Podcast
Questions and Answers
Which HPV genotypes are responsible for approximately 70% of invasive cervical cancer cases worldwide?
Which HPV genotypes are responsible for approximately 70% of invasive cervical cancer cases worldwide?
- HPV types 1 and 2
- HPV 16 and 18 (correct)
- HPV types 3 and 4
- HPV 6 and 11
What is the primary risk factor for developing cervical intraepithelial neoplasia (CIN)?
What is the primary risk factor for developing cervical intraepithelial neoplasia (CIN)?
- Presence of warts
- Transitory HPV infections
- Age over 50 years
- Persistent infection with an oncogenic HPV type (correct)
Where does HPV replicate exclusively?
Where does HPV replicate exclusively?
- In the mucosal surface
- In stratified squamous epithelium (correct)
- In smooth muscle tissue
- In the bloodstream
What is a common clinical presentation of cutaneous warts caused by HPV?
What is a common clinical presentation of cutaneous warts caused by HPV?
What role do early non-structural viral proteins E6 and E7 play in HPV infection?
What role do early non-structural viral proteins E6 and E7 play in HPV infection?
What types of warts are primarily caused by HPV 6 and 11?
What types of warts are primarily caused by HPV 6 and 11?
How does HPV evade immune recognition in the epithelium?
How does HPV evade immune recognition in the epithelium?
What happens to the majority of HPV infections within 12–24 months?
What happens to the majority of HPV infections within 12–24 months?
Which of the following viruses is classified as a DNA tumor virus?
Which of the following viruses is classified as a DNA tumor virus?
What characterizes oncogenic viruses?
What characterizes oncogenic viruses?
Which proteins are associated with tumor-suppressor genes?
Which proteins are associated with tumor-suppressor genes?
Which HPV type is most commonly linked to cervical cancer?
Which HPV type is most commonly linked to cervical cancer?
What is the primary mode of transmission for high-risk HPV types?
What is the primary mode of transmission for high-risk HPV types?
Which of the following cell types gives rise to carcinoma?
Which of the following cell types gives rise to carcinoma?
What term describes the process normal cells undergo to become malignant?
What term describes the process normal cells undergo to become malignant?
What best describes the role of proto-oncogenes?
What best describes the role of proto-oncogenes?
Which term refers to the continuous proliferation of a clone of cells in cancer?
Which term refers to the continuous proliferation of a clone of cells in cancer?
What percentage of human cancers worldwide are estimated to have a viral etiology?
What percentage of human cancers worldwide are estimated to have a viral etiology?
Which area is most commonly affected by lesions associated with HPV infections?
Which area is most commonly affected by lesions associated with HPV infections?
What is the most common cause of laryngeal papillomatosis?
What is the most common cause of laryngeal papillomatosis?
Which statement is true regarding epidermodysplasia verruciformis?
Which statement is true regarding epidermodysplasia verruciformis?
How does HPV oncogenesis begin?
How does HPV oncogenesis begin?
Which factor increases the risk of HPV persistence and cervical cancer?
Which factor increases the risk of HPV persistence and cervical cancer?
What is an effective prevention method for cervical cancer?
What is an effective prevention method for cervical cancer?
What is the treatment focus for infants affected by laryngeal papillomatosis?
What is the treatment focus for infants affected by laryngeal papillomatosis?
What condition does a CD4 cell count of < 200 indicate in relation to HPV?
What condition does a CD4 cell count of < 200 indicate in relation to HPV?
What is the recommended age for females to receive the Cervarix vaccine?
What is the recommended age for females to receive the Cervarix vaccine?
Which HPV vaccine targets serotypes 6, 11, 16, and 18?
Which HPV vaccine targets serotypes 6, 11, 16, and 18?
Flashcards are hidden until you start studying
Study Notes
HPV and Cervical Cancer
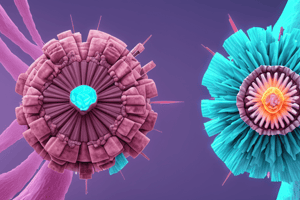
- Human Papillomavirus (HPV) is a non-enveloped, double-stranded DNA virus with over 200 types.
- HPV is sexually transmitted and can also be transmitted in utero or perinatally.
- About 15 HPV types are linked to cancer.
- High-risk (hr) types are associated with malignancy, particularly HPV 16 and 18.
- Low-risk types are associated with warts.
- hrHPV 16 and 18 are responsible for ~90% of anal cancers, ~70% of all cervical cancer cases and oropharyngeal tumors, and ~40% of penile, vulvar, and vaginal cancers.
- hrHPV 31, 33, 45, 52, and 58 also contribute to cancers, but to a lesser extent.
HPV Replication
- HPV replicates exclusively in stratified squamous epithelium, requiring differentiating epithelium for a complete cycle.
- HPV enters basal epithelial cells through micro-abrasions.
- Early non-structural viral proteins (E6 and E7) are expressed in the basal layer.
- These proteins stimulate infected cells to proliferate faster and replicate the viral genome.
- As epithelial cells mature and move up the epithelial layer, the virus's structural genes (L1 and L2) are expressed.
- Structural viral proteins are produced, new virus particles assemble, and the virus is shed as infected cells desquamate.
- Epithelium is an immune-privileged site, allowing the virus to evade immune recognition and persist for months or years.
HPV and Oncogenesis
- HPV DNA can integrate into host chromosomes.
- Viral proteins (E6 and E7) interfere with cell cycle control.
- E6 binds to p53, a tumor suppressor gene, and E7 binds to pRb, another tumor suppressor.
- The integration of HPV DNA can activate c-myc, leading to uncontrolled cell growth.
HPV and STIs
- HIV infection is associated with increased HPV persistence and the development of cervical intraepithelial lesions (CIN).
- HIV-infected females with a CD4 cell count below 200 have a seven-fold increased incidence of cervical cancer.
- Antiretroviral therapy (ART) can reduce HPV persistence and allow for clearance of the virus.
- HSV 1 and 2 infection allows for better access to the basal cell layer, potentially leading to increased persistence and oncogenic activity of HPV.
HPV and Cervical Cancer
- Most HPV infections are transient and become undetectable in 12-24 months.
- Persistent HPV infection with an oncogenic type is a major risk factor for CIN progression to cancer.
Clinical Spectrum of HPV Infection
- Most HPV infections are clinically silent.
- A small minority of individuals develop clinically apparent lesions, such as warts.
- Cutaneous warts are caused by HPV types 1, 2, 3, 4, 5, and 8.
- Mucosal warts are mainly caused by HPV types 6 and 11.
- Laryngeal papillomatosis (warts in the larynx) is commonly seen in infants and young children, usually acquired during passage through the birth canal.
- Epidermodysplasia verruciformis is a rare condition caused by mutations in the EVER1 or EVER2 genes, leading to a defect in cell-mediated immunity and high HPV susceptibility.
Prevention of Cervical Cancer
- Vaccination: Cervarix (serotypes 6 and 11) and Gardasil 4 (serotypes 6, 11, 16, and 18).
- Behavior change: Limiting high-risk exposure.
- Treatment of HIV and other STIs.
- Cervical cytology screening: Reduces the incidence of cervical cancer by 70%.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.