L.
- Values differ among individuals.
- Kidneys adapt their function to maintain homeostasis.
Renal Function
- Kidneys filter wastes from blood and maintain homeostasis.
- Impairment causes reduced urine production, elevated blood pressure, anemia, and central nervous system problems.
Chronic Renal Failure
- Kidney function deteriorates gradually.
- Progression can be slowed, but the condition is irreversible.
- Minimizing urine volume through restricted fluid, salt, and protein intake is a management technique.
- Acidosis is a common problem with renal failure.
Acute Renal Failure
- Kidneys may be impaired for weeks following rapid deterioration of function.
- It can be caused by exposure to toxic drugs, infection, renal ischemia, or blockage.
Renal Failure - Chronic Treatment: Dialysis
- Dialysis is a process of passive diffusion across a selectively permeable membrane.
- Hemodialysis uses an artificial membrane to mimic kidney function and regulate blood composition.
- Shunts connect blood vessels with the dialysis machine allowing efficient filtration of blood and regulation of solute concentrations.
Renal Failure - Transplant
- Kidney transplant is the only real cure for severe renal failure.
- Patient survival is typically >90% at two years.
- Close relatives are preferred donors.
- Immunosuppressive drugs are necessary to reduce transplant rejection.
Urinary tract (Post Kidney Functions)
- The urinary tract, including the ureters, bladder, and urethra, encompasses urine transport, storage, and elimination.
- Imaging with a pyelogram—an X-ray of the urinary tract—can visualize the tract after a radiopaque dye is administered intravenously.
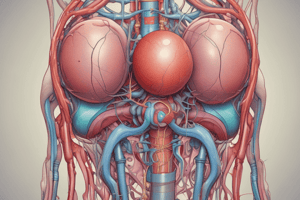
Urinary tract Anatomy (Ureters)
- Paired muscular tubes, approximately 30 cm long, connecting the kidneys to the urinary bladder.
- Retroperitoneal and attached to the posterior abdominal wall.
Urinary tract Anatomy (Urinary Bladder)
- A hollow muscular organ that holds urine.
- Rugae (folds in the bladder lining) allow the bladder to expand.
- Ureteral orifices are slit-like structures in the bladder that prevent urine back-flow.
Urinary tract Anatomy (Urethra)
- The urethra extends from the urinary bladder to the body exterior.
- Different lengths and functions differentiate male and female urethras.
The ureters, urinary bladder, and urethra functions
- Ureters conduct urine from the kidneys to the bladder.
- The bladder stores urine until urination occurs.
- The urethra carries urine out of the body.
Conduction and storage of urine (Wall of the urinary bladder)
- Mucosa, submucosa, and muscularis layers constitute the urinary bladder wall.
- The muscularis layer is made of three layers of smooth muscle (collectively detrusor muscle).
Conduction and storage of urine (Wall of the urethra)
- The urethra's wall has a thick, elastic lamina propria (a layer of connective tissue).
- Longitudinal mucous membrane folds are present.
- Mucin-secreting cells are found within epithelial pockets.
- Lined with stratified epithelium.
Urinary reflexes coordinate Urine storage & Urination
- Micturation reflexes coordinate urine storage and urination.
- These reflexes involve afferent sensory and efferent motor responses involving two anatomical regions (spinal reflex and pontine storage center).
- The spinal reflex involves the stretch receptors, sympathetic stimulation to the bladder's detrusor muscle, and internal urethral sphincter contraction to hold urine.
- The pontine storage center, within the brain stem, controls conscious bladder emptying.
Clinical Module: Urinary disorders
- Changes in urine volume and appearance can indicate underlying urinary disorders.
- Polyuria is excessive urine production.
- Oliguria is reduced urine production (50-500 mL/day).
- Anuria is severely reduced urine production (<50 mL/day).
- Urine analysis can identify urinary disorders by assessing characteristics such as volume, appearance, and chemical composition.
Other signs of Urinary disorders
- Urinary disorders can present with varying symptoms, including changes in frequency (increased urgency or frequency), incontinence (difficulty controlling urination), pain in the superior pubic region or lumbar region, and urinary retention (difficulty urinating).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.