Podcast
Questions and Answers
What is the most important risk factor for the development of a catheter-associated UTI (CAUTI)?
What is the most important risk factor for the development of a catheter-associated UTI (CAUTI)?
Which of the following is NOT a commonly accepted indication for the insertion of a urinary catheter?
Which of the following is NOT a commonly accepted indication for the insertion of a urinary catheter?
What should be prioritized to reduce the risk of catheter-associated UTIs?
What should be prioritized to reduce the risk of catheter-associated UTIs?
Which of the following scenarios would be a valid indication for catheterization?
Which of the following scenarios would be a valid indication for catheterization?
Signup and view all the answers
Which condition is a contraindication for urinary catheter use?
Which condition is a contraindication for urinary catheter use?
Signup and view all the answers
What happens when urinary retention progresses?
What happens when urinary retention progresses?
Signup and view all the answers
Which of the following can cause acute urinary retention?
Which of the following can cause acute urinary retention?
Signup and view all the answers
What key sign indicates acute urinary retention?
What key sign indicates acute urinary retention?
Signup and view all the answers
What is a potential complication of bladder distension in individuals with spinal cord injury above T6?
What is a potential complication of bladder distension in individuals with spinal cord injury above T6?
Signup and view all the answers
Which condition is likely to lead to chronic urinary retention in individuals with male genitalia?
Which condition is likely to lead to chronic urinary retention in individuals with male genitalia?
Signup and view all the answers
What is an effect of general and regional anesthetics on the urinary system?
What is an effect of general and regional anesthetics on the urinary system?
Signup and view all the answers
Which procedure may be necessary for a patient experiencing overflow incontinence due to urinary retention?
Which procedure may be necessary for a patient experiencing overflow incontinence due to urinary retention?
Signup and view all the answers
Which symptom would most likely be experienced by an alert patient with severe bladder distension?
Which symptom would most likely be experienced by an alert patient with severe bladder distension?
Signup and view all the answers
What is micturition?
What is micturition?
Signup and view all the answers
At what point does the urge to void typically begin for adults?
At what point does the urge to void typically begin for adults?
Signup and view all the answers
Which of the following alterations in urinary elimination causes involuntary leakage of urine?
Which of the following alterations in urinary elimination causes involuntary leakage of urine?
Signup and view all the answers
What condition is characterized by an accumulation of urine due to the inability of the bladder to empty?
What condition is characterized by an accumulation of urine due to the inability of the bladder to empty?
Signup and view all the answers
Why are patients with female genitalia more susceptible to urinary tract infections?
Why are patients with female genitalia more susceptible to urinary tract infections?
Signup and view all the answers
Which of the following can be a cause of urinary tract infections?
Which of the following can be a cause of urinary tract infections?
Signup and view all the answers
What is nocturia?
What is nocturia?
Signup and view all the answers
Which alteration in urinary elimination results from catheterization and may cause urinary tract infections?
Which alteration in urinary elimination results from catheterization and may cause urinary tract infections?
Signup and view all the answers
What is a primary reason for creating a urinary diversion?
What is a primary reason for creating a urinary diversion?
Signup and view all the answers
Which statement describes the ileal conduit accurately?
Which statement describes the ileal conduit accurately?
Signup and view all the answers
What is a characteristic of an incontinent urinary diversion?
What is a characteristic of an incontinent urinary diversion?
Signup and view all the answers
What is the primary function of the Indiana pouch?
What is the primary function of the Indiana pouch?
Signup and view all the answers
Which statement about the orthotopic neobladder is true?
Which statement about the orthotopic neobladder is true?
Signup and view all the answers
What is an ideal characteristic of a urinary stoma?
What is an ideal characteristic of a urinary stoma?
Signup and view all the answers
What complication can occur if urine consistently contacts the skin in incontinent urinary diversions?
What complication can occur if urine consistently contacts the skin in incontinent urinary diversions?
Signup and view all the answers
What differentiates a continent urinary diversion from an incontinent one?
What differentiates a continent urinary diversion from an incontinent one?
Signup and view all the answers
What is the typical odour of concentrated urine?
What is the typical odour of concentrated urine?
Signup and view all the answers
What does a sweet or fruity odour of urine indicate?
What does a sweet or fruity odour of urine indicate?
Signup and view all the answers
Which urine collection method involves discarding the first morning urine?
Which urine collection method involves discarding the first morning urine?
Signup and view all the answers
What abnormal finding in urinalysis may indicate a urinary tract infection?
What abnormal finding in urinalysis may indicate a urinary tract infection?
Signup and view all the answers
What is the normal pH range for urine?
What is the normal pH range for urine?
Signup and view all the answers
What does the presence of ketones in urine suggest?
What does the presence of ketones in urine suggest?
Signup and view all the answers
What is a potential cause of hematuria in urine analysis?
What is a potential cause of hematuria in urine analysis?
Signup and view all the answers
What does the presence of bilirubin in urine indicate?
What does the presence of bilirubin in urine indicate?
Signup and view all the answers
What is a common responsibility before a diagnostic examination?
What is a common responsibility before a diagnostic examination?
Signup and view all the answers
Which of the following is NOT a responsibility after a diagnostic procedure?
Which of the following is NOT a responsibility after a diagnostic procedure?
Signup and view all the answers
What is an important consideration when promoting normal micturition?
What is an important consideration when promoting normal micturition?
Signup and view all the answers
What does chronic kidney disease (CKD) involve?
What does chronic kidney disease (CKD) involve?
Signup and view all the answers
What is a key marker of kidney damage in chronic renal failure?
What is a key marker of kidney damage in chronic renal failure?
Signup and view all the answers
Which action is NOT appropriate for preventing urinary tract infections?
Which action is NOT appropriate for preventing urinary tract infections?
Signup and view all the answers
What is an effective method to promote complete bladder emptying?
What is an effective method to promote complete bladder emptying?
Signup and view all the answers
Which condition is characterized by pathological abnormalities in the kidneys?
Which condition is characterized by pathological abnormalities in the kidneys?
Signup and view all the answers
Study Notes
Micturition
- Complex neural response allowing the bladder to contract, the urethral sphincter to relax, and urine to leave the body.
Voiding Reflex
- Voluntary control over bladder emptying develops as a child matures.
- Adults typically feel the first urge to void when the bladder is half full.
Common Alterations in Urinary Elimination
- Urinary tract infections (UTIs): Involuntary leakage of urine.
- Urinary incontinence: An accumulation of urine due to the bladder's inability to empty.
- Nocturia: Waking in the night to urinate.
- Urinary retention: Commonly result from catheterization (CAUTI), may also be caused by hygiene.
- Urinary diversions: Diversion of urine to an external source.
Common Symptoms of Urinary Alterations
- Incontinence: Involuntary loss of urine
- Urgency: Sudden, compelling desire to urinate difficult to defer.
- Dysuria: Pain, burning, or discomfort during urination.
- Frequency: Voiding more than eight times in 24 hours.
- Hesitancy: Delay in initiating urination
- Polyuria: Notably larger urine excretion volume.
- Oliguria: Diminished urinary output relative to intake.
- Nocturia: Number of times urine is passed during the main sleep period.
- Dribbling: Leakage of urine despite voluntary control.
- Hematuria: Passage of visible blood mixed with urine
- Elevated postvoid residual urine: Volume of urine in bladder after emptying.
Urinary Tract Infections (UTIs)
- UTI involves the lower urinary tract causing cystitis, urethritis, and prostatitis in male patients.
- Patients with female genitalia are more susceptible to infection due to the short urethra
- Causes: obstruction of the urinary tract (e.g., benign prostatic hyperplasia, pelvic organ prolapse), incomplete bladder emptying, and abnormal anatomy.
- Risk factors: older adults, antibiotic use, progressive underlying disease, and decreased immunity.
- UTI can spread to the upper tract, causing kidney infection (pyelonephritis) and potentially long-term kidney damage.
- Bacteria can spread to the bloodstream (bacteremia) resulting in urosepsis
- Symptoms of lower UTIs: pain/burning sensation during urination (dysuria), fever, chills, nausea, vomiting, and malaise.
- Symptoms of upper UTIs: inflammation of the bladder causing a frequent/urgent need to void, incontinence, and confusion
Clinical Manifestations of UTIs
- Irritation to the bladder and urethral mucosa resulting in blood-tinged urine (hematuria).
- Cloudy, foul-smelling urine or a change in urine colour, in the absence of other symptoms, does not indicate infection.
- If the infection spreads to the upper urinary tract (i.e., the kidneys), rapid onset of flank or lower back pain, tenderness, fever, and chills can occur.
- Catheter-associated UTIs (CAUTIs): results in increased length of hospital stay, morbidity, and mortality for patients.
- Reduce unnecessary use of in-dwelling catheters and remove them as soon as clinically indicated; good perineal care is recommended.
Indications for Urinary Catheterization
- Post-operative or acute urinary retention
- Bladder outlet obstruction (e.g., gross hematuria, BPH, pelvic organ prolapse, urethral strictures)
- Need for accurate measurements of I&O
- Prolonged immobilization
- Continuous bladder irrigation (CBI)
- Administration of medications into the bladder (cancer)
- Improving comfort at the end of life
- Perioperative in selected surgical procedures.
Contraindications for Urinary Catheterization
- Perceived comfort in patients with urinary or fecal incontinence.
- Using a catheter to obtain urine for tests when patients can void voluntarily.
- Prolonged postoperative use without appropriate indications.
Urinary Incontinence
- Defined as a complaint of involuntary loss of urine.
- Often occurs with other lower urinary tract symptoms. (e.g., daytime frequency, nocturia, urgency, intermittent or slow stream, hesitancy, postmicturition symptoms)
- Psychosocial impact ranges from lifestyle changes to stigma, embarrassment, and self-imposed social isolation.
- Types include transient, urgency, stress, mixed, UI associated with chronic retention, functional, neurogenic
Nocturia
- Bothersome symptom defined as the need to get up at night on a regular basis to urinate.
- Prevalence increases with age.
- Possible causes: overactive bladder, prostate enlargement (men), excess urine production at night (nocturnal polyuria), heart failure, obstructive sleep apnea, loss of vasopressin.
- Associated with metabolic imbalances (hyperglycemia, hypercalcemia).
Urinary Retention
- Accumulation of urine in the bladder due to the bladder's inability to empty.
- Micturition reflex is impaired
- The build-up of urine causes pressure, discomfort, tenderness, restlessness, and diaphoresis.
- Possible causes: Post-partum, urogenital surgery, medication adverse effects (anticholinergic), fecal impaction, Post-operative urinary retention (POUR), Chronic urinary retention.
Safety Alert: Autonomic Dysreflexia
- Bladder distention can trigger autonomic dysreflexia in individuals with spinal cord injury above the T6 level.
- Dysregulation of the autonomic nervous system leads to uncoordinated autonomic response (potentially life-threatening hypertension).
- Immediate recognition and correction (e.g. irrigating or changing the Foley catheter) is critical.
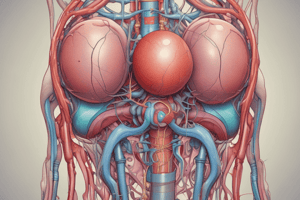
Urinary Diversion
- A urinary stoma to divert urine flow from the kidneys to the abdominal surface.
- Reasons for diversion include: bladder cancer, trauma, radiation injuries, fistulas, and chronic cystitis.
- Temporary or permanent.
- Patients require an ostomy appliance.
- Local irritation and skin breakdown are possible due to urine contact with skin.
GU Fistula
- Abnormal connection between the urinary and genital tracts.
Urinary Diversion Methods
-
Ileal Conduit: Loop of ileum separated with intact blood supply where ureters are implanted; remaining ileum reconnected
-
Orthotopic Neobladder: Internal pouch formed from the ileum and reconnected to the urethra
-
Indiana Pouch: Creates a continent internal pouch from the ileum; a portion is connected to the abdominal wall
-
Ideal urinary stoma are symmetrical, do not have skin breakdown and protrude about 1.5cm
Nursing Considerations: Urinary Elimination
- Infection control and hygiene: sterile urinary tract
- Catheter duration is most important risk factor for UTIs
- Medical and surgical asepsis during catheterization
- Growth and development: changes in kidney and bladder function with aging, less effective emptying, increased susceptibility to UTIs, and elevated postvoid residual volume.
- Psychological considerations: urinary problems can impact sexuality and self-concept, embarrassment, and self-isolation
- Cultural considerations: cultural needs around urinary function.
Assessment of Urine
- Color: Pale straw to amber (depending on concentration); dark red/bright red (kidney/bladder/urethra bleed); dark amber (bilirubin)
- Clarity: Transparent at voiding; cloudy if left standing/high protein/bacteria
- Odor: Characteristic; stronger with concentration; ammonia with stagnant urine; sweet/fruity (diabetes, starvation)
Urine Testing Collection Techniques:
- Clean-Catch Midstream: Patient cleans urethral area; begins urinating and collects midstream in sterile container.
- 24-hour urine collection: Urine collected over 24 hours, discarding first void, collecting remaining urine in provided container.
- Catheterized sample: Collected by healthcare professional directly from catheter.
Urinalysis
- Color, Clarity, Odor: Normal values. Changes in these can indicate problems
- pH (Acidity): Normal range (4.5-8). High pH may suggest infection or high-protein diet; low pH indicates high-protein diet or certain medications
- Protein: Normally absent or in small amounts. Proteinuria can indicate kidney disease or infection.
- Glucose: Absent. Glycosuria suggests high blood sugar levels (uncontrolled diabetes)
- Ketones: Absent. Ketonuria can indicate uncontrolled diabetes, starvation, or a low-carbohydrate diet.
- Leukocyte Esterase & Nitrites: Indicate infection
- Blood: Absent. Hematuria can indicate infection, trauma, or kidney stones
- Bilirubin & Urobilinogen: Absent. Bilirubin suggests liver or gallbladder disease
Diagnostic Examinations
- Noninvasive examination
- Invasive examination
Common Post-Procedure Interventions
- Assessing intake and output
- Observing characteristics of the urine, including color, clarity, and presence of blood
Health Promotion
- Promoting regular micturition: Use sensory stimuli to stimulate voiding reflex
- Maintaining elimination habits, adequate fluid intake promoting complete bladder emptying: double voiding/intermittent catheterization, bladder scanning
- Preventing infection: good perineal hygiene, hand washing, fluid intake, good quality perineal products.
- Use of urinary catheter requires prescript
- Incontinence alone is not reason to insert catheter
Class Learning Outcomes
- Compare common alterations in urinary elimination.
- Describe nursing implications of common diagnostic tests.
- Discuss nursing measures to prevent episodes of incontinence.
- Describe nursing and collaborative care for clients with chronic renal failure and chronic kidney disease.
- Describe indications for peritoneal and hemodialysis.
- Describe nursing care for clients undergoing peritoneal and hemodialysis.
Chronic Kidney Disease (CKD)
-
Progressive, irreversible loss of kidney function.
-
Chronic renal failure
-
Kidney damage: pathological abnormalities (nephron destruction), markers of damage (blood, urine, imaging tests)
-
Glomerular filtration rate (GFR) decline (<60 mL/minute/1.73 m²) for 3+ months.
-
80% GFR loss without significant body response
-
Compensatory mechanism: remaining nephrons increase in size (hypertrophy)
-
Leading causes of end-stage renal disease include diabetes mellitus, hypertension, renal vascular disease (affecting blood flow), renal artery stenosis/thrombosis, renal vein thrombosis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the complexities of micturition and urinary alterations in this quiz. Learn about the neurological responses involved in bladder control, common urinary issues like UTIs and incontinence, and their symptoms. Test your knowledge of urinary physiology and related disorders.